Zygomatic maxillary complex (ZMC) fractures
Updated May 2024
Karen Brown, MD; Makayla McCoskey, MD; Vikram Durairaj, MD
Establishing the diagnosis
Etiology
- The zygomaticomaxillary complex (ZMC) includes the zygomatic bone and the suture lines with the four adjacent bones: the maxillary, frontal, sphenoid, and temporal bones. The suture lines include the zygomaticomaxillary (ZM), zygomaticofrontal (ZF), zygomaticosphenoid (ZS), and the zygomaticotemporal (ZT). Force applied to the zygoma is often transmitted along the respective zygomatic processes.
- The zygomatic bone makes up part of the lateral orbital wall and orbital floor. Fracture of the zygoma commonly involves fracture of the orbital floor and/or lateral orbital wall.
- The zygomatic bone provides anterior and lateral projection of the midface and contributes to the vertical and horizontal buttresses of the facial skeleton. The zygomaticomaxillary buttress is the vertical buttress that extends from the lateral maxilla through the zygoma at the lateral rim, through the frontal process of the zygoma, and then then zygomatic process of the frontal bone. This vertical buttress provides important support for mastication. The horizontal buttress includes the zygomatic arch and inferior orbital rim gives bony stability to the face (Funk).
- As a result, displaced ZMC fractures can cause midface deprojection due to disruption of the horizontal buttress. Fracture of the zygomatic arch can result in trismus if the fracture is depressed to the extent where it injures the temporalis muscle or interferes with forward movement of the coronoid process of the mandible.
Epidemiology
- ZMC fractures are more common in men and result from blunt trauma, such as sports related injury, falls, and motor vehicle collisions.
History
- Time course: The ideal window of time for repair is 1-2 weeks. Fractures older than 3 weeks become more difficult to repair due to healed bone and may require osteotomies to refracture the bone to allow for anatomic reduction.
Clinical features
- Diplopia, if present, can be due to one or more causes:
- Entrapment
- Edema causing restricted motility
- Oculomotor nerve damage (rare)
- Infraorbital nerve hypoesthesia
- Trismus due to medially or posteriorly displaced ZMC causing restriction of the coronoid process
- Facial asymmetry due to horizontal widening and malar depression
Exam
- Each patient should undergo a full ophthalmologic exam, including a pupil exam to assess for traumatic optic neuropathy and a dilated fundus exam to assess for ocular trauma.
- If concern for retrobulbar hemorrhage causing ocular compartment syndrome, emergent lateral canthotomy and cantholysis is necessary.
- Evaluate position of the lateral canthal ligament. Vertical displacement of the zygoma may result in vertical displacement of the lateral canthus and canthal dystopia, hypoglobus (Marwan)
- Presence of a supratarsal sulcus deformity suggests enophthalmos due to orbital floor fracture
- Extraocular motility testing
- Forced duction exam is warranted if gaze restriction is present to differentiate entrapment (restriction) vs. paresis/nerve pathology
- V2 sensory exam
- Palpation of orbital rim and ZMC for step-offs, crepitus, hematoma
- Bird’s-eye or worm’s-eye view to assess malar prominence, which is normally 1cm lateral to and 2cm inferior to the lateral canthus and often displaced posteriorly and rotated medially in ZMC fractures
Radiographic findings
- ZMC fractures are best assessed with a non-contrast maxillofacial computed tomography (CT) axial and coronal imaging with 1.5mm cuts
- Review from caudal to rostral on the axial view will demonstrate a fracture along the ZS process, then the ZT process, then the ZM process (Figure 3).
- Review from anterior to posterior on the coronal will demonstrate a ZM fracture, the ZF fracture, and orbital floor fracture (Figure 4)
- The sagittal view is helpful to discern the anterior-posterior extent of the orbital floor fracture
- Soft tissue window is useful if there is concern for an orbital hematoma.
A. 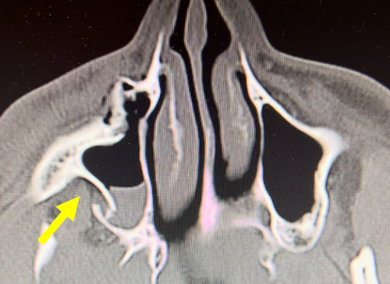 B.
B. 
Figure 3. Axial orbital CT demonstrating a fracture at the ZM suture (A) and ZS suture (B).
A. 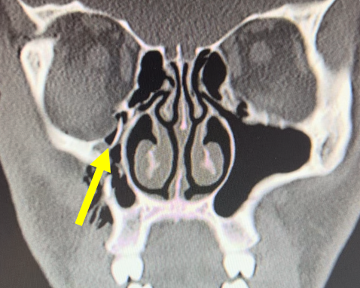 B.
B. 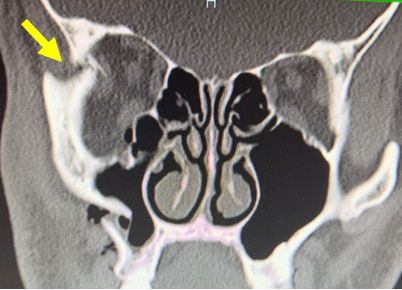
Figure 4. Coronal orbital CT demonstrating a fracture of the orbital floor (A) and ZF suture (B).
- Zingg Classification System, proposed by Zingg et al in 1992
- Type A: an incomplete zygomatic fracture involving a single ZMC structure
- A1: Zygomatic arch fracture
- A2: Lateral orbital wall fracture
- A3: Infraorbital rim fracture
- Type B: complete tetrapod fracture, with the zygoma remaining intact (noncomminuted)
- Type C: multi-fragment zygomatic fracture, with complete tetrapod fracture as well as a comminuted zygomatic body fracture
Patient management: treatment and follow-up
Natural history
- The natural course of fracture repair involves an inflammatory hematoma phase within the first five days. This is followed by hard callus formation via endochondral ossification over the course of 1-6 weeks after injury. This is then followed by the remodeling phase which is a slow process mediated by the balanced action of osteoblasts and osteoclasts that lasts months to years after injury. (Bigham-Sadeg)
Medical therapy
- Minimally displaced ZMC fractures without associated functional deficits (i.e. extraocular muscle entrapment, hypoglobus, trismus) or aesthetic concerns (i.e. malar deprojection, enophthalmos) may be appropriate for nonsurgical management.
- Data regarding the utility and safety of preoperative and/or perioperative steroids is inconclusive. A prospective study of 64 patients undergoing open reduction and internal fixation of ZMC fractures found a significantly increased risk of surgical wound healing complications in patients receiving 10mg or 30mg of dexamethasone perioperatively (Snall et al). Conversely, a retrospective review of 100 patients receiving perioperative dexamathasone (10mg every 8 hours x 3 doses) did not find a statistically significant difference in perioperative wound healing compared to controls (Thoren et al).
- Nonoperative fractures do not routinely require antibiotics.
- A single dose of preoperative (within 3 hours of surgery) or intraoperative antibiotics is standard for operative ZMC fractures. The antibiotic choice should cover oral and respiratory flora given the involvement of the fracture with the paranasal sinuses. Cefazolin (Ancef) is the common choice for intraoperative prophylaxis, with alternatives including ampicillin-sulbactam (Unasyn) or clindamycin. Postoperative antibiotics are not routinely recommended. (Mundinger)
Surgery
- Surgical emergencies: extraocular muscle entrapment, orbital compartment syndrome/retrobulbar hemorrhage
- Other indications for surgery: 1) functional impairment – i.e. trismus/impaired mouth opening, enophthalmos, significant diplopia 2) cosmetic deformity – i.e. malar prominence depression, facial contour irregularity
- Timing of surgery: patients demonstrating extraocular muscle entrapment require immediate surgery to free the entrapped muscle and prevent associated long-term complications, including muscle necrosis, permanent motility deficits, and prevent acute complications related to the oculocardiac reflex; in the absence of indications for emergent intervention, timing of surgery is at the discretion of the individual surgeon. Generally, repair is best performed within 1-2 weeks, after the initial edema has begun to settle, but prior to onset of significant fibrosis and scarring.
- Surgical approach is guided by the type of fracture (ie. Zingg Classification) and the stability of the ZMC after reduction, which determines the necessity and type of fixation.
- Surgical treatment algorithm by Zingg Class (Marinho et al 2013 https://pubmed.ncbi.nlm.nih.gov/24055372/):
- Class A1 (zygomatic arch fracture): Displaced zygomatic arch fractures can often be reduced without requiring fixation; this can be performed in a closed approach using a transcutaneous towel clamp or bone hook, or with an open surgical approach, such as a Gillies temporal incision or an intraoral incision. In cases of instability after fixation, external stabilization can be performed with an external splint sutured transcutaneously; alternatively, for more complex unstable arch fractures, a coronal approach may be required to allow access for internal plate fixation.
- Class A2 (lateral orbital wall fracture): Isolated lateral orbital wall fractures can be accessed and reduced via a lateral upper eyelid lid crease incision. Fixation with mini-plates generally provides adequate stabilization.
- Class A3 (Infraorbital rim fracture): Access to the infraorbital rim can be achieved through a lower eyelid transconjunctival incision. This approach also allows access to the orbital floor, which is often also involved in fractures of the infraorbital rim. Low profile plates can be used to fixate these fractures.
- Class B (tetrapod fracture): Most Class B fractures demonstrate some degree of instability, and thus require open reduction and internal fixation. The degree of instability determines the number of points of fixation. Many Class B fractures require only one or two points of fixation at the zygomaticomaxillary buttress via a transoral incision and/or at the frontozygomatic suture via an eyelid crease incision. In fractures with remaining instability, the infraorbital rim (via transconjunctival incision) or the zygomatic arch (via coronal approach) can also be plated to provide further fixation.
- Class C (comminuted fracture): All Class C fractures require open reduction and internal fixation. The approach is similar to Class B fractures, and generally multiple access sites are required for fixation in multiple locations to provide adequate stabilization.
- Orbital floor involvement: Fractures of the orbital floor frequently accompany ZMC fractures, particularly those involving injury to the infraorbital rim. Not all orbital floor fractures require exploration or repair, however. See the article on orbital floor fractures for additional information (https://asoprseducation.org/orbital-floor-fractures/)
- Types of plates: Titanium miniplates and screws are generally used for fixation in facial fractures, providing stable fixation with few complications. Various plate sizes and shapes are available. The use of bioresorbable fixation systems remains controversial.
Other considerations
- Late repair: Delayed surgical intervention, typically after 2 weeks, is possible but becomes increasingly challenging with time as bony callous and scar tissue forms. Beyond 6 weeks after the injury, surgical intervention may require more open approaches and intraoperative imaging/navigation to facilitate fracture reduction.
Preventing and managing treatment complications
Postoperative infection
- Single-dose intraoperative antibiotics covering oral and respiratory flora (i.e. cefazolin) is standard to minimize postoperative infection.
- The routine use of postoperative antibiotics is variable among providers (Reiss) and evidence to support routine postoperative antibiotic prophylaxis is lacking.
Postoperative vision loss
- Monitor for the development of postoperative hematoma in the immediate postoperative period. If there is concern for hematoma development with orbital compartment syndrome, urgent return to the operating room for exploration is warranted.
- Minimize compression on the globe from tissue retraction during surgery.
- Size any orbital implant precisely with care to fixate the implant without inducing posterior elevation of the implant which could compress the optic nerve.
Wound healing complications
- There is typically minimal tension on the skin incisions created for access to the fracture sites.
- Closure of intraoral incisions with chromic gut suture may aid in healing. Encourage a soft diet in the early postoperative period to avoid food particles entering the wound. Use of an oral rinse such as chlorhexidine gluconate 0.12% (Peridex) postoperatively helps keep the intraoral incision clean as it heals.
- There is conflicting data regarding the potential negative effect of perioperative steroids on wound healing (Snall, Thoren).
Implant extrusion
- Implant extrusion can occur in the setting of infection, poor placement/fitting or fixation or inadequate soft tissue coverage of the implant.
- Size the implant carefully and avoid oversizing.
- Fixate the implant to adjacent stable bone. When plating orbital floor fractures, this may require use of a plate along the orbital rim if there is a comminuted orbital rim fracture.
- Close the periosteum over hardware to provide soft tissue coverage and minimize risk of implant exposure.
- If there is concern for infection, antibiotics are necessary and implant removal should be considered.
Diplopia and extraocular muscle limitation
- Perform forced ductions preoperatively and after placement of an orbital implant. Forced ductions should be free after implant placement. If there is restriction with forced ductions, this suggests there is muscle entrapment in the fracture due to implant malposition.
- Diplopia may worsen in the immediate postoperative period due to swelling and/or paresis of the inferior rectus or oblique muscles in ZMC fractures involving the orbital floor. This is expected to improve with healing. Patients with diplopia persisting months after surgery should be referred to a strabismologist for evaluation of surgical repair. Strabismus surgery should only be considered if motility and diplopia remain stable for at least 6 months.
Hypesthesia/dysesthesia
- Infraorbital nerve dysfunction can occur with fracture involvement of the infraorbital nerve canal or with edema surrounding the nerve. This may temporarily worsen after surgery due to postoperative edema. This may take up to 18 months to resolve following injury or surgery.
- If there is persistent infraorbital nerve pain postoperatively, this may indicate nerve impingement from an implant and imagining should be obtained to assess for implant malposition.
Eyelid malposition
- Retraction and/or entropion is more likely with transcutaneous approach or orbital floor and ZMC fracture repair. Transconjunctival approach should be used whenever possible.
- Swinging eyelid approach with lateral canthotomy cantholysis may be required for adequate visualization of large orbital floor and ZMC fractures. Care should be taken to properly reform the lateral canthus with closure.
- Adequate soft tissue coverage of an orbital rim implant with periosteum is important to prevent scarring of the orbicularis to the orbital rim and consequent retraction. In the event of eyelid retraction and tethering to the rim, this may require surgical repair via release of scar tissue +/- free mucosal graft (i.e. conjunctiva, hard palate, buccal mucosa) or allogeneic material (i.e. Alloderm, Tutoplast).
Disease-related complications
The following complications can occur with or without surgical intervention:
- Globe injury
- Extraocular muscle entrapment or other injury
- Enophthalmos (particularly in fractures involving the orbital floor)
- Infraorbital sensory nerve injury with hypesthesia
- Facial nerve injury and possible facial paralysis
- Facial deformity, specifically loss of malar projection
- Trismus (inability to fully open the mouth) due to compression of the zygomatic arch on the temporalis muscle and coronoid process of the mandible
- Hardware problems, including infection and exposure
- Sinusitis
- Scarring and soft tissue distortion
References and additional resources
- Bigham‐Sadegh A, Oryan A. Basic concepts regarding fracture healing and the current options and future directions in managing bone fractures. International Wound Journal. 2015;12(3):238-247. doi:10.1111/iwj.12231
- Huang W, Lynham A, Wullschleger M. Orbitozygomatic Fracture Repairs: Are Antibiotics Necessary? Craniomaxillofacial Trauma & Reconstruction. 2015;8(4):271-276. doi:10.1055/s-0034-1399795
- Marinho ROM, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin North Am. 2013;25(4):617-636. doi:10.1016/j.coms.2013.07.011
- Marwan H SY, Sawatari Y, Peleg M. Management of Orbito-Zygomaticomaxillary Fractures. 1st edition. Springer International Publishing; 2021.
- Mundinger GS, Borsuk DE, Okhah Z, et al. Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice. Craniomaxillofacial Trauma & Reconstruction. 2015;8(1):64-78. doi:10.1055/s-0034-1378187
- Reiss B, Rajjoub L, Mansour T, Chen T, Mumtaz A. Antibiotic Prophylaxis in Orbital Fractures. TOOPHTJ. 2017;11(1):11-16. doi:10.2174/1874364101711010011
- Snäll J, Kormi E, Koivusalo AM, et al. Effects of perioperatively administered dexamethasone on surgical wound healing in patients undergoing surgery for zygomatic fracture: a prospective study. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2014;117(6):685-689. doi:10.1016/j.oooo.2014.02.033
- Thorén H, Snäll J, Kormi E, et al. Does Perioperative Glucocorticosteroid Treatment Correlate With Disturbance in Surgical Wound Healing After Treatment of Facial Fractures? A Retrospective Study. Journal of Oral and Maxillofacial Surgery. 2009;67(9):1884-1888. doi:10.1016/j.joms.2009.04.089
- Zingg M, Laedrach K, Chen J, et al. Classification and treatment of zygomatic fractures: a review of 1,025 cases. J Oral Maxillofac Surg. 1992;50(8):778-790. doi:10.1016/0278-2391(92)90266-3
