Dermoid Cysts
Updated May 2024
Suzanne K. Freitag, MD; Lora R. Dagi Glass, MD
Establishing the diagnosis
Etiology
- Congenital, choristoma
- Ectodermal nests pinched off from neural tube adjacent to suture lines of orbital or other cranial bones
- Classic epidermal dermoid cyst is lined by keratinizing stratified squamous epithelium with dermal tissue containing skin appendages including hair follicles and sebaceous and sweat glands (Figure 1).
- Rare reports of squamous cell carcinoma of cyst lining (Ahuja, Semin Ophthalmol, 2006)
- Less common conjunctival dermoid cyst is lined by nonkeratinizing squamous epithelium, with goblet cells in addition to dermal appendages
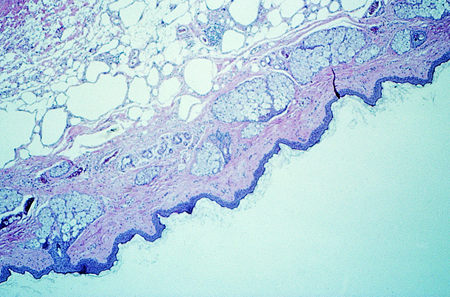
Figure 1. High power photomicrograph of dermoid cyst wall showing sebaceous glands.
Epidemiology
- Greater than 80% of dermoids are found in the head, and majority of those are periocular (Shields, Surv Ophthalmol, 2004)
- Might represent between 2% and 14% of all orbital tumors (Bonavolontà, Ophthal Plast Reconstr Surg, 2013; also, Shields, Ophthalmology, 2004)
- If rim site is counted, likely most common pediatric orbital tumor (Shields, Surv Ophthalmol, 2004)
- Most common cystic orbital lesion (Shields, Surv Ophthalmol, 2004)
History
- Typically presents as a slowly progressive mass in superotemporal or superomedial orbital quadrant (Figure 2)
- Visible at or near birth
- Slowly enlarges as the child grows
- Acute rupture may result in intense periorbital inflammatory reaction that mimics orbital cellulitis

Figure 2. External photograph showing clinical appearance of dermoid cyst present along frontozygomatic suture in a child.
Clinical features
- Divided into superficial and deep
- Superficial is usually recognized in childhood, often in the first few months of life. Small, subcutaneous, nontender, well-circumscribed, firm mass; sometimes mobile, sometimes adherent to periosteum
- Most commonly seen at the superolateral orbital rim (frontozygomatic suture)
- Second most common location is superomedial orbital rim.
- Must be careful to differentiate from meningoencephalocele, thus these are typically imaged preoperatively.
- Occasionally present with rupture and acute inflammation or as sinus tract with drainage
- Deep is rarer, presenting later in life (teenage years or older) with globe displacement or as in incidental radiographic finding.
- Usual presentation is globe displacement due to a large mass.
- Long duration can gradually erode bone.
- Soft tissue locations including lateral rectus muscle, lacrimal gland have been reported.
- Quantitative analysis of an incidentally noted deep dermoid in a young child did show significant growth, though not clinically overt (Hou, J AAPOS, 2012).
- Rarely, the lesion might involve both the superficial and orbital sides of the bone, resulting in what is described as a dumbbell configuration.
Testing
Indications for imaging
- Atypical lesion
- Atypical location, deep adherence require imaging
- Confirm diagnosis
- Rule out intracranial or intraorbital dumbbell component
- Discuss typical lesions with parents to make a joint decision. Not scanning will avoid sedation.
- Less sedation for shorter CT duration compared to MRI, but radiation exposure with CT
- Consider ultrasound.
CT scan
- Round, smooth borders, well-circumscribed mass
- Enhancing wall, nonenhancing center
- Bony erosion confirms long-standing nature of lesion
- Adjacent bone changes may be seen in 85% of cases (Chawda, Clin Radiol, 1999)
- Useful for identifying dumbbell extension on other side of bone
- Rarely, bone erosion may progress through lateral orbital wall, so dermoid takes on hourglass shape
- Bone erosion does not usually require treatment in these cases
- More rarely, bone erosion may progress intracranially
- Lucent center due to fat content. Layering of contents can occur
- Internal calcification may be seen in 14% of cases (Chawda, Clin Radiol, 1999)
- Useful for demonstrating bony details
MRI also useful
- Fat-suppressed view
- Fat density of cyst content helpful in making diagnosis
- Intra-cyst signal intensity variable
- Unlike CT, does not show bone detail
- Might be preferred to CT to avoid radiation exposure to children
- Image acquisition time is longer than CT, however, so requires longer sedation time in small children
Ultrasound
- Differentiate simple versus complex cyst structure
- Differentiate varying tissue densities
- No radiation, no sedation
Risk factors
- Congenital developmental abnormality with no known risk factors
Differential diagnosis
Dermoid cyst
- Lacrimal gland cyst
- Lacrimal gland tumor
- Meningoencephalocele (medial)
- Infantile Capillary Hemangioma (medial)
- Neoplasm
- Foreign body
- Mucocele
- Teratomatous cyst
- Frontal osteoma
- Aneurysmal bone cyst
- Lymphangioma
Ruptured dermoid
- Orbital cellulitis
- Abscess parasitic cyst
- Idiopathic orbital inflammation
Patient management: treatment and follow-up
Natural history
- Lesions grow slowly, often in proportion to the growth of the child.
- If anterior, can become fairly noticeable by teenage years
- Even minor trauma can result in cyst rupture with release of contents into orbit with secondary acute inflammation.
- Therefore, excision is often recommended after age 1.
- Patients presenting with a ruptured dermoid cyst with a significant inflammatory reaction might be treated with systemic corticosteroids — 1 mg/kg of PO prednisone or equivalent — and might benefit from surgery to remove cyst wall fragments after the inflammation has quieted.
- Timing is individualized; clinical exam should demonstrate complete resolution of inflammatory process, which might take weeks.
Surgery
- Surgical resection: Lesion should be kept intact to avoid spillage of contents into orbit, which can cause inflammation.
- Incision choice based on location
- Superior lid crease
- Lateral approach including lateral orbital rim
- Subconjunctival
- Around brow — take care not to disturb brow follicles.
- Over belly of cyst
- Controlled dissection key
- Maintain view with hemostasis and blunt-instrument retraction using Desmarres, malleable, etc.
- Blunt dissection ideal
- Cryotherapy can help close small cyst wall lacerations and allow for safer cyst maneuverability.
- In case of inadvertent cyst rupture, have a large suction and ample saline available for immediate suction of contents and flushing of operative site.
- Controlled decompression can be helpful for larger lesions, but it’s important to remove all the cyst wall.
- Usually adherent to frontozygomatic suture line; less frequently adherent to the suture line between the frontal bone and the frontal process of the maxillary bone
- Might require removal of periosteum at area of adherence to decrease risk of recurrence
- Deep orbital lesions or orbital components of dumbbell lesions usually involve upper temporal orbit; lateral orbitotomy with bone window might be required for exposure.
- For better visualization, methylene blue can be injected into lesion.
- Dumbbell lesions can be excised in 2 pieces — first extraorbital component, then orbital — but a modified lateral wall removal anterior to the intra-extra-orbital connection might allow for en bloc removal (Yuen, Ophthal Plast Reconstr Surg, 2004).
- For intracranial extension or deep apical lesion, joint neurosurgical case might be required.
- Both orbital and intracranially extending dermoids have been treated with percutaneous drainage and ablation (Golden, J AAPOS, 2007).
- No need for ongoing follow-up after complete resection, but percutaneous drainage/ablation likely should have ongoing follow-up until methodology is proven over years.
Preventing and managing treatment complications
- If cyst rupture with orbital inflammation occurs, copious irrigation at time of surgery
- Consider intraoperative and/or postoperative steroid or nonsteroid anti-inflammatory medications.
- Steroid dosing is weight based, generally 1 mg/kg of oral prednisone or its equivalent.
- Individualized taper, usually over 3 weeks
- Remind family to inform treating physicians of steroid use should child become ill.
- Steroid can also be intraoperatively irrigated within the surgical cavity to avoid systemic effects.
- Injury to adjacent orbital structures
- Lateral rectus (lateral lesions), superior oblique (medial lesions) or other extraocular muscle complete or partial palsy
- Ciliary ganglion damage
- Optic nerve damage
- Orbital hemorrhage
- Orbital infection
- Recurrence of lesion, if excision incomplete: carefully, completely re-excise
Disease-related complications
- Traumatic rupture leading to acute and chronic inflammation
- Rarely, intracranial extension from erosion of bone in long-standing lesion
- Visible or palpable permanent bone deformities from long-standing lesion with bone erosion
Patient instructions
Surgical resection recommended because of continued growth and risk of rupture
References and additional resources
- AAO, Basic and Clinical Science Course. Section 2: Fundamentals and Principles of Ophthalmology; Section 4: Ophthalmic Pathology and Intraocular Tumors; Section 6: Pediatric Ophthalmology and Strabismus; Section 7: Orbit, Eyelids, and Lacrimal system; Section 8: External Disease and Cornea, 2013-2014.
- AAO, Focal Points: Orbital Tumors in Children, Module #9, 1990, p.2.
- Ahuja R, Azar NF. Orbital dermoids in children. Semin Ophthalmol. 2006;21(3):207-11.
- Bonavolontà G, Strianese D, Grassi P, et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthal Plast Reconstr Surg. 2013;29(2):79-86.
- Chawda SJ, Moseley IF. Computed tomography of orbital dermoids: a 20-year review. Clin Radiol. 1999;54(12):821-5.
- Golden RP, Shiels WE 2nd, Cahill KV, Rogers GL. Percutaneous drainage and ablation of orbital dermoid cysts. J AAPOS. 2007;11(5):438-42.
- Hou JH, Aakalu VK, Setabutr P. Quantitative characterization of growth rate of an incidental deep dermoid cyst in a child using sequential magnetic resonance imaging. J AAPOS. 2012;16(4): 403-5.
- Kiratli H, Bilgic S, Sahin A, Tezel CG. Dermoid cyst of the lacrimal gland. Orbit. 2005;24(2):145-8.
- Shields JA, Shields CL. Orbital cysts of childhood – classification, clinical features, and management. Surv Ophthalmol. 2004;49(3):281-99.
- Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. Ophthalmology. 2004;111(5)997-1008.
- Tannan A, Jhaveri M, Moftakhar R, et al. Compressive optic neuropathy secondary to a lateral rectus muscle dermoid cyst. Ophthal Plast Reconstr Surg. 2015;31(3):e63-4.
- Yuen HKL, Chong YH, Chan SK, et al. Modified lateral orbitotomy for intact removal of orbital dumbbell dermoid cyst. Ophthal Plast Reconstr Surg. 2004;20(4): 327-9.
