Erysipelas
Updated July 2025
Alexis Kassotis and Lora R. Dagi Glass, MD
Establishing the diagnosis
Etiology
- Erysipelas is a cutaneous infection classically caused by beta-hemolytic streptococcus species. It is distinct from cellulitis in that it is more superficial.
- Up to 67% of cases are caused by Streptococcus pyogenes (Bonnetblanc, 2003).
- Streptococcus agalactiae (Group B Streptococcus) is the most common cause in neonates.
- Erysipelas can rarely be caused by non-Streptococcal species including Staphylococcus aureus (methicillin resistant or methicillin sensitive), Pseudomonas aeruginosa and Clostridium spp.
- Acutely, there is significant infiltration of neutrophils into the dermis and to a lesser extent the hypodermis.
- Infiltration of neutrophils and macrophages into the lymphatics can occur, causing lymphatic dilation.
Epidemiology
- Incidence has not been well established as cellulitis and erysipelas are not always easily differentiated. Additionally, most epidemiologic studies are done in hospitals and only include severely ill patients.
- The combined incidence of cellulitis and erysipelas is approximately 20 per 10,000 European individuals (Bartholomeeusen, 2007).
- The average age of onset is in the 5th decade of life.
- There is some evidence that incidence is rising in young children and individuals over 75 years of age (Bartholomeeusen, 2007 & Stulberg, 2002)
Risk factors
- Loss of skin integrity:
- Trauma (i.e. insect sting, abrasion)
- Surgical wounds or prior radiation
- Underlying dermatologic disease:
- Dermatophytosis was found to be a significant predisposing factor for erysipelas in the primary care setting in individuals aged 45-64 (Bartholomeeusen, 2007).
- Psoriasis
- Eczema
- Previous skin infection
- Venous insufficiency with ulceration
- Lymphedema
- Nephrotic syndrome
- Pregnancy
- Nasopharyngeal infection
- Immunocompromised states:
- Diabetes mellitus
- Obesity
- Alcoholism
- Human immunodeficiency virus (HIV)
- Transplant recipients
History
- Individuals may experience a prodrome of fevers, chills, malaise, nausea and/or vomiting.
Clinical features
- The most common location is the leg.
- Facial erysipelas accounts for approximately 6% of cases, making the face the second most commonly affected site (Lazzarini, 2005).
- Facial erysipelas often appears in a malar distribution (involving the cheeks and nasal bridge)
- Erysipelas presents as the acute onset of a bright red rash with a sharply demarcated, raised border (Figure 1).
- Other features that are sometimes present include:
- Edema, warmth, firmness and tenderness
- Fine dimples on the affected region (similar to the skin of an orange)
- Regional lymphadenopathy and/or lymphangitis
- Pustules and/or bullae
- Purpura due to bleeding into the skin
Other diagnostic studies
- The Infectious Disease Society of America does not recommend routine bacteriological skin culture as sensitivity is low (41%).
- Blood cultures should be obtained if signs of toxicity are present or if the patient is immunosuppressed.
- Other serologic findings that support the diagnosis (but are not routinely required) include: complete blood count with differential showing leukocytosis with neutrophilia, elevated levels of procalcitonin, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Though CRP and ESR are only elevated in approximately 50% of cases, elevated inflammatory markers are predictive of more severe disease (Lazzarini, 2005).
- A recent prospective study found that nearly 50% of patients with erysipelas were colonized with beta-hemolytic streptococcus species in the perianal area, making perianal culture a potential new diagnostic method (Trell, 2019).
Differential diagnosis
- Deeper skin infections:
- Preseptal cellulitis
- Necrotizing fasciitis
- Herpes zoster ophthalmicus
- Herpes simplex infection
- Malar rash (systemic lupus erythematous)
- Dermatomyositis
Patient management: treatment and follow-up
- Medical therapy (Infectious Disease Society of America, 2014):
- Erysipelas is treated by empirically covering beta-hemolytic streptococcus species as they are the overwhelmingly most common inciting organism.
- Outpatient management with empiric oral penicillin V potassium for five days is used for mild disease.
- If patients have systemic symptoms, inpatient management with IV penicillin is preferred.
- Macrolides, cephalosporins, and fluoroquinolones have also shown efficacy, but are costlier.
- A systematic review including 43 studies did not find any of the above antibiotics to be more efficacious than another. This review also found a five-day course of treatment to be equally as effective as a longer course of treatment (Brindle, 2019).
- In severe cases unresponsive to initial treatment, other organisms should be suspected and antibiotics should be broadened to vancomycin plus piperacillin/tazobactam.
- Surgical therapy: surgical debridement is only required in severe, necrotizing disease.
- Prognosis: lesions typically resolve completely over 1-2 weeks without scarring.
Complications
- Ocular complications (rare):
- Endogenous endophthalmitis due to hematogenous spread of Streptococcus pyogenes infection has been reported in the literature (Costa, 2015).
- Chronic periocular lymphedema.
- This mostly occurs with recurrent disease as lymphatic drainage becomes permanently impaired.
- Although this is a rare complication, a case report demonstrated improvement of periocular lymphedema, without intervention, over several months (Buckland, 2006).
- Other complications
- Abscess formation
- Focal necrosis
- Bacteremia
- Blood cultures return positive in less than 5% of cases (Bonnetblanc, 2003).
- Infections at distant sites (i.e. infective endocarditis)
- Post-streptococcal glomerulonephritis
- Cavernous sinus thrombosis
- Streptococcal toxic shock syndrome
- Deep vein thrombophlebitits
- Occurs in less than 5% of cases (Bonnetblanc, 2003).
- Compartment syndrome
- Usually related to infection with Clostridium spp.
- Can compromise the airway and circulation if the large vessels of the neck are involved.
- 3-year recurrence rates are up to 30% in patients hospitalized for severe disease and approximately 16% in the those who receive outpatient treatment for mild to moderate disease (Bartholomeeusen, 2007).
- High recurrence rates may be caused by the persistence of toxins in lymphatic channels due to impaired lymphatic drainage.
- Long term penicillin prophylaxis can be considered in these cases.
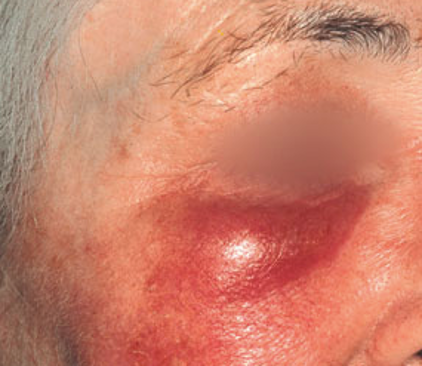
Photograph courtesy of D@nderm Atlas of Clinical Dermatology.
Figure 1. Erysipelas presenting as an intensely erythematous, demarcated rash involving the periocular region.
References and additional resources
- Bonnetblanc J & Bedane C. Erysipelas recognition and management. Am J of Clin Dermatology. 2003; 4(3): 157-163.
- Bartholomeeusen S, Vandenbroucke J, Truyers C, Buntinx F. Epidemiology and comorbidity of erysipelas in primary care. Dermatology. 2007;215:118–122.
- Stulberg D, Penrod, M, Blanty, RA. Common bacterial skin infections. Am Fam Physician. 2002 Jul 1;66(1):119-125.
- Morris AD. Cellulitis and erysipelas. BMJ Clin Evid. 2008;1708.
- Batista M & Goncalo M. The rash that presents as a red swollen face. Clinics in Dermatology. 2020; 38(1): 63-78.
- Bishara J, Golan-Cohen A, Robenshtok E, et al. Antibiotic use in patients with erysipelas: a retrospective study. Isr Med Assoc J 2001; 3: 722-4.
- Brindle R, Williams MO, Barton E. Assessment of Antibiotic Treatment of Cellulitis and Erysipelas: A Systematic Review and Meta-analysis. JAMADermatol. 2019;155(9):1033-1040.
- Karakonstantis S. Is coverage of S. aureus necessary in cellulitis/erysipelas? A literature review. Infection. 2020;48:183–191.
- Stevens D, Bisno A, Chambers H. Executive Summary: Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2014; 59(2): 147-159.
- Lazzarini L, Conti E, Tositti G & de Lalla F. Erysipelas and cellulitis: clinical and microbiological spectrum in an Italian tertiary care hospital. J Infect. 2005;51(5):383-9.
- Trell K, Rignér S, Wierzbicka M, et al. Colonization of β-hemolytic streptococci in patients with erysipelas-a prospective study. Eur J Clin Microbiol Infect Dis. 2019;38(10):1901‐1906.
- Costa JF, Marques JP, Marques M, Quadrado MJ. Endogenous endophthalmitis secondary to erysipelas. BMJ Case Reports. 2015: bcr2014209252.
- Buckland G, Carlson J, Meyer D. Persistent Periorbital and Facial Lymphedema Associated With Group A [beta]-Hemolytic Streptococcal Infection (Erysipelas). Ophthal Plast Reconstr Surg. 2007;23(2):161-163.
Financial disclosures
Financial Disclosures
Reviewers
Victoria North – No disclosures
