Trachoma
Updated May 2024
Establishing the diagnosis
Etiology
Trachoma is a chronic follicular conjunctivitis cause by infection with Chlamydia trachomatis.
Slow spontaneous resolution of the infection is accompanied by scarring of the conjunctiva.
Many who live in endemic areas have repeated infections, causing significant palpebral conjunctival scarring and cicatricial entropion, leading to corneal ulceration and opacification.
Epidemiology
According to current estimates there are still 84 million people in the world with active trachoma (chronic infection) in 55 countries in which the disease is still endemic (Solomon, New Engl J Med 2004).
In the 1970s it was estimated that 500 million people worldwide were affected by trachoma, of whom 7 million were blinded by the disease (Thylefors, Bull World Health Organ 1995).
As late as 1984, in Saudi Arabia, a national eye survey found that trachoma was still the second leading cause of blindness, after cataracts, with 9.5% of school children found to have clinical evidence of active trachoma (Tabbara, JAMA 1986; Sallam, Saudi Med J 2003).
Worldwide efforts have reduced the prevalence of trachoma dramatically, but it still accounts for about 3.6% of world blindness (Resnikoff, Bull World Health Organ 2004).
Several countries are close to being verified as having eliminated trachoma, including Morocco, Ghana, and Oman (Sommer, JAMA Ophthalmol 2014).
- As of 2014, there are still countries with high chlamydia prevalence, such as Ethiopia, South Sudan, and Nigeria, and countries where trachoma reduction programs have not yet gained significant traction such as Somalia and the Democratic Republic of Congo.
Efforts to eradicate trachoma can be understood from the example of rural Myanmar/Burma, where a Trachoma Control Program (TCP) was created in 1964, beginning with efforts to surgically correct trichiasis, followed by primary prevention programs using the World Health Organization (WHO) recommendations for antibiotics, facial hygiene and environmental change (Durkin, Ophthalmology 2007).
- The prevalence of active disease in this region in the 1960s was more than 30%.
- By 1975 the prevalence had been reduced to about 20%.
- In a 2005 survey of 2,076 inhabitants ≥ 40 years old in rural villages, the population percentage of trachomatous trichiasis and corneal opacity had been further reduced to 2.6%.
- SAFE is an acronym for surgery for trichiasis, antibiotic treatment, face washing and environmental improvements.
- WHO efforts include latrine construction, face-washing campaigns availability of clean water and widespread distribution of oral azithromycin.
- Eye-seeking flies are an important vector for the transmission of chlamydia and providing clean water and teaching children to clean the area around their eyes keeping it clear of secretions reduces spread of the disease.
- The British Broadcasting Corporation developed health education print material, radio programs and videos in support of the SAFE program (Edwards, Ophthalmology 2006).
- In 2 Ethiopian villages the polymerase chain reaction evidence of infection among children aged 1–5 years was reduced from 48% to 0% at 42 months through biannual mass distribution of azithromycin (Biebesheimer, Ophthalmology 2009).
- The mean elimination time is about 7–8 months faster if the antibiotics are distributed twice yearly, versus annual distribution (Gebre, Lancet 2012).
An arid climate is conducive to endemic infection, the prevalence is lower in regions with greater rainfall (Schwab, Ophthalmology 1995).
Disease burden:
- Estimated at 1.3 million life years
- Economic burden estimated at $5.3 billion in lost productivity
Highest current incidence is in India, China, Africa, and the Middle East.
Low incidence in Europe and North America:
- Related to improved hygiene rather than trachoma elimination program
- Low-grade trachoma persists: In Roraima, Brazil, where trachoma was thought to have been eradicated, a recent survey of 6,986 students grades 1–4 showed the overall prevalence rate was still 4.5%.
- There are still municipalities in Roraima where the prevalence is particularly high among school children, around 10%, and the prevalence rate among 2,152 family and school contacts of those children 9.3% (Medina, Ophthalmology 2011).
History
Establish country of origin.
Inquire about travel or work in endemic areas.
Duration:
- Clinical signs accumulate slowly over years.
- Often a latent period between infection and clinical signs
Symptoms:
- Ocular irritation
- Reduced vision
Clinical features
- Conjunctival follicles
- Follicles often greater than 0.5 mm
- Conjunctiva/tarsal scarring (Arlt’s line)
- Cicatricial entropion
- Dry eye
- Trichiasis
- Corneal opacification
- Central secondary to trichiasis/corneal drying
- Superior pannus
- Herbert’s pits
- Depression resulting from resolved limbal follicles
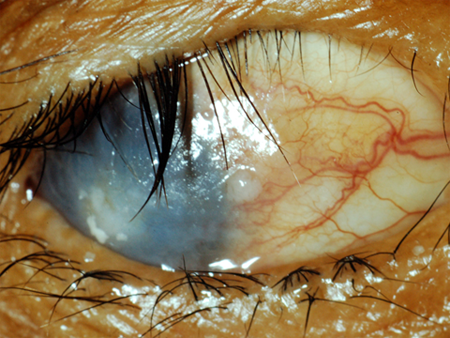
Figure 1. Trachoma-related cicatricial entropion secondary to posterior lamellar scarring and contraction. Also note marked ocular surface disease with corneal scarring, indicative of chronicity. Image courtesy of Thomas M. Lietman, MD.

Figure 2. Inflamed palpebral conjunctiva in a patient with untreated active trachoma infection. Arlt’s line refers to the linear scaring 2–3 mm adjacent the lash line. Incision along this line often aids in surgical repositioning of the eyelid margin. Also note disease-carrying flies on lower eyelid. Image courtesy of Thomas M. Lietman, MD.

Figure 3. Noninflamed scarred conjunctiva in a patient with treated tachoma infection. Note diffuse irregular scarring, indicative of years of untreated infection. Image courtesy of Thomas M. Lietman, MD.
Testing
Diagnosis can usually be inferred from clinical findings in appropriate setting.
Histopathology shows a thick, compact, subepithelial fibrous membrane adherent to the upper lid tarsus, loss of meibomian glands, loss of goblet cells, and degeneration of the tarsus with replacement by adipose tissue (al-Rajhi, Ophthalmology 1993).
In vivo confocal microscopy (IVCM) is a noninvasive means of obtaining high-resolution tissue images at a cellular level (Hu, Ophthalmology 2011).
- In normal conjunctiva, IVCM can identify normal epithelial cell nuclei, inflammatory cell nuclei, and dendritic cells.
- There are also tubular microcysts in the superficial conjunctiva which contain highly reflective material.
- There is a fine network of small blood vessels 20–30 microns beneath the surface and brightly reflective fibrous material.
- In trachomatous conjunctiva, with active disease, in children, IVCM demonstrates more numerous dendritic cells, with longer dendritic processes that are often interdigitating (Hu, Massae, Ophthalmology 2011).
- The cystic spaces are larger and more irregular.
- In trachomatous conjunctiva, with scarring, in adults, there is evidence of chronic inflammation, both papillary and follicular conjunctivitis, with an increase in inflammatory cells.
- Increased cysts and dendritic cells are seen in adults.
- With increasing severity of scarring, the deeper subepithelial connective tissue contains broad bands of scar tissue arranged in parallel.
In vivo confocal microscopy can be performed using the Heidelberg Retina Tomograph 3 (HRT3) in combination with the Rostock Cornea Module (RCM).
- This uses a 670-nm diode laser as a light source with a special water-contact objective covered with a sterile single-use polymethylmethacrylate (PMMA) cap.
- A small amount of carbomer gel is used as a coupling agent.
- The device scans at a magnification of x800 and a lateral resolution of 1 micron.
Nuclear acid amplification tests (NAATs):
- DNA-based
- rRNA-based
- Point of care assay of Chlamydial lipopolysccharides
Testing for staging, fundamental impairment
There is a simplified WHO trachoma grading system, mnemonic = FISTO:
- Trachomatous inflammation: follicular (TF) = the presence of 5 or more follicles in the upper tarsal conjunctiva.
- Trachomatous inflammation: intense (TI) = pronounced inflammatory thickening of the tarsal conjunctiva that obscures more than half of the deep normal vessels.
- Trachomatous scarring (TS) = presence of scarring in the tarsal conjunctiva.
- Trachomatous trichiasis (TT) = at least one lash rubbing on the eye.
- Corneal opacity (CO) = easily visible corneal opacity over the pupil.
Risk factors
- Exposure to endemic area
- Poor hygiene
Differential diagnosis
- Ocular cicatricial pemphigoid
- Topical medication (glaucoma medication is most common)
Patient management: treatment and follow-up
Natural history
- With active infection, slow progression is expected.
- With inactive disease, eyelid deformation is stable.
- But if trichiasis/eyelid malposition is not corrected, corneal injury continues.
- Stable once eyelid abnormality and infection are treated
Medical therapy
In the 1930s and 1940s oral sulfonamides were distributed, especially in North America, to treat trachoma, but the practice was discontinued due to an unacceptably high incidence of adverse reactions, especially Stevens-Johnson syndrome (Solomon, New Eng J Med 2004).
In the 1950s and 1960s tetracycline ointment was distributed in a number of countries, but effective treatment required a 6-week course, making compliance difficult.
A single oral dose of azithromycin was found to have similar efficacy (63% vs. 65% resolution of clinical trachoma) compared to the tetracycline regimen (Tabbara, Ophthalmology 1996).
- Peak levels in the serum and tears are found to be therapeutic within 12 hours after a single dose of oral azithromycin (Karcioglu, Ophthalmology 1998).
A directly observed single oral dose of azithromycin 20 mg/kg (maximum 1 gm) is the accepted standard.
Annual treatment is recommended wherever the prevalence of active trachoma infection among children is 20% or greater.
Topical lubrication is offered for corneal protection associated with dry eye and loss of meibomian glands.
Surgery
There are 3 main surgical techniques used around the world:
- The bilamellar tarsal rotation (BLTR) procedure has been endorsed by WHO has a standard surgery.
- It is described in the WHO manual and is performed by non-physicians in areas where the need is greatest (Bog, BJO 1993).
- This technique is similar to the Weis procedure used for entropion of the lower lid, and was described by Ballen as a treatment for upper lid entropion (Ballen, Arch Ophthalmol 1964).
- The BLTR is a full thickness incision made 3 mm above and parallel to the lid margin, for a length of 20 mm, coupled with rotation sutures.
- Some suggest staggering the two incisions with the skin incision 4 mm above the lash line and the posterior lamella incision 2.5 mm above the lid margin (Sandford-Smith, Br J Ophthalmol 1976).
- Everting sutures are passed from the tarsal conjunctiva through the anterior lamella.
- The second surgical approach is the Trabut method – a horizontal incision made in the posterior lamella, above the lash line, with everting sutures to bring the posterior lid margin forward. (Reacher, BJO 1990)
- The third is the Cuenod-Nataf procedure – a posterior tarsal incision and dissection along the posterior lamella so that it can be elongated and brought down to the lid margin, as an additional barrier to prevent lash contact with the cornea. (Thanh, BJO 2004)
Trichiasis recurrence after surgery is very high:
- In a survey of postoperative patients in Oman the recurrence rate was 62% after three years
- Left eye recurrence is more common than right, possibly due to difficulties for right-handed surgeons (Merbs, Ophthalmology 2005).
- Among 1,917 patients in Ethiopia who underwent BLTR surgery in 2009 the rate of post-operative trichiasis at two years was about 40% (Gower, JAMA Ophthalmol 2013).
Active chlamydial infection at the time of eyelid surgery is an important risk factor for post-operative recurrence of trachomatous trichiasis (Zhang, Arch Ophthalmol 2004).
The STAR trial (surgery for trichiasis, antibiotics to prevent recurrence) coupled antibiotics with surgery to minimize recurrence:
- In Southern Ethiopia, 1,452 patients underwent trichiasis surgery and were randomized to a single dose of azithromycin versus topical tetracycline following surgery (Woreta, Arch Ophthalmol 2012).
- The rate of recurrence was 10% in the azithromycin group and 13% in the tetracycline group.
Patients with trichiasis, without entropion, can also be treated with tarsotomy:
- Eplilation is an alternative.
- Mechanical
- Cryotherapy
- Electrolysis
- Eyelid can also be split with mucous membrane grafting
Other management considerations
Trachoma was eliminated during the 20th century in Western Europe and the United States through improved living conditions and economic development, without a direct trachoma control program (Numazaki, Lancet 1997).
The WHO initiated a global program to eliminate blindness from trachoma by 2020:
- The main limiting factor continues to be access to surgery for entropion and trichiasis (Lietman. Ophthalmology 2001).
Once the disease has caused scarring, blindness can ensue despite intervention:
- In a 12-year longitudinal follow-up of 362 patients in Gambia with some degree of trachomatous scarring, corneal opacity developed in 6%, and visual impairment developed in 2.5%.
- A history of lid surgery was a significant risk factor for the development of corneal opacity at follow-up (Bowman, Ophthalmology 2001).
In addition to the SAFE efforts, there are initiatives to educate patients on epilation of trichiatic lashes, and high quality forceps have been distributed.
- In a study of 4,310 eyes with trichiasis from trachoma, with epilation performed at least once a month (in 77% of the eyes) by someone other than the patient (in 93% of cases), the incidence of corneal opacity was reduced in patients with severe entropion (Rajak, Ophthalmology 2012).
Bandage contact lens can also be important for protection of the cornea – as a temporizing measure until surgery can be arranged.
Common treatment responses, follow-up strategies
Once active infection is eliminated focus is on correction of trichiasis and entropion.
Reinfection is a problem in endemic regions.
Dry eye disease is likely longstanding and can require treatment.
Preventing and managing treatment complications
Antibiotics
- Resistance has been reported.
- Allergy
Tarsotomy
- Failure to adequately correct eyelid position might require repeat surgery.
- Necrosis of eyelid margin is a complication best avoided by spacing sutures and avoiding overly aggressive dissection.
Epilation
- Cryotherapy often results in eyelid deformation and for this reason is avoided by many surgeons.
- Electrolysis is expensive and has a high recurrence rate, often requiring repeat treatment.
Disease-related complications
- Conjunctival inflammation
- Trichiasis
- Tarsal scarring and deformation resulting in entropion
- Corneal opacity
- Secondary bacterial corneal infection
- Blindness
Historical perspective
In a 1915 article in the Boston Medical and Surgical Journal, the forerunner of the New England Journal of Medicine, a “native” outbreak of trachoma was described, meaning it was not introduced to the US by immigrants, in the mountainous regions of West Virginia and Kentucky (New Engl J Med 1915; 173:820).
- “Investigations carried out by the Public Health Service…revealed the fact that this ophthalmia and the resulting high percentage of blindness was trachomatous.”
- “The pointing out by Massachusetts medical men of the prevalence and the dangers of trachoma …through the importation of this disease by immigrants…(led to) the barring of immigrants suffering from this condition.”
- This barring of immigrants “awakened not only foreign governments to the menace of this disease and the taking of measures against it, but the number of immigrants with active disease attempting immigration has fallen to a negligible quantity.”
- “It is true that thus far all attempts to locate a specific germ or other specific causative factor have proved fruitless…To various bacteria found in the discharges have been ascribed the causation of this disease, but thus far none of them has fulfilled the Koch postulate necessitating the isolation, the cultivation in pure culture, the reinfection with the bacteria, and the recovery of the specific bacterium.”
- “In these mountainous cases…the sanitary conditions and the mode of living fully warranted the spread of this disease among them, especially during the winter, when a whole family would be huddled up in one cabin, using the same towel, the same basin, and the same water.”
Ten years earlier, the clinical course of trachoma among US patients had been described among immigrants to the US from Ireland, Poland, and other parts of Europe (Boston Med Surg J 1906; 155:305).
- “It is said that trachoma originated in Egypt, where it is endemic and from whence it has spread over practically all the countries of the temperate and tropical zones.”
- Napoleon’s soldiers are said to have brought it back to Europe from Egypt.
- “In his campaign of 1798, more than 20,000 of his followers contracted the disease. In light of this fact, it is easily believed that the resulting epidemic in Europe lasted 30 years and that more than 1 million people were infected.”
- “As the granulations increase in size, the symptoms change. He complains of the eyes feeling as though sand were in them. They are hot and burning, and the tears, instead of being cool and moist, are scalding and there is an excessive flow.”
- “The lids move over the globe with more and more difficulty and any clear cornea that had remained is converted into a dense opacity.”
Ten years before that (Boston Med Surg J 1897; 137:417), it was suggested that tincture of iodine was better than galvanocautery for trachoma and other suppurative conditions of the external eye because it was just as effective and “leaves less scar”.
Intracytoplasmic inclusions were identified by Halberstaedter and Prowazek in 1907 and the first successful culture of trachoma was by Tang in 1957 (Arch Ophthalmol 1963; 69:143).
Trachoma is 1 of 6 major epidemics that have invaded America since 1900 (New Engl J Med 2005; 352:1828), the others being tuberculosis, plague, typhus, AIDS, and cholera.
In the book Forgotten Ellis Island (Lorie Conway, Smithsonian Books, 2007), the author writes sympathetically of the “anxiety and bewilderment of the men, women, and children who were pulled out of lines in the Great Hall and taken to the hospital. The eye disease trachoma, which ultimately leads to blindness, was particularly difficult for many immigrants to comprehend. Persons who were diagnosed with this condition, but who were not yet visually impaired often could not fathom why they were being denied admittance to the nation” (New Engl J Med 2008; 358:11).
Forceps thought to have been used to remove eyelashes to treat trachoma have been found in many ancient Egyptian tombs (Surv Ophthalmol 2012; 57:105).
References and additional resources
- http://trachoma.org/
- http://www.who.int/topics/trachoma/en/
- Al-Rajhi AA et al. The histopathology and the mechanism of entropion in patients with trachoma. Ophthalmology 1993; 100:1293.
- Ballen PH. A SIMPLE PROCEDURE FOR THE RELIEF OF TRICHIASIS AND ENTROPION OF THE UPPER LID. Arch Ophthalmol 1964; 72:239
- Bhosai SJ, Bailey RL, Gaynor BD, Lietman TM. Trachoma: an update on prevention, diagnosis, and treatment. Curr Opin Ophthalmol. 2012;23:288-95.
- Biebesheimer JB et al. Complete local elimination of infectious trachoma from severely affected communities after six biannual mass azithromycin distributions. Ophthalmology 2009; 116:2047
- Bog H et al. Results of community-based eyelid surgery for trichiasis due to trachoma. BJO 1993; 77:81
- Bowman RJ et al. Natural history of trachomatous scarring in The Gambia: results of a 12-year longitudinal follow-up. Ophthalmology 2001; 108:2219.
- Durkin et al. Prevalence of trachoma-related trichiasis and corneal opacity in rural Myanmar: the Meiktila Eye Study. Ophthalmology 2007; 114:e7-11.
- Edwards T el al. Impact of health education on active trachoma in hyperendemic rural communities in Ethiopia. Ophthalmology 2006; 113:548
- Frick KD, Hanson CL, Jacobson GZ. Global Burden of trachoma and economics of the disease. Am J Trop Med Hyg 2003;69:1-10.
- Gebre T et al. Comparison of annual versus twice-yearly mass azithromycin treatment for hyperendemic trachoma in Ethiopia: a cluster-randomised trial. Lancet 2012; 379:143-51.
- Gower EW et al. Trachomatous trichiasis clamp vs standard bilamellar tarsal rotation instrumentation for trichiasis surgery: results of a randomized clinical trial. JAMA Ophthalmol 2013; 131:294
- Hu VH et al. In vivo confocal microscopy in scarring trachoma. Ophthalmology 2011; 118:2138-46
- Hu VH, Massae P, et al. In vivo confocal microscopy of trachoma in relation to normal tarsal conjunctiva. Ophthalmology 2011; 118:747-54.
- Karcioglu ZA et al. Pharmacokinetics of azithromycin in trachoma patients: serum and tear levels. Ophthalmology 1998; 105:658
- Lietman TM. Trachoma control: the end of the beginning? Ophthalmology 2001; 108:2163
- Medina NH, Lopes MF, Durkin SR, et al: Survey of trachoma within school students in the state of Roraima, Brazil. Ophthalmology 2011; 118:1938.
- Merbs SL et al. Pattern of recurrence of trachomatous trichiasis after surgery surgical technique as an explanation. Ophthalmology 2005; 112:705
- Numazaki et al. Reduction of trachoma in absence of a disease-control programme. Lancet 1997; 350:447
- Rajak SN et al. Epilation for trachomatous trichiasis and the risk of corneal opacification. Ophthalmology 2012; 119:84
- Reacher MH et al. A trial of surgery for trichiasis of the upper lid from trachoma. Br J Ophthalmol. 1990 Feb;74(2):109-13
- Resnikoff S, Pascolini D, Etya’ale D, et al: Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82:844.
- Sallam TA et al. Chlamydia trachomatis infections among Yemeni school pupils in relation to environmental conditions. Saudi Med J. 2003 Jan;24(1):84-7.
- Sandford-Smith JH. Surgical correction of trachomatous cicatricial entropion. Br J Ophthalmol 1976; 60:253
- Schwab L et al. The epidemiology of trachoma in rural Kenya. Variation in prevalence with lifestyle and environment. Study Survey Group. Ophthalmology 1995; 102:475
- Solomon AW et al. Mass treatment with single dose azithromycin for trachoma. New Engl J Med 2004; 351:1962-71.
- Sommer A et al. Challenges of ophthalmic care in the developing world. JAMA Ophthalmol 2014; 132:640.
- Tabbara KF et al. Blindness in Saudi Arabia. JAMA 1986; 255:3378
- Tabbara KF et al. Single-dose azithromycin in the treatment of trachoma. A randomized, controlled study. Ophthalmology 1996; 103:842-6
- Thanh TT et al. One year recurrence of trachomatous trichiasis in routinely operated Cuenod Nataf procedure cases in Vietnam. Br J Ophthalmol. 2004 Sep;88(9):1114-8.
- Thylefors B et al. Global data on blindness. Bull World Health Organ 1995; 73:115.
- Woreta F et al. Three-year outcomes of the surgery for trichiasis, antibiotics to prevent recurrence trial. Arch Ophthalmol 2012; 130:427
- Zhang H et al. Risk factors for recurrence of postoperative trichiasis: implications for trachoma blindness prevention. Arch Ophthalmol 2004; 122:511
