Plasma Cell Tumors of the Orbit and Periocular Region
Updated May 2024
Establishing the diagnosis
Etiology
- Monoclonal or polyclonal proliferations of plasma cell or plasmacytoid lymphocytes
- IgG is most common, followed by IgA.
- 4 main variants (Burkat, Surv Ophthalmol. 2009)
- Polyclonal plasma cell tumor
- Heterogenous population of plasma cells and lymphocytes
- Typically affect conjunctiva, but can be found in the orbit
- Solitary plasmacytomas
- Isolated monoclonal plasma cells within bone
- No other skeletal bone involvement
- Extramedullary plasmacytoma
- Develops in soft tissue
- Commonly occur in upper respiratory tract and sinuses with orbital extension
- Plasma cell myeloma (multiple myeloma)
- Arise from bone marrow of skeletal bone; leukemic stage
- Lytic lesions of bone
- Necrobiotic xanthogranuloma (NXG)
- Histiocytic nodules that affect eyelids and periorbitum
Epidemiology
Solitary Plasmacytoma
- 6th–7th decades
- Male to female: 3:1
Extramedullary plasmacytoma
- 7th–8th decades
- Male to female: 2:1
Plasma cell myeloma
- 68–70 years median age
History
- Typically a manifestation of systemic disease; rarely a solitary focus in the orbit
- 65% of patients presenting with orbital involvement are carrying a diagnosis of multiple myeloma (MM) (Burkat, Surv Ophthalmol. 2009).
- Weight loss/fatigue
- Bone pain
- Particularly in multiple myeloma, whereas solitary plasmacytoma typically do not cause pain
- Anemia
- Hypercalcemia
- Lytic lesions of bone
- Peripheral neuropathy
- Cutaneous rash
Clinical features
(Burkat, Surv Ophthalmol. 2009)
- Slowly progressive proptosis (axial or abaxial) is the most common presenting sign.
- Periorbital swelling (Figure 1)
- Loss of vision
- Ptosis
- Diplopia
- Can be bilateral, however unilateral is more common (Malik, Indian J Ophthalmol. 2009)
- Location varies:
- Most commonly superotemporal, posterior, and extraconal
- Bone involvement is common.
- Solitary plasmayctoma
- Multiple myeloma
- Can also affect the lacrimal gland, optic nerve and extraocular muscles
- Amyloidosis develops in 8%–15% of patients.
- Should also be included in the differential diagnosis for a multiple myeloma patient with an orbital or subconjunctival mass
- Although the orbit is the most common location, conjunctival and anterior segment lesions have also been documented.
- May manifest as a salmon patch conjunctival mass.
- Systemic myeloma can present with orbital muscle swelling and proptosis due to paraproteinemia (Rootman, Diseases of the Orbit: A multidisciplinary approach 2002).

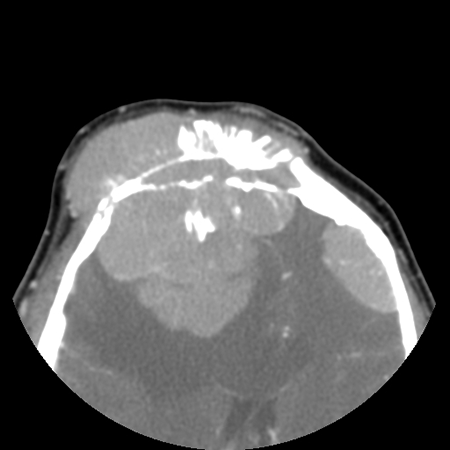
Figure 1. Top: Periorbital swelling seen clinically. Bottom: Axial CT of the patient demonstrating periorbital and intracranial involvement with bony remodeling.
Testing
- Patients need to be evaluated for MM.
- Serum/urine protein electrophoresis for immunoglobulin components
- Light chain (Bence-Jones protein)
- Heavy chain (IgG, IgA, etc.)
- 15% of cases do not have immunoglobulinemia (Bataille, New Engl J Med 1997).
- Free light chain assay
- Serum calcium elevated in MM
- Erythrocyte sedimentation rate
- Alkaline phosphatase level elevated in MM
- Complete blood count with differential
- Bone marrow aspirate
- Skeletal bone imagery
- Scintigraphy of the head and neck
- Positron emission tomography (PET) scan
- Computed tomography
- Solitary plasmacytoma of bone: bone erosion
- Extramedullary plasmacytoma: homogeneous, nonencapsulated mass with mild enhancement; molds to surface of globe
- Plasma cell myeloma: soft tissue mass in retrobulbar space; may see lysis of walls of orbit; appears attached to underlying bone
- Magnetic resonance imaging (Jackson, Br J Radiol. 1993) (Figure 2)
- T1: Intensity similar to extraocular muscles
- T2: Intensity similar to orbital fat
- Useful in distinguishing from metastasis which generally are more intense that fat
- Tissue diagnosis critical in diagnosing the lesion and subsequent evaluation
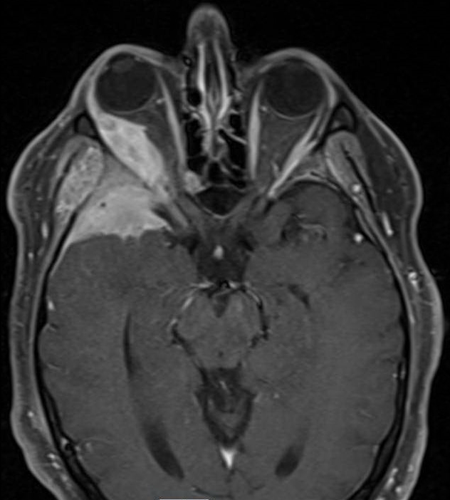
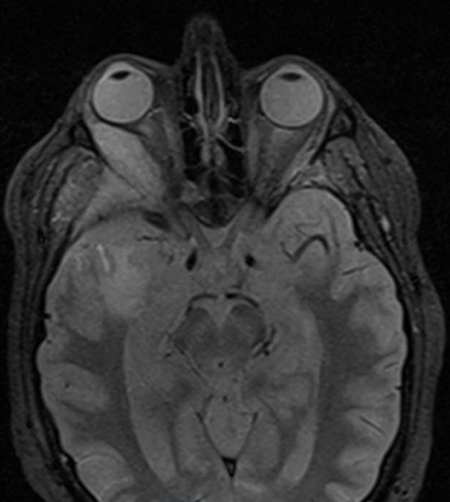
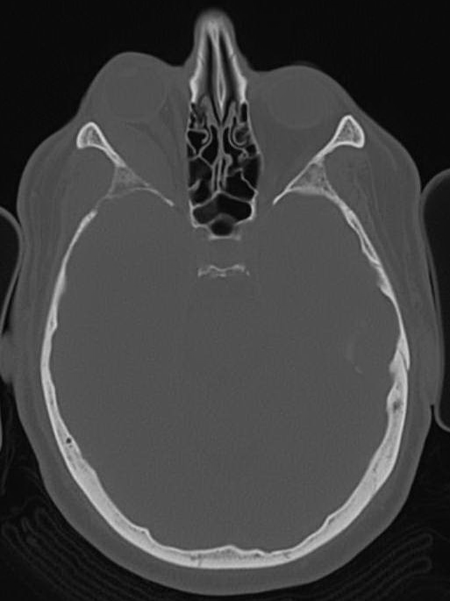
Figure 2. MRI and CT of a patient with plasmacytoma involving brain and R lateral orbit. Note the relative paucity of bony changes on the CT and the variable densities of the mass on T1- and T2-weighted images.
Risk factors
- Age: The incidence of myeloma increases with age and peaks in individuals more than 80 years of age.
- Race: More common in blacks than whites
- Obesity: Body mass index (BMI) greater than 30
- Family history: More common in individuals with a family history of monoclonal gammopathy
- Gender: More common in men than women
Differential diagnosis
- Lymphoma and other lymphoproliferative disorders
- Metastatic lesions
Patient management: treatment and follow-up
Natural history
- Mean survival (de Smet, Ophthalmology. 1987)
- Plasmacytoma: 28 months
- Compared to 8.3 years for plasmacytomas located in other areas of the body
- Extraosseous plasmacytoma: 8.3 years
- Multiple myeloma: 24 months
- Plasmacytoma (de Smet, Ophthalmology. 1987)
Treatment options
(Rootman, Diseases of the Orbit: A multidisciplinary approach 2002)
- Polyclonal plasmacytoma
- Excision
- Large or inaccessible lesions can be treated with low-dose radiation.
- Solitary plasmacytoma of orbital bone: radiotherapy
- Extraosseous plasmacytoma
- Radiotherapy as initial treatment
- Surgical excision and chemotherapy for persistent and recurrent disease
- Plasma cell myeloma
- Chemotherapy
- Bone marrow transplantation
Surgery
- Aimed at obtaining a tissue diagnosis
- Excisional biopsy
- Fine needle aspiration (Yakulis, A case report. Acta Cytol. 1995)
Preventing and managing treatment complications
- Surgical complications
- Radiotherapy complications
- Chemotherapy complications
Disease-related complications
- Development of multiple myeloma
- Solitary plasmacytoma of bone: 50%
- Extraosseous plasmacytoma: 15%
- Necrobiotic xanthogranuloma: 10 %
Patient instructions
Monitor for palpable mass in orbit following initial therapy to detect recurrence.
Follow osseous and extraosseous plasmacytoma patients for possible plasma cell myeloma.
References and additional resources
- AAO, Basic and Clinical Science Course. 2010-11.
- Bataille R, Harousseau JL. Medical progress: multiple myeloma. New Engl J Med. 1997;336:1657-64
- Ben Artsi E, Barkley MR, Khong JJ, Mckelvie PA, McNab AA, Hardy TG. Multiple myeloma manifesting as an ocular salmon patch – a case report. Orbit. 2020 Oct;39(5):379-382. doi: 10.1080/01676830.2019.1691608. Epub 2019 Nov 13. PMID: 31722590.
- Bhadauria M, Ranjan P, Mishra D. Primary Orbital Plasmacytoma Mimicking Lacrimal Gland Tumor. Orbit. 2014 May 15:1-3.
- Black EH, et al. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. 3rd ed. New York: Springer; 2012; 1213
- Br J Radiol. 1993 Mar;66(783):266-8.
- Burkat CN1, Van Buren JJ, Lucarelli MJ. Characteristics of orbital multiple myeloma: a case report and literature review. Surv Ophthalmol. 2009 Nov-Dec;54(6):697-704.
- Chin KJ, Kempin S, Milman T, Finger PT. Ocular manifestations of multiple myeloma: three cases and a review of the literature. Optometry 2011 Apr;82(4):224-3.
- de Smet MD, Rootman J. Orbital manifestations of plasmacytic lymphoproliferations. Ophthalmology. 1987 Aug;94(8):995-1003.
- Gangadhar K, Santhosh D, Kallahalli S. A rare differential diagnosis for cause of proptosis: skull plasmacytoma. Neuroradiol J. 2012 Jul;25(3):374-8
- Garrity JA, Henderson JW. Henderson’s Orbital Tumors. 4th edition. Lippincott Williams & Wilkins. 2007.
- Jackson A, Kwartz J, Noble JL, Reagan MJ. Case report: multiple myeloma presenting as bilateral orbital masses: CT and MR appearances.
- Malik A, Narang S, Handa U, Sood S. Multiple myeloma presenting as bilateral orbital proptosis. Indian J Ophthalmol. 2009 Sep-Oct;57(5):393-5
- Rootman, J. Diseases of the Orbit: A multidisciplinary approach. 2nd revised edition, Lippincott Williams & Wilkins. 2002.
- C. Shen, C. Y. Wang, T. Y. Huang, Y. S. Lo, S. C. Fong, and Y. F. Lee, Multiple myeloma manifesting as a salmon patch conjunctival mass, American Journal of Ophthalmology, vol. 141, no. 5, pp. 948–949, 2006.
- Yakulis R1, Dawson RR, Wang SE, Kennerdell JS. Fine needle aspiration diagnosis of orbital plasmacytoma with amyloidosis. A case report. Acta Cytol. 1995 Jan-Feb;39(1):104-10.
