Carotid Cavernous Sinus Fistula
Updated July 2024
Establishing the diagnosis
Etiology
Fistulous tract between arterial and venous vascular supply allows shunting of blood from carotid artery or its tributaries to the cavernous sinus (a trabeculated venous cavity).
Hemodynamically, this results in arterial pressure in the venous channel and its tributaries, causing congestion and ischemia.
Anatomy
The cavernous sinus normally measures 2 cm anteroposteriorly by 1 cm in lateral width and 1.3 cm in vertical height (J Craniofac Surg 1995; 6:55).
The sixth cranial nerve runs within the cavernous sinus, lateral to the internal carotid artery.
Other nerves including III, IV, V1, and V2 pass in the lateral wall of the cavernous sinus between 2 dural layers.
The cavernous sinus receives drainage from the sphenoparietal sinus, superior ophthalmic vein,and superficial sylvian vein.
The middle meningeal vein empties into the cavernous sinus laterally.
The superior and inferior petrosal sinuses drain the cavernous sinus posteriorly.
The intercavernous sinus and basilar plexus of veins connect the 2 cavernous sinuses.
Indirect fistula
- Low-flow fistula between branches of the internal or external carotid artery and the cavernous sinus
- Degenerative process in older patients with systemic hypertension and atherosclerosis
- Posttraumatic indirect fistulas have been reported (Orbit 2003; 22:121).
- Spontaneous; onset can be insidious.
Direct fistula
- High-flow connection between the main trunk of the internal carotid artery and venous channels in the cavernous sinus
- Typically occurs after trauma with tear through the wall of the internal carotid artery
- Can also follow rupture of carotid artery aneurysm.
- Diversion of arterialized blood into the venous system causes venous outflow obstruction, which leads to elevated IOP, choroidal effusions, and blood in the Schlemm canal.
- Young patients can develop spontaneous high-flow fistulas in the context of elastin disorders such as Ehlers-Danlos syndrome (Ophthalmology 1983; 90:1337).
Barrow classification
(J Neurosurg 1985; 62:248)
- Type A: internal carotid artery (caused by trauma or aneurysm)
- Type B: meningeal branches of internal carotid artery
- Type C: meningeal branches of external carotid artery
- Type D: meningeal branches of internal and external
Epidemiology
Direct carotid artery fistulas are more common in males, with 80% associated with trauma.
Indirect dural artery fistulas are associated with atherosclerotic disease and are more common in elderly females.
In an early study of 132 patients, 75% were Barrow type A, 0% type B, 3% C, and 22% D (Neurosurgery 1988; 22:285).
Type A direct fistulas have become less common due to motor vehicle restraints and air bags (Neurosurg Focus 2012; 32:E9).
In a 2005–2013 review of 38 indirect dural fistulas, 76% were female and average age was 63 years (Eur Radiol 2014; 24:3051).
History
- Antecedent trauma includes presumably incidental episodes and contact without obvious sequelae (J Emerg Med 2014; 46:475).
- Can be remote trauma of 6 months or more (J Emerg Med 2015; 48:186)
- Orbital bruit with high flow direct fistulas
- Although helpful if found, the absence of a bruit does not argue against the diagnosis of a fistula.
- Proptosis: Chemosis can precede proptosis in low-flow dural fistulas and can be a relatively benign condition (J Neurointervent Surg 2013; 5:e1).
- Red eye correlates with higher degree of orbital congestion and arterialization of conjunctival vessels with increasing tortuosity.
- Decreased vision
- Diplopia, ophthalmoplegia
- Facial pain
- Headache
Clinical features
Ocular presentation is common.
- Proptosis, eyelid edema
- Chemosis: specific, uncommon association
- Isolated chemosis, possibly with some proptosis, can be a subtle presentation (J Emerg Med 2015; 48:186).
- Bruit
- Headache can be sudden onset without trauma, such as with direct aneurysmal fistula (BMJ Case Reports 2015, 2015).
- Conjunctival injection is the most prominent feature of indirect fistulas.
- Episcleral “corkscrew” vessels extend to limbus.
- Elevated intraocular pressure is more prevalent with indirect fistulas (International Ophthalmol 2012; 32:153).
- Blood in Schlemm canal, recognized on gonioscopy, a sign of congestion
- Ophthalmoplegia
- In a 1984 report on 15 fistulas it was observed that patients with isolated abduscens palsy have normal muscle size on CT and recover slowly after closure of the fistula (Br J Ophthalmol 1984; 68:128).
- In contrast, patients with generalized ophthalmoplegia have enlarged extraocular muscles on CT and recover motility rapidly after embolization.
- Presumably, neurogenic ophthalmoplegia relates to ischemia of the isolated abduscens nerve as it courses through the cavernous sinus.
- When more global ophthalmoplegia is observed, with enlarged muscles on orbital imaging, it is from congestion and venous stasis.
- Seizures can be associated with cortical ischemia; signs of middle cerebral artery stroke have also been observed (J Emerg Med 2015; 48:186).
- Visual loss can be caused by varied ischemic processes.
- Ischemic optic neuropathy from reduced flow or compression
- Central retinal vein occlusion manifested by intraretinal/vitreous hemorrhage
- Choroidal effusion or detachment
- Optic disc swelling is a sign of congestion and/or ischemia.
- Angle closure glaucoma is caused by iris/choroid congestion, forward displacement of iris-lens diaphragm.
- Severe neurologic deficit is less common, related to intracranial engorgement and ischemia compromising feeding vessels to pons, midbrain, thalamus, and/or basal ganglia (J Neurointervent Surg 2013; 5:e1).
- Facial pain or numbness might be due to compression of Gasserian ganglion or fifth nerve branches.
- Epistaxis from venous engorgement
- Most severe spectrum of cortical and midbrain neurologic deficits can include weakness of all extremities and difficulty breathing (J Neurointervent Surg 2013; 5:e1).
- Can cause intracerebral hemorrhage and death

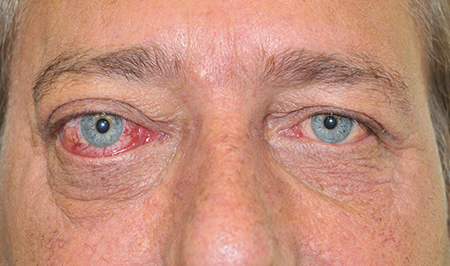
Figure 1. Right CCF seen in frontal photograph and from below. Note the proptosis, episcleral venous dilation with corkscrew vessels, and relative inferior scleral show.
Testing
- High-resolution CT (video) or MRI is the initial test of choice, although these scans can miss the diagnosis.
- Enlarged superior ophthalmic vein on orbital CT or MRI
- Extraocular muscle enlargement
- Flow voids
- Ultrasound with Doppler
- Can show reversed, arterialized blood flow in superior ophthalmic vein
- Can assess muscle size and superior ophthalmic vein size by ultrasound
- CT angiography and magnetic resonance angiography (MRA) has replaced conventional angiography as primary diagnostic modality, but can miss the fistula due to resolution.
- Conventional angiography
- Best chance of making the clinical diagnosis if clinical suspicion is high and other modalities are negative
- Performed in treatment planning
Risk factors
- Trauma with shearing force
- Basilar skull fracture a hallmark associated finding with direct fistula
- Advanced age or involutional changes
- Pregnancy — numerous case reports (Hong Kong Med J 2013; 19:258)
- Hypertension and atherosclerotic disease
- Elastic tissue diseases: Ehlers-Danlos syndrome type IV predisposes to direct aneurysmal fistula (BMJ Case Reports 2014, 2014).
Differential diagnosis
Congestion can be confused with thyroid eye disease.
Ophthalmoplegia and muscle enlargement can be confused with myositis.
Cavernous sinus thrombosis and infection have similar features.
Scleritis can cause congestion and proptosis.
Chronic blepharoconjunctivitis can cause chemosis and injection.
Patient management: treatment and follow-up
Medical and nonsurgical
Endovascular embolization is now the treatment of choice, replacing open surgical approach (Neurosurg Focus 2012; 32:E9).
Low-flow or dural cavernous fistulas have a high rate of spontaneous resolution and can at first be observed (Am J Neuroradiol 1991; 12:435).
Intervention is recommended for progressive, severe ocular symptoms.
Spontaneous resolution and thrombosis of the fistula has been reported after airplane travel, angiography (Am J Neuroradiol 1991; 12:435).
Manual compression of the external carotid artery and the angular vein can be prescribed for mild congestion.
- Patients are also instructed to compress the superomedial orbit for 5-10 minutes three times a day (Eur Radiol 2014; 24:3051).
Secondary effects of fistula formation can also be managed medically.
- Corneal exposure: Tarsorrhaphy and topical lubrication
- Elevated IOP: topical and systemic medication
- Diplopia: Occlusion and prisms followed by muscle surgery when disease is stabilized.
Surgery
Initially, transcavernous surgical approach was developed after recognition and description of carotid cavernous fistula by Parkinson (J Neurosurg 1967; 26:420).
Kupersmith et al. reported successful transfemoral venous embolization in 33 of 34 patients in 1986 (Ophthalmology 1986; 93:906).
Keltner et al. followed with reported success with embolization in 71% of 18 patients with direct and indirect fistulas (Ophthalmology 1987; 94:1585).
General anesthesia is usually needed for embolization.
Transfemoral venous catheterization targets the inferior petrous sinus to gain access to the cavernous sinus.
Arterial catheterization — in contrast to transvenous catheterization — via femoral artery or external carotid artery is ideally avoided because it carries higher risk of traumatizing dural feeding arterioles off the internal carotid artery.
Transorbital approach via the superior ophthalmic vein offers more direct access to the cavernous sinus.
- The transorbital approach is generally performed under general anesthesia (Ophthalmology 2006; 113:1220).
- The superior ophthalmic vein enters the anterior orbital fat just lateral to the trochlea, as confluent drainage from the supraorbital and angular veins.
- The vein continues posteriorly, medial to the superior rectus muscle, close to the orbital roof.
- The superior ophthalmic vein crosses over to the lateral border of the superior rectus before entering the cavernous sinus via the annulus and Zinn and superior orbital fissure.
- Fat is reflected laterally to expose the vein which is isolated on a suture ligature.
- Recent onset high flow direct fistulas are not optimally approached directly via the orbit, to avoid excessive bleeding (Ophthalmology 2006; 113:1220).
- In a series of 91 dural indirect, low flow fistulas treated from 1993-2005, cannulation of the superior ophthalmic vein was attempted in 25 patients, with six unsuccessful attempts due to difficulties isolating and accessing the vein in the orbit (Ophthalmology 2006; 113:1220).
The internal carotid artery can be directly accessed via the orbit, in extreme cases (J Neurointervent Surg 2013; 5:e1).
The cavernous sinus can also be accessed via the inferior ophthalmic vein (J Neuroradiol 2012; 39:181).
Transfacial vein embolization via the internal jugular vein is an alternative approach for fistulas with anterior drainage (World Neurosurg 2015; 84:90).
- The facial vein can also be accessed by submandibular puncture (Neuro-Chirurgie 2014; 60:165).
- The facial vein, if tortuous, can be directly accessed by cutdown (J Clin Neuroscien 2014; 21:1238).
Options for fistula occlusion include platinum coils, fibrin glue, sclerosing agents, ethylene vinyl alcohol (onyx), bone wax, oxidized cellulose, stents, detachable balloons, and cyanoacrylate glue.
- Latex balloons filled with contrast material deflate within several weeks, sufficient time for closure of the fistula.
- Polymerizing agents in the latex balloon or other expansile materials risk compression of the 3rd, 5th,and 6th cranial nerves in the cavernous sinus and progressive neuropathy (Am J Neuroradiol 1991; 12:435).
If endovascular treatment fails, can revert to craniotomy (World Neurosurg 2012; 77:512).
Indications for treatment
Absolute
- Obstruction of cortical venous drainage
- Progressive optic neuropathy
Relative
- Intractable ophthalmoplegia
- Intractable chemosis/exposure keratopathy
Preventing and managing treatment complications
- Abducens nerve palsy is the most common complication after transvenous embolization of dural fistulas (Acta Neurochirurg 2014; 156:97).
- In a study of 73 patients treated from 1991 to 2012 abducens nerve palsy developed in 4 (5.5%) at 3–65 months after embolization (Acta Neurochirurg 2014; 156:97).
- Angle closure with elevated intraocular pressure has been observed after spontaneous closure of the fistula with thrombosis, and after embolization (BMC Ophthalmol 2012; 12:28).
- Challenges to transorbital embolization via the superior ophthalmic vein include fragility, bleeding, and small vein size (Ophthalmology 2006; 113:1220).
- Complications can include vision loss from ischemia, hemorrhage, and intracranial subarachnoid hemorrhage (J Neurointervent Surg 2013; 5:e1).
- The superior ophthalmic vein might be accessible, but clotted anteriorly, preventing cannulation (Ophthalmology 2006; 113:1220).
- The superior ophthalmic vein might be displaced deep into the orbit, making isolation and cannulation difficult (Ophthalmology 2006; 113:1220).
- Aneurysmal fistula from Ehlers-Danlos syndrome type IV is particularly difficult to treat because of vessel friability (BMJ Case Reports 2014, 2014).
- Stroke
- Recurrence
Disease-related complications
- Visual loss can have multiple etiologies.
- Corneal exposure and edema
- Glaucoma
- Venous stasis retinopathy with vitreous hemorrhage and proliferative retinopathy
- Optic neuropathy
- Exudative retinal detachment and choroidal effusion
- Oculomotor weakness and diplopia
- In a 2005-2013 study of 87 patients requiring balloon embolization for traumatic fistulas, oculomotor nerve function recovery time averaged 33 days (range 1–6 months) (J South Med Univ 2015; 35:244).
- Flow volume of the fistula negatively correlated with recovery time.
- Age, severity of preoperative palsy, and injury to treatment time positively correlated with recovery time.
- Intractable pain
References and additional resources
- AAO, Basic and Clinical Science Course. Section 5: Neuro-ophthalmology, 2013-2014.
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2013-2014.
- Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT: Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg 1985; 62:248.
- Brunel H, Girard N, Dufour H, et al. Submandibular puncture of the facial vein: an original route for endovascular therapy of carotid cavernous sinus dural fistulas. Neuro-Chirurgie 2014; 60:165.
- Cecchini MM, Levitt MR, Taneja M, et al. Embolization of carotid-cavernous fistula via direct percutaneous puncture of the inferior ophthalmic vein. J Neuroradiol 2012; 39:181.
- Debrun GM, ViníÄuela F, Fox AJ, Davis KR, Ahn HS: Indications for treatment and classification of 132 carotid-cavernous fistulas. Neurosurgery 1988; 22:285.
- de Keizer R: Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit 2003; 22:121.
- Ellis JA, Goldstein H, Connoly ES, Meyers PM: Carotid-cavernous fistulas. Neurosurg Focus 2012; 32:E9.
- Erickson BP, Johnson TE: A 32 year-old man with delayed onset post-traumatic proptosis and diplopia. J Emerg Med 2014; 46:475.
- Farley MK, Clark RD, Fallor MK, et al. Spontaneous carotid-cavernous fistula and the Ehlers-Danlos syndromes. Ophthalmology 1983; 90:1337.
- Gemmete JJ, Chaudhary N, Pandey A Ansari S: Treatment of carotid cavernous fistulas. Curr Treat Options Neurol 2010; 12:43.
- Keltner JL, Satterfield D, Dublin AB, Lee BCP: Dural and carotid sinus fistulas: Diagnosis, Management and Complications. Ophthalmology 1987; 94:1585.
- Kashiwazaki D, Kuwayama N, Akioka N, Kuroda S: Delayed abducens nerve palsy after transvenous coil embolization for cavernous sinus dural arteriovenoue fistulae. Acta Neurochirurg 2014; 156:97.
- Klevtsova E, Nguyen-Min C, Lalani T, et al. Posttraumatic carotid cavernous sinus fistula that presented as seizure and focal neurologic deficits with symptom resolution after therapeutic coil embolization. J Emerg Med 2015; 48:186.
- Kupersmith MJ, Berenstein A, Flamm E, Ransohoff J: Neuroophthalmic abnormalities and intravascular therapy of traumatic carotid cavernous fistulas. Ophthalmology 1986; 93:906.
- Leibovitch I, Modjtahedj S, Duckwiler GR, Goldberg RA: Lessons learned from difficult or unsuccessful cannulations of the superior ophthalmic vein in the treatment of cavernous sinus dural fistulas. Ophthalmology 2006; 113:1220.
- Leonard TJK, Moseley IF, Sanders MD: Ophthalmoplegia in carotid cavernous sinus fistula. Br J Ophthalmol 1984; 68:128.
- Luo CB, Teng MMH, Chang FC, et al. Transorbital direct puncture of the cavernous sinus through the internal carotid artery for embolization of isolated cavernous sinus dural arteriovenous fistula. J Neurointervent Surg 2013; 5:e1.
- Luo CB, Chang FC, Teng MMH, Ting WW: Anatomic variation of facial vein in carotid-cavernous sinus fistula and trans-facial vein embolization. World Neurosurg 2015; 84:90.
- Michels KS, Ng JD, Falardeau J: Transvenous embolization of a dural carotid-cavernous sinus fistula via the inferior opthalmic vein. Ophthalmic Pl Reconstr Surg 2007; 23: 480.
- Monsein LH, Debrun GM, Miller NR, et al. Treatment of dural carotid-cavernous sinus fistulas via the superior ophthalmic vein. Am J Neuroradiol 1991; 12:435.
- Nakagawa I, Park HS, Wada T, et al. A novel approach to the treatment of direct carotid-cavernous fistula in a patient with Ehlers-Danlos syndrome type IV. BMJ Case Reports 2014, 2014.
- Nakagawa S, Murai Y, Wada T, Tateyama K: 4D flow preliminary investigation of a direct carotid cavernous sinus fistula due to a ruptured intracavernous aneurysm. BMJ Case Reports 2015, 2015.
- Parkinson D: Transcavernous repair of carotid cavernous fistula. Case report. J Neurosurg 1967; 26:420.
- Parkinson D: Lateral sellar compartment: history and anatomy. J Craniofac Surg 1995; 6:55.
- Rodrigues T, Willinsky R, Agid R, et al. Management of dural carotid cavernous fistulas: a single-centre experience. Eur Radiol 2014; 24:3051.
- Satchi K, Mitchell PJ, McNab AA: Transorbital puncture of the cavernous sinus to treat a dural carotid-cavernous sinus fistula. Ophthalmic Pl Reconstr Surg 2009; 25: 54.
- Thiex R, Gross BA, Gupta R, et al. Transvenous approach to carotid-cavernous fistula via facial vein cutdown. J Clin Neuroscien 2014; 21:1238.
- Thinda S, Melson MR, Kuchtey RW: Worsening angle closure glaucoma and choroidal detachments subsequent to closure of a carotid cavernous fistula. BMC Ophthalmol 2012; 12:28.
- Uflacker R, Lima S, RIbas GC, Piske RL: Carotid-cavernous fistulas: embolization through the superior ophthalmic vein. Radiology 1986; 159:175.
- Winslow J: Exposition Anatomique de la Structure du Corps Humain. London: Prevast, Vol II, 1734.
- Yeung SW, Suen SS, Yu SS, et al. Spontaneous carotid cavernous sinus fistula complicating pregnancy. Hong Kong Med J 2013; 19:258.
- Zanaty M, Chalouhi N, Tjoumakaris SI, et al. Endovascular treatment of carotid-cavernous fistulas. Neurosurg Clin N Am 2014; 25:551.
- Zheng C, Shu H, Tang K, et al. Factors affecting oculomotor nerve function recovery time following balloon embolization of oculomotor nerve palsy caused by traumatic carotid cavernous sinus fistula. J South Med Univ 2015; 35:244.
