Corneal Neurotization
Updated July 2024
Goals
- Primary goals of the procedure are to re-establish corneal sensibility, integrity, and blink reflex by
- Transferring an intact sensory donor nerve to the corneoscleral limbus
- Secondary goals of the procedure are minimizing donor site morbidity and optimizing cosmesis by
- Use of sensory donor nerves that impose minimal sensory disturbance at their respective dermatomes
- Use of sensory donor nerves that have a quick sensory recovery in their respective dermatome
- Use of minimally invasive techniques with camouflaged incision placement
Indications & Contraindications
- Indications
- Neurotrophic keratopathy (NK) with secondary corneal injury
- Etiology of NK may be central (e.g., trigeminal nerve injury due to tumor, surgery, trauma, congenital, etc.) or local (e.g., herpetic corneal infections, ocular surgery, contact lens overuse, retinal laser, topical medications, etc.)
- Neurotrophic keratopathy (NK) with secondary corneal injury
- Contraindications
- Relative
- Extensive conjunctival scarring (e.g., multiple prior ocular procedures, quiescent cicatrizing conjunctivitis, chemical burns, etc.)
- Poorly controlled diabetes mellitus, other systemic immunosuppression, and poor systemic health
- Bleeding diathesis (e.g., coumadin, high dose aspirin, low molecular weight heparin, blood clotting abnormalities, etc.)
- Unrealistic expectations of surgical outcome by the patient (e.g., immediate recovery, “perfect” postoperative vision, etc.)
- Glaucoma drainage device or filtering bleb
- Absolute
- Active inflammatory or infectious ocular and eyelid conditions (e.g., active ocular cicatricial pemphigoid, active infectious conjunctivitis, scleritis, keratitis, cellulitis, skin disorders, etc.)
- Ongoing external beam radiation therapy to the orbit or the eye
- Perineural spread of malignancy into the orbit/skull base
- Absence of healthy sensory donor nerves
- Inability to tolerate general anesthesia
- Relative
Pre-procedure evaluation
- Patient history
- Etiology of defect
- Denervation time
- Prior surgical and medical interventions
- History of eyelid facial, intracranial surgery or trauma
- History of periorbital cutaneous and other malignancies
- History of radiation
- Medical co-morbidities and systemic health
- History of skin or cutaneous disease or disorders
- Current medications, particularly anticoagulants
- Clinical examination
- Comprehensive eye and adnexal examination
- Measurement of corneal sensibility in 4 peripheral quadrants and centrally (preferably with an aesthesiometer such as Cochet-Bonnet) and blink reflex
- Evaluation of sensory donor nerve function by light touch, monofilament test, or 2-point discrimination tests (i.e., ipsilateral and contralateral trigeminal nerve function)
- Preoperative assessment
- Anterior segment photography and in vivo confocal microscopy
- Medical clearance for general anesthesia
- Nerve Selection
- Check sensation V1 – V3 and sensation along behind the ear to assess greater auricular nerve and in front of the ear to assess the auiculotemporal nerve
- Depending on the etiology and the patient’s sensation, you will have to decide contralateral versus and ipsilateral nerve
- If there is no sensation on that side in V1-V3, you may need to use the ipsilateral greater auricular nerve or contralateral transfer
Alternatives to the procedure
- Temporizing medical treatments (e.g., ocular lubrication, antibiotic drops, autologous serum drops, topical neurotrophic factors, bandage contact lenses, etc.)
- Temporizing surgical/interventional treatments (e.g., amniotic membrane grafting, tarsorrhaphy, ptosis induction by botulinum toxin A injection, conjunctival flaps)
Available techniques
Coronal technique (utilized with intact ipsilateral or contralateral supraorbital and/or supratrochlear nerves)
- Procedure is performed under general anesthesia
- Generous tumescent solution (2 ampules of 1:1000 adrenaline diluted in 1000ml of normal saline) is infiltrated into the entire forehead and anterior hair baring scalp
- Lidocaine 1% with 1:100,000 dilution of epinephrine is infiltrated into the upper eyelid crease incision on the affected eye
- A coronal incision is made behind the hairline from ear to ear or from midline to the ipsilateral ear (hemicoronal) in case of ipsilateral nerve harvest
- Dissection is carried in subgaleal plane to the superior orbital rims (for contralateral nerve transfer) or to the ipsilateral orbital rim (for ipsilateral nerve transfer)
- Supraorbital and/or supratrochlear nerves are then dissected and reflected inferiorly under either loop or microscopic magnification from the subgaleal tissue with care taken to avoid injury to the nerves and maintain hemostasis
- Approximately 4-10 cm of the nerve length can be dissected depending on the need (e.g., ipsilateral vs contralateral transfer) and patient’s anatomy
- Next an eyelid crease incision is made on the recipient side and the nerve branches are tunneled into the incision
- A blepharotomy is created medial to the medial horn of the levator aponeurosis and the nerve branches are further tunneled into the superior medial conjunctival fornix. Alternatively, Wright fascia needle passed through the same location can be used to tunnel the nerve branches into the conjunctival fornix
- An operating microscope is then brought into the surgical field
- Any adipose and connective tissue is carefully dissected off the nerve branches
- Next, a conjunctival incision is made approximately 7-8mm above the 12 o’clock corneoscleral limbus
- Dissection is carried through the tenon’s fascia and a wide upside down “V” tunnel is created to the corneoscleral limbus
- Additional conjunctival incisions are created at 3 and 9o’clock positions 1-2 mm from the corneoscleral limbus or a conjunctival peritomy may be performed
- The nerve branches are then retrieved through these incisions (or through the peritomy) and can be placed at 3 and 9 o’clock
- The epineurium of the nerve branches is then secured to the sclera with either fibrin glue or an interrupted 9-0 polyglactin or nylon sutures
- The conjunctival, eyelid crease, and scalp incisions are then closed in a standard fashion
- Either a temporary or permanent tarsorrhaphy is performed in most cases depending on the severity of corneal injury
Endoscopic technique (utilized with intact ipsilateral or contralateral supraorbital and/or supratrochlear nerves)
- Procedure is performed under general anesthesia
- Generous tumescent solution (2 ampules of 1:1000 adrenaline diluted in 1000ml of normal saline) is infiltrated into the area of the forehead and anterior hair baring scalp along the course of the donor supraorbital or supratrochlear nerve
- Lidocaine 1% with 1:100,000 dilution of epinephrine is infiltrated into the upper eyelid crease incision on the affected eye (in case if ipsilateral donor nerve is used) or both upper eyelid creases (in case if contralateral donor nerve is used)
- An eyelid crease incision is then made on the side of the donor nerve
- Dissection is then carried deep to the orbicularis muscle lateral to the supraorbital notch to the supraorbital rim
- Periosteum is then incised, and dissection is carried medially in the subperiosteal plane to the supraorbital notch
- Once the supraorbital neurovascular bundle is identified the vessels are gently separated from the nerve and obliterated with either gentle bipolar cautery or sutures
- Dissection is then carried cephalad with long Steven tenotomy scissors by making relaxing periosteal incisions along the course of the supraorbital nerve and releasing the anterior surface of the nerve from the subgaleal tissues
- A muscle hook can be used to place gentle inferior traction on the nerve
- Once approximately 2 cm of nerve is dissected under direct visualization an endoscope is brought into the surgical field
- A 30 or 0 degree endoscope is used with a brow lift sheath to assist in retracting the scalp
- Dissection is then carried further superiorly under endoscopic visualization. At that point branching of the nerve is seen and each branch is dissected separately
- If contralateral nerve transfer is necessary 2 small (1-1.5 cm ) radial scalp incisions behind the hairline are made at the level of the lateral and medial canthi. This allows to harvest a longer segment of the nerve (>4cm)
- Dissection is carried from these incisions in the subgaleal plane which is then joined with the subperiosteal plane created from the upper eyelid crease incision
- The nerve branches are then severed at the desired length(e.g., approximately 4 cm for the ipsilateral and 8-10 cm for the contralateral transfer)
- Next an eyelid crease incision is made on the ipsilateral side and the nerve branches are tunneled into the incision
- If contralateral transfer is needed another eyelid crease incision is made on the affected side and a hemostat is used to tunnel the nerve branches across nasal bridge in the subgaleal plane
- A blepharotomy is created medial to the medial horn of the levator aponeurosis on the affected side and the nerve branches are further tunneled into the superior medial conjunctival fornix. Alternatively, Wright fascia needle passed through the same location can be used to tunnel the nerve branches into the conjunctival fornix
- An operating microscope is then brought into the surgical field
- Any adipose and connective tissue is carefully dissected off the nerve branches
- Next, a conjunctival incision is made approximately 7-8mm above the 12 o’clock corneoscleral limbus
- Dissection is carried through the tenon’s fascia and a wide upside down “V” tunnel is created to the corneoscleral limbus
- Additional conjunctival incisions are created at 3 and 9 o’clock positions 1-2 mm from the corneoscleral limbus or a conjunctival peritomy may be performed
- The nerve branches are then retrieved through these incisions (or peritomy) to encircle the entire corneoscleral limbus (or at least reach 3 and 9 o’clock positions depending on the available donor nerve length)
- The epineurium of the nerve branches is then secured to the sclera with fibrin glue or either an interrupted 9-0 polyglactin or nylon sutures
- The conjunctival, eyelid crease, and scalp incisions are then closed in a standard fashion
- Either a temporary or permanent tarsorrhaphy is performed in most cases depending on the severity of corneal injury (e.g., presence of an epithelial defect, etc.)
Nerve graft technique with supraorbital or supratrochlear nerve
- Lidocaine 1% with 1:100,000 dilution of epinephrine is infiltrated into the upper eyelid crease incision on the affected eye (in case if ipsilateral donor nerve is used) or both upper eyelid creases and across the glabella (in case if contralateral donor nerve is used)
- An eyelid crease incision is then made on the side of the donor nerve
- Dissection is then carried deep to the orbicularis muscle lateral to the supraorbital notch to the supraorbital rim
- Periosteum is then incised, and dissection is carried medially in the subperiosteal plane to the supraorbital notch
- Once the supraorbital and/or supratrochlear neurovascular bundle is identified the vessels are gently separated from the nerve and obliterated with either gentle bipolar cautery or sutures
- Dissection is then carried cephalad with long Steven tenotomy scissors by making relaxing periosteal incisions along the course of the supraorbital nerve and releasing the anterior surface of the nerve from the subgaleal tissues
- A muscle hook can be used to place gentle inferior traction on the nerve
- Once approximately 1-2 cm of nerve segment is dissected the distal nerve is sharply transected and reflected inferiorly through the eyelid crease incision
- Alternatively, an epineurial window is created within the visible nerve segment
- Concurrently a nerve graft may be harvested by another team (if autograft is used) or alternatively, a decellularized nerve allograft may be used (1-2mm by 7cm) (Avance graft by AxoGen, Alachua, FL)
- A nerve graft with at least 7 cm length for contralateral transfer and 4 cm for unilateral transfer should be used
- A blepharotomy is created medial to the medial horn of the levator aponeurosis on the affected side and the nerve graft is further tunneled into the superior medial conjunctival fornix. Alternatively, Wright fascia needle passed through the same location can be used to tunnel the nerve graft into the conjunctival fornix
- An operating microscope is then brought into the surgical field
- Next, a conjunctival incision is made approximately 7-8mm above the 12 o’clock corneoscleral limbus.
- Dissection is carried through the tenon’s fascia and a wide upside down “V” tunnel is created to the corneoscleral limbus.
- Additional conjunctival incisions are created at 3 and 9 o’clock positions 1-2 mm from the corneoscleral limbus or a conjunctival peritomy may be performed
- The nerve allograft is then tunneled in subtenons plane from the superior bulbar conjunctival incision into the 12 o’clock incision.
- At that point, the epineurium is opened and nerve fascicles are released distal to the 12 o’clock incision.
- Usually 2-6 fascicles are available. Each is tunneled to encircle the entire corneoscleral limbus (or at least reach 3 and 9 o’clock incisions depending on the available donor nerve length).
- The perineurium of the nerve branches is then secured to the sclera with either an interrupted 9-0 polyglactin or nylon sutures or fibrin glue.
- An epineurial neurorrhaphy should be done at the end of the case. In the end to end or side to end fashion is then performed between the donor nerve and the nerve graft using interrupted 9-0 or 10-0 nylon sutures
- Alternatively, the coaptation maybe performed with a nerve connector or wrap
- Inset of the nerve graft around corneoscleral limbus maybe performed prior to neurorrhaphy if there is concern for undue tension at the site of anastomosis
- If contralateral transfer is needed another eyelid crease incision is made on the affected side and a hemostat or Wright fascia needle is used to tunnel the nerve graft across nasal bridge in the subgaleal plane into the incisionThe conjunctival and eyelid crease incisions are then closed in a standard fashion
- Either a temporary or permanent tarsorrhaphy is performed in most cases depending on the severity of corneal injury (e.g., presence of an epithelial defect, etc.)
Nerve graft technique with infraorbital nerve
- After the induction of general anesthesia, the inferior conjunctival fornix on the donor side is infiltrated with lidocaine 2% with 1:100,000 dilution with epinephrine
- Patient’s face is then prepped and draped in a standard fashion of oculofacial surgery
- An inferior conjunctival fornix incision is created with a monopolar cautery
- Dissection is carried to the infraorbital rim and the periosteum is reflected off the orbital floor to expose the roof of the infraorbital canal
- A small osteotome is used to unroof the infraorbital canal and the nerve is carefully elevated superiorly with a 4-0 silk suture
- An epineurial window is created and a nerve graft (either allograft or autograft) is coapted in the end to side fashion.
- The nerve graft is then retrieved from the fornix incision.
- Additional conjunctival incisions are created at 3 and 9 o’clock positions 1-2 mm from the corneoscleral limbus or a conjunctival peritomy may be performed
- The graft is tunneled to the 6 o’clock limbal conjunctival incision
- Epineurium is then opened and nerve fascicles are released and tunneled and secured around the cornea at 3 and 9, positions in the same fashion as in the previously described techniques.
- Either a temporary or permanent tarsorrhaphy is performed in most cases depending on the severity of corneal injury (e.g., presence of an epithelial defect, etc.)
Nerve graft technique with greater auricular nerve
- A preauricular modified Blair incision is made
- Dissection occurs until the branches of the greater auricular nerve are identified
- A supraparotid dissection is carried and tunneld to the inferior conjunctival fornix
- A sural nerve is typically harvested due to the length of donor nerve required
- tunnel to the lateral left inferior conjunctival fornix
- The sural nerve graft if harvested to the inferior fornix
- The fassicles are separated and fixated onto the globe
- End-to-end anastomosis of the greater auricular nerve to the sural nerve is performed
- A lateral temporary or permanent tarsorrhaphy is performed
Ongoing controversies
- It is unclear which technique results in higher success rate in restoration of corneal sensibility and epithelial integrity
- The author’s preferred donor nerve is ipsilateral supraorbital or supratrochlear nerve if sensation in the respective dermatome is intact (tested by either light touch, monofilament, or 2 point discrimination test and compared to the contralateral side). End to End connection may provide a stronger connection than end to side
- Next preferable donor is ipsilateral infraorbital nerve and then contralateral supraorbital or supratrochlear nerve
- Other potential donors if none of these are available may include auriculotemporal and greater auricular
- It is unclear if using nerve autograft, allograft, or direct nerve transfer results in more successful outcomes. An advantage of decellularized nerve allograft over direct harvest of the donor nerve, with either endoscopic or coronal approach, include less operative time and learning curve, less technical equipment and instrumentation, and potentially less morbidity. The advantage of the nerve allograft over nerve autograft includes less operative time, no secondary donor site morbidity, better graft to donor size match (there are many diameters of the allograft available). The disadvantages of nerve allograft include cost, length limit (max length is 7cm), and theoretical risk of rejection.
- It is unclear if incorporating more nerve fascicles/branches results in better surgical outcomes
- Many surgeons have simplified this technique to do 2 fascicles nasal and temporal and use fibrin glue for fixation
- The exact mechanism for corneal neurotization is not clear (i.e., regeneration of the existing corneal nerves due to paracrine support from the donor nerve vs. axonal ingrowth into the cornea from the donor nerve)
- It is unclear if side to end neurorrhaphy in adults is as effective as it is in children in restoring corneal sensibility. Children tend to regain sensation better than adults.
Patient management: treatment and follow-up
- Postoperative instructions
- This is generally an outpatient procedure
- Standard postoperative eyelid/forehead surgery instructions are given. If nerve autograft is harvested the donor site is dressed in the standard fashion and patients are given additional standard instructions for its care. Any eye/forehead dressings are removed the next day.
- Postoperative medications
- Topical antibiotic drops are used 2 times daily for 1 week and topical ophthalmic antibiotic ointment 2 times a day for 1 week to the eyelid incisions
- Narcotic pain medicine and short steroid taper maybe prescribed
- Postoperative follow up
- Patients are seen in the first 1-3 days postoperatively
- Common response to treatment, follow-up, and secondary treatment
- Improvement in corneal sensibility is seen in most patients with its magnitude and rate likely dependent on several factors including patient’s specific etiology of NK, systemic health, age, surgical technique, and length of the graft (if nerve graft is used) among other factors
- In patients with ipsilateral donor nerve transfer improvement in corneal sensibility and epithelial integrity maybe seen as early as 2 – 4 months postoperatively.
- In patients with contralateral donor nerve transfer improvement in corneal sensibility and epithelial integrity maybe seen as early as 2 – 6 months postoperatively.
- Frequently, corneal epithelial integrity and ocular surface improvements occur before any notable improvement in corneal sensibility
- It is likely that the full effect of the procedure takes as long as 2 years to manifest
- Secondary treatment may include continued supportive medical and surgical therapy to maintain corneal integrity until adequate restoration of protective corneal sensibility
Surgical complications, prevention, and management
- Neuroma formation at the site of neurorrhaphy (if nerve graft is used) or at the site of ocular inset. Prevention includes sound surgical technique, minimizing tension and crush injury to the axons, and gentle handling of nerve tissue. Treatment may include observation only or excision if symptomatic.
- Hematoma or seroma formation. If expanding hematoma, evacuation is urgent to avoid skin necrosis or vision loss (if in the orbit).
- Donor site morbidity at the donor nerve harvest. Numbness and paresthesia at the site of donor nerve (e.g., supraorbital, supratrochlear) is usually temporary and resolves within weeks to months regardless of the technique used. It is possible that loss of skin sensation at the donor dermatome maybe permanent, but so far has not been reported.
- Donor site morbidity at the site of autograft harvest. Complications at the site of nerve autograft harvest (e.g., sural nerve) may include permanent loss of protective sensibility at the lateral malleolus, unsightly scarring, neuroma formation, infection, and pain.
- Scarring at the incision sites and areas of dissection. Visible scarring is minimized by cosmetic incision placement (e.g., eyelid crease), gentle tissue handling, and sound surgical technique.
- Postoperative infection at the surgical site. Infections of the soft tissues or the eye are rare. Treatment usually includes topical and systemic antibiotics, and drainage of any abscess or fluid collection.
- Ocular complications and vision loss. Corneal or scleral perforation, ocular infections, and vision loss have not been reported to date, but remain a possibility with any ocular surgery. Treatment would depend on the location and the type of ocular complication.
- Ptosis or other eyelid malpositions. Eyelid malpositions are possible with any surgery involving eyelids. Most eyelid malpositions are initially treated conservatively by observation for 6-12 months. Surgical intervention would be needed to correct the malposition beyond that period or if significant corneal injury occurs before that period.
- Alopecia. Hair loss at the site of the incision may be seen with coronal or endoscopic techniques. This complication maybe reduced by proper incision design, beveling any coronal incision, conservative cautery, minimizing tension on wound closure, and gentle tissue handling. Significant hair loss is more common with coronal approach and less likely to occur with endoscopic technique.
- Injury to the frontal branch of the facial nerve. This complication may occur if the subgaleal plane is violated during the dissection. Coronal approach poses the highest risk given the needed dissection through the temporal line of fusion. Observation is usually indicated as the nerve may regenerate.
Disease-related complications
- Persistent corneal epithelial defects
- Corneal ulceration
- Corneal neovascularization
- Corneal scarring and thinning
- Corneal perforation
- Endophthalmitis
- Loss of the eye
Historical perspective
- Terzis et al. first described corneal neurotization in 2009. Six patients in their study with ipsilateral trigeminal nerve palsy underwent re-innervation of the cornea, via a coronal approach, with the contralateral supraorbital and supratrochlear branches of the ophthalmic division of the trigeminal nerve.
- Subsequently, in 2014, Elbaz et al. described a technique of using nerve autograft (sural nerve) anastomosed to either an ipsilateral or contralateral supratrochlear nerve and tunneled through the upper eyelid incision avoiding a coronal incision.
- In 2018 Leyngold et al. described endoscopic technique for corneal neurotization.
- In 2018 Leyngold et al. also described case series of patients who have successfully undergone corneal neurotization with nerve allograft coapted to either supratrochlear, supraorbital, or infraorbital nerves.
- In addition, since the first description of the procedure, both morphological (in vivo confocal microscopy of the cornea) and histological proof of recovered corneal innervation have been published by several authors.
References and additional resources
- Elbaz U, Bains R, Zuker RM, Borschel GH, Ali A. Restoration of Corneal Sensation With Regional Nerve Transfers and Nerve Grafts: A New Approach to a Difficult Problem. JAMA ophthalmology. Jul 10 2014.
- Bains RD, Elbaz U, Zuker RM, Ali A, Borschel GH. Corneal neurotization from the supratrochlear nerve with sural nerve grafts: a minimally invasive approach. Plast ReconstrSurgery. Feb 2015;135(2):397e-400e.
- Flores LP, Martins RS, Siqueira MG. Clinical results of transferring a motor branch of the tibial nerve to the deep peroneal nerve for treatment of foot drop. Neurosurgery. Oct 2013;73(4):609-615; discussion 615-606.
- Terzis JK, Dryer MM, Bodner BI. Corneal neurotization: a novel technique for the anesthetic cornea. Cornea. Jul 2010;29(7):812-819.
- Allevi F, Fogagnolo P, Rossetti L, Biglioli F. Eyelid reanimation, neurotisation, and transplantation of the cornea in a patient with facial palsy. BMJ case reports. 2014;2014.
- Lau, N. , Osborne, S. , Vasquez-Perez, A. , Wilde, C. , Manisali, M. & Jayaram, R. (2022). Corneal Neurotization Using the Great Auricular Nerve for Bilateral Congenital Trigeminal Anesthesia. Cornea, 41 (5), 654-657.
- Leyngold IM, Weller CM, Leyngold MM., Tabor, M. Endoscopic Corneal Neurotization: Technique and Initial Experience. Ophthalmic Plastic & Reconstructive Surgery. 2018 Jan/Feb;34(1):82-85
- Jacinto F, Espana E, Padilla M, Ahmad A, Leyngold I. Ipsilateral supraorbital nerve transfer in a case of recalcitrant neurotrophic keratopathy with an intact ipsilateral frontal nerve: A novel surgical technique. Am J Ophthalmol Case Reports (4) 2016: 14-17
- Leyngold IM, Tabor M, Leyngold MM, Espana E. Endoscopic Corneal Neurotization: Cadaver Feasibility Study. Ophthalmic Plastic & Reconstructive Surgery. 2018 May/Jun;34(3):213-216.
- Leyngold IM, Yen M, Tian J, Vora G, Leyngold M, Weller CM. Minimally invasive corneal neurotization with decellularized nerve graft: technique and clinical outcomes. Ophthalmic Plastic & Reconstructive Surgery. 2018, Jul 24. Epub ahead of print
- Benkhatar H, Levy O, Goemaere I, Borderie V, Laroche L, Bouheraoua N. Corneal Neurotization With a Great Auricular Nerve Graft: Effective Reinnervation Demonstrated by In Vivo Confocal Microscopy. Cornea. 2018 Feb 22. [Epub ahead of print]
- Green et al., Green’s Operative Hand Surgery. Fifth Addition. Volume 1Chapter 30 pg 1085 – 1098
Endoscopic technique photos and videos
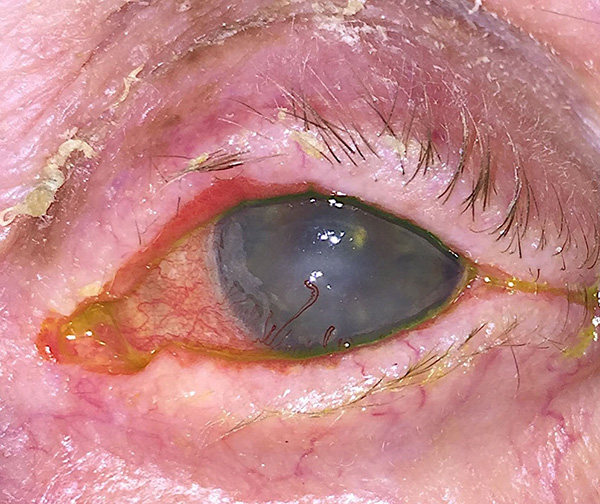
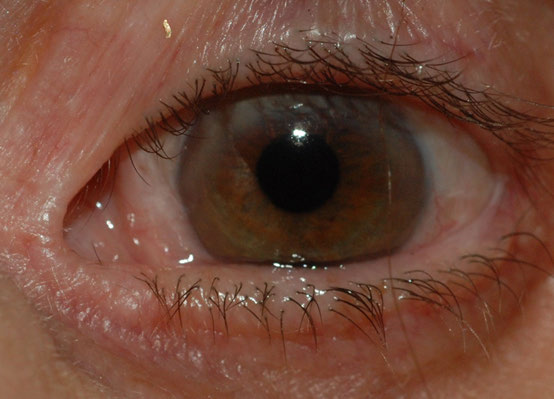
Figure 1. Persistent epithelial defect in the patient with neurotrophic keratopathy (surgeon’s view)

Figure 2. Scalp incisions for the endoscopic approach
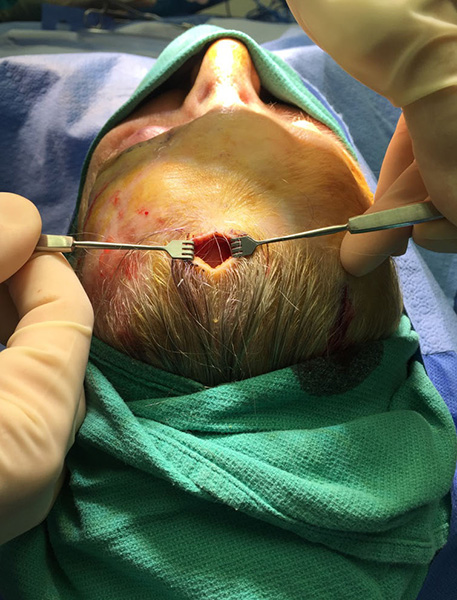
Figure 3a. Endoscopic dissection of the supraorbital nerve from the eyelid (a) and scalp (b) incisions.

Figure 3b
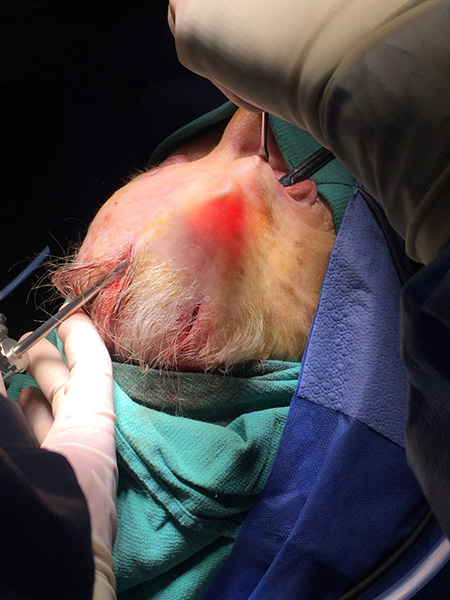
Figure 3c. Supraorbital nerve being harvested under endoscopic visualization
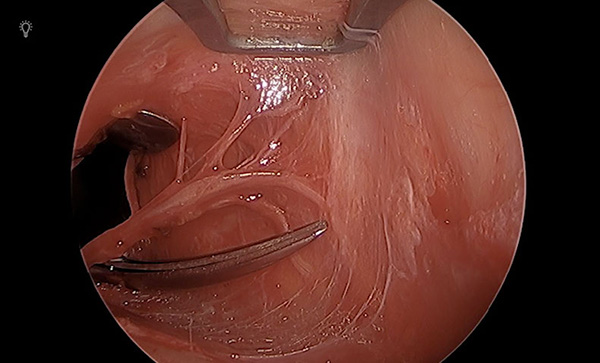
Figure 4a. Supraorbital nerve delivered through the palpebral incision (a) and tunneled to the contralateral side (b,c).and through the blepharotomy incision (d).

Figure 4b

Figure 4c

Figure 4d

Figure 5. Supraorbital nerve transferred to the sub-Tenon’s space of the affected eye.
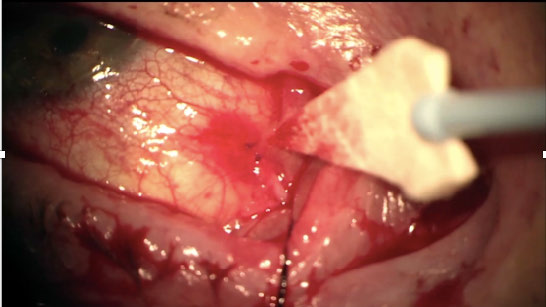
Figure 6. Complete closure of the persistent corneal epithelial defect 5 weeks after endoscopic neurotization.
Video: Endoscopic dissection of distal supraorbital nerve branches
Video: Ipsilateral endoscopic corneal neurotization
Coronal technique photos
Figure 1. Pre-operative photograph at initial presentation showing conjunctival injection, corneal opacification, and peripheral neovascularization (BCVA 20/200).

Figure 2. Intraoperative photograph of an isolated supraorbital nerve.
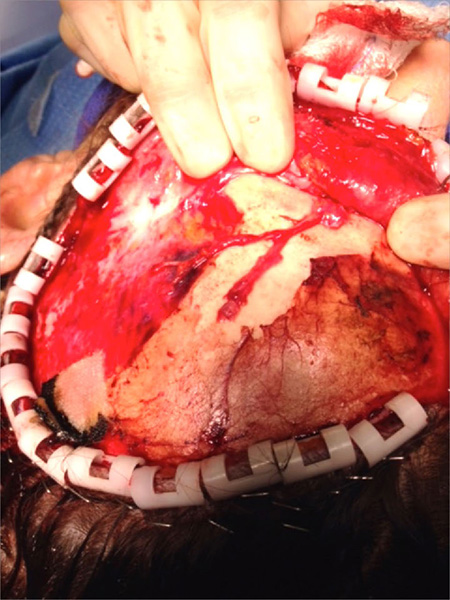
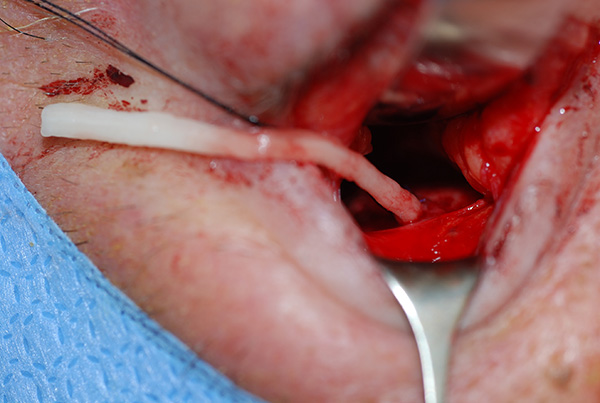
Figure 3. An intraoperative photograph showing supraorbital nerve branches tunneled through an upper eyelid crease incision.
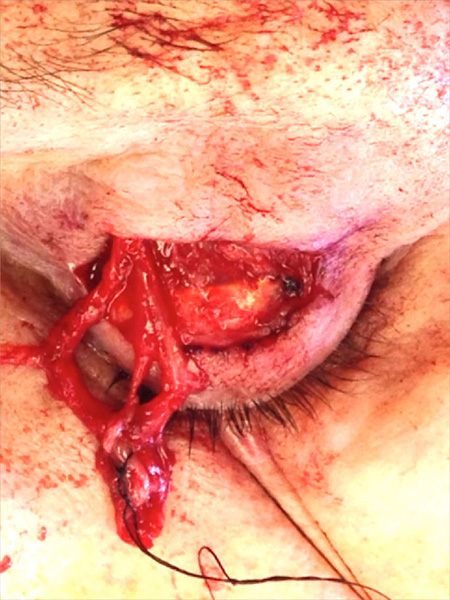
Figure 4. At 8 month postoperative follow up there is resolution of corneal opacification, improvement of corneal sensation, and visual acuity. Medially, a branch of the supraorbital nerve is seen deep to the bulbar conjunctiva (arrow).
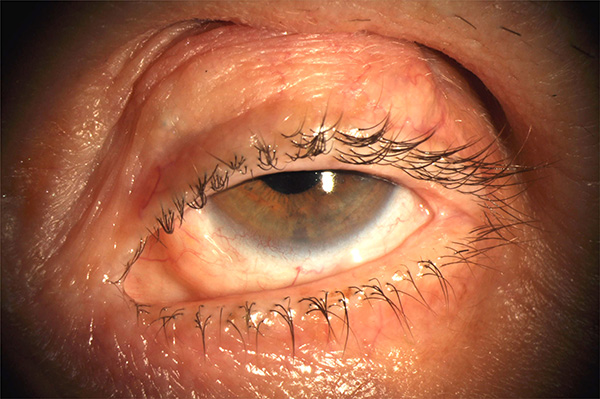
Figure 5. At a 2-year postoperative follow up the cornea remains clear with intact sensation (BCVA: 20/30).
Nerve graft technique photos and videos
Figure 1. Marking for contralateral transfer of the either a supraorbital or supratrochear nerve. A higher crease is marked on the donor side (left upper eyelid) and the approximate locations of the sensory donor nerves is marked with small vertical lines. Natural eyelid crease is marked on the recipient side (right upper eyelid).
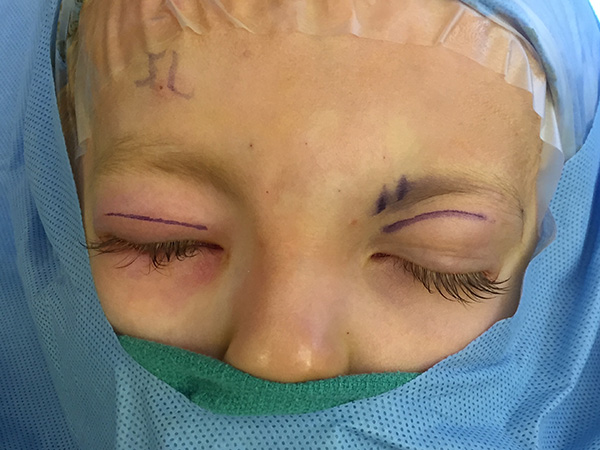
Figure 2. Isolated supraorbital nerve segment severed approximately 2 cm from the supraorbital notch.
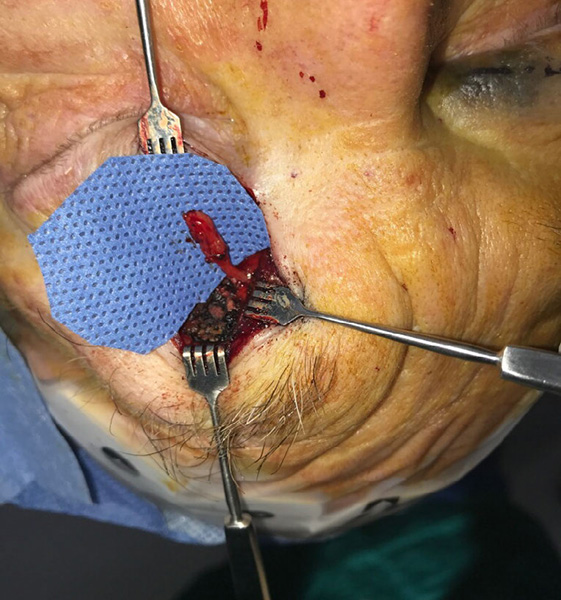
Figure 3. Coaptation between neve allograft (long arrow) and supraorbital nerve (short arrow).
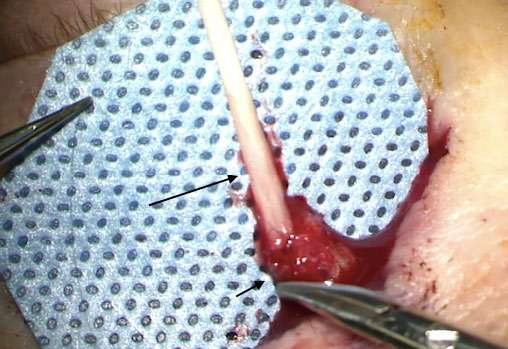
Figure 4. (a) In case of contralateral transfer, a large hemostat tunneled in subgaleal plane from the recipient side is used to retrieve the nerve allograft via a 4-0 silk suture attached to epineurium of the graft (b) Nerve allograft tunneled to the upper eyelid crease incision on the recipient side.


Figure 5. (a) A hemostat is tunneled through the blepharotomy incision to retrieve the graft. (b) The epineurium is the incised and the fascicle are released on the ocular surface. (c) A conjunctival incision is the created 7-8mm above 12 o’clock limbus and the fascicles are tunneled in the subconjunctival pane around the superior limbus.

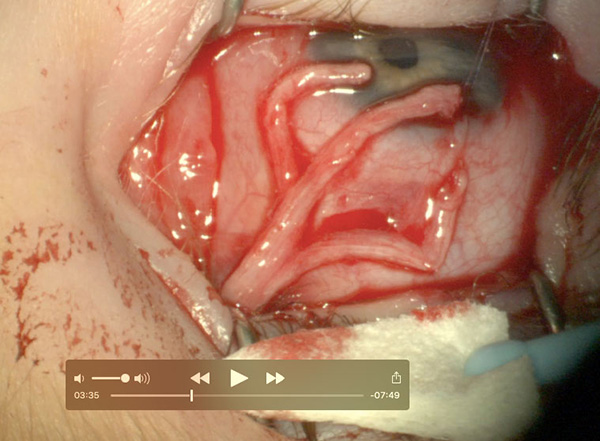

Figure 6. Appearance of the nerve allograft and ocular surface at postoperative month 2 after corneal neurotization using contralateral supraorbital nerve (left) in primary gaze (right) in infraduction.
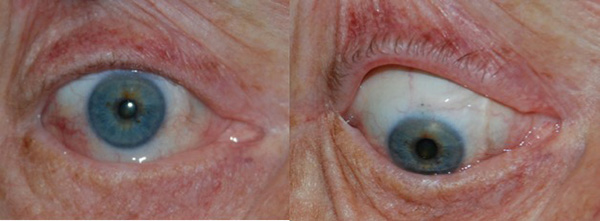
Figure 7. A representative in vivo confocal micrograph showing paucity of corneal anterior stromal nerves before (left) and after (right) corneal neurotization. Arrows point at the corneal stromal nerves.
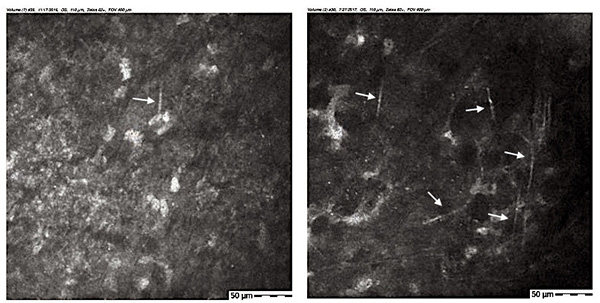
Figure 8a. The infraorbital groove is unroofed and the infraorbital nerve is isolated.
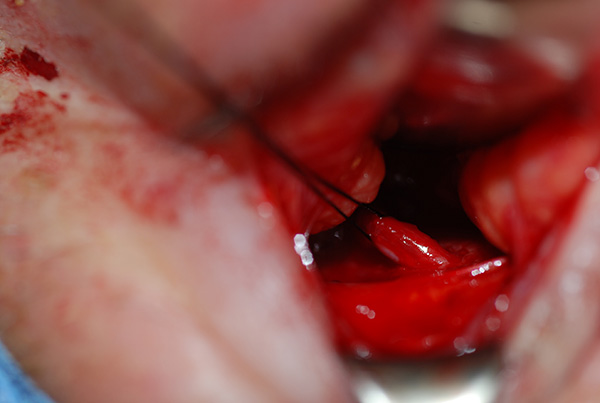
Figure 8b. Side-to-end coaptation of the nerve allograft to the infraorbital nerve.
Video: Contalateral Neurotization with allograft
Video: Ipsilateral Corneal neurotization with infraorbital nerve (side to end coaptation with nerve allograft)
Video: Ipsilateral Corneal neurotization with infraorbital nerve (inset)
Video: Ipsilateral Corneal neurotization with nerve allograft
