Dacryocystectomy
Updated July 2024
Goals, indications, contraindications
Goals
Primary
- Removal of lacrimal sac
- Removal of lacrimal sac tumor
Secondary
- Prevent further episodes of dacryocystitis
Indications
- Suspected or confirmed lacrimal sac tumor
- Chronic dacryocystitis following failed dacryocystorhinostomy (DCR)
- Dacryocystitis without a history of epiphora
- Dacryocystitis in setting of chronic dry eye syndrome (DES)
- Dacryocystitis in patients with high risk of anesthesia in an effort to avoid need for further surgery
- Patients who are unable to tolerate potential side effects of nasal packing such as, tachycardia and hypertension
- Dacryocystitis in setting of granulomatosis with polyangiitis (Wegeners granulomatosis) that is refractory to conventional management
Contraindications
Relative
- Primary treatment of nasolacrimal duct obstruction that do not fall into the above mentioned categories
- Lacrimal sac tumor that has extended beyond the sac where en bloc or further resection is necessary
Preprocedure evaluation
Complete history with particular attention to
- Epiphora
- Ocular surface disease and DES
- History of cancer, particularly sinus or facial
- Presence of bloody tears
- Palpable masses in the medial canthal region
- Prior lacrimal surgery
- Facial trauma
- Aspirin/Anti-coagulant therapy
- History of systemic rheumatologic disease
Clinical examination
- Complete periorbital and anterior segment examination
- Assess for DES including evaluation of tear lake, tear break up time, and basic secretion testing.
- Complete lacrimal evaluation with probing and irrigation
- Lacrimal sac tumor suspected
- Orbital evaluation including measurement of exophthalmometry
- Motility evaluation
- Palpate lacrimal sac and look for purulent or sanguineous reflux from punctum
- Examine for fullness of lacrimal sac extending superior to the medial canthal tendon
- Intranasal exam with endoscope or speculum looking for nasal extension
Imaging
- Indicated for suspected lacrimal tumors to determine extent and characteristics of the lesion
- In cases of severe dacryocystitis, imaging can also be useful to determine presence of orbital extension or abscess
- Imaging options
- Computed tomography (CT) of the orbit and sinuses (Figure 1)
- Magnetic resonance imaging (MRI) of the orbit and sinuses
- Dacryocystography
- Radionuclide dacryoscintigraphy

Figure 1. CT of orbit and sinuses.
Procedure alternatives
Chronic dacryocystitis
- Observation
- Medical treatment of dacryocystitis
- Primary or repeat external or endoscopic DCR
- +/- Mitomycin C
- +/- Silastic intubation
Suspected tumor
- Palliative radiation and/or chemotherapy following lesion biopsy
- En bloc resection
Surgical techniques
Anesthesia
- Monitored anesthesia care (MAC)
- Local anesthesia infiltration to medial canthal region
- i.e., 50/50 mixture of 2% lidocaine with epinephrine and 0.5% Marcaine with epinephrine
- Typically provides adequate anesthesia given that there is no bone removal and decreased risk of aspiration compared to DCR
- General anesthesia
- If unable to tolerate MAC
- Possibility of larger resection with bone removal or intranasal involvement
- Consider infiltration with above local mixture for hemostasis and postoperative comfort
Technique
- Skin marking uses an Iliff type incision starting at the superior border of the medial canthal tendon and curving downward along the anterior lacrimal crest.
- Better aesthetic results are obtained by aligning this incision with the patient’s natural relaxed skin tension lines (Figure 2).
- Incision can be made with a 15 blade.
- CO2 laser, monopolar needle tip, radiofrequency wire, or other devices are preferred by some surgeons.
- Dissect down to the anterior lacrimal crest.
- Incise the periosteum using a monopolar cautery with needle tip (Figure 3).
- Use a Freer periosteal elevator to elevate the lacrimal sac from the lacrimal fossa
- Insert a Bowman probe and visualize in the sac.
- Free the lacrimal sac superiorly.
- Take care not to enter the nasal cavity, particularly if there is concern for a lesion. The posterior portion of the dissection encounters the ethmoid bone, which is very thin, so use caution.
- Isolate the anterior crus of the medial canthal tendon and cut using Westcott scissors to improve visualization and removal of the lacrimal sac.
- Baddeley et al. reported using viscoelastic to aid in visualization and dissection of the lacrimal sac.
- The upper punctum is clamped with a bulldog clip and viscoelastic is injected through the lower.
- The lower punctum is then clamped with a bulldog clip.
- The authors do not recommend this technique if there is a known or suspected lacrimal sac tumor.
- If a tumor is present and contained within the lacrimal sac, it is recommended to leave the sac intact to the best extent possible. If a tumor has eroded through the lacrimal sac, biopsy with frozen section analysis may be indicated.
- The lacrimal sac is then amputated from the nasolacrimal duct as inferiorly as possible.
- The lacrimal sac is sent to pathology for permanent histopathological analysis.
- In some cases, fresh tissue analysis for flow cytometry in cases of suspected lymphoproliferative disorders may be indicated.
- Frozen section analysis may be used as well.
- In setting of dacryocystitis, copious irrigation of the fossa with saline or antibiotic solution is indicated.
- Confirm the sac has been removed by placing a Bowman probe in the lower punctum and visualizing it exiting the common canaliculus (Figure 4).
- The superior opening of the nasolacrimal duct, now exposed, should be sealed to prevent reflux of nasal contents into the lacrimal sac fossa.
- This can be accomplished with the monopolar cautery.
- The same technique can be used to seal the common canalicular opening/common internal punctum.
- Repair the medial canthal tendon using a 5-0 polyglactin or polypropylene suture in a horizontal mattress fashion.
- Medial orbital fat can be mobilized and secured to the periosteum using 6-0 polyglactin suture to fill the lacrimal sac fossa and reduce or eliminate dead space (Figure 5).
- Orbicularis is closed using buried 6-0 polyglactin suture.
- Skin is closed using 6-0 plain gut or polypropylene suture in a running or interrupted fashion.
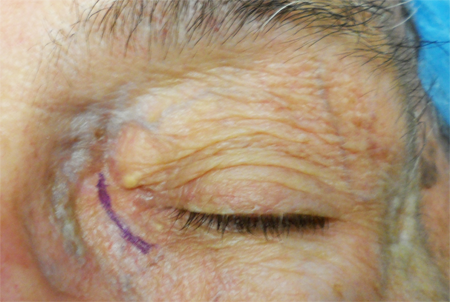
Figure 2. Patient marked using a modified Iliff incision.

Figure 3. Incision along anterior lacrimal crest.

Figure 4. Following removal of the lacrimal sac, the Bowman probe is seen exiting the common canaliculus/common internal punctum.

Figure 5. Transfer of medial orbital fat into dead space.
Endoscopic technique
Shams and Selva published a case in 2013 using an endoscopic approach for chronic dacryocystitis following a failed external DCR in which a demented patient aggressively agitated the incision leading to dehiscence and wound infection. The endoscopic approach was performed to avoid an external incision and was successful. The common canaliculus was treated with local cauterization.
Patient management: treatment and follow-up
Postoperative instructions
Postanesthesia precautions
- No heavy lifting or bending
- Do not rub the incision
- Sleep with head of bead elevated
- Ice packs to surgical site for 15 minutes every hour while awake for 3 days
- Resume anticoagulation on post-operative day one
Medications prescribed
- Analgesia
- Often require only acetaminophen
- Cautious use of narcotics for older patients
- Consider ophthalmic antibiotic ointment to the incision.
- Consider oral antibiotics in setting of chronic dacryocystitis.
Other management considerations
Depending on the outcome of the intraoperative frozen section biopsy, patient may require referral to oncology and/or otolaryngology for further surgical and medical management.
Common treatment responses, follow-up strategies
Chronic dacryocystitis
- Erythema and pain should improve considerably over 1–2 weeks postoperatively.
- Purulent discharge should improve immediately, although patients will likely have irritation and discharge for 1–2 weeks.
Suspected or unsuspected lacrimal tumor
- Patient will have pain and erythema associated with surgery that should resolve over 1–2 weeks.
- Patients that had partial or no obstruction of the nasolacrimal system, as is common with lacrimal sac tumors, will likely have increased epiphora postoperatively.
- As mentioned above, management will vary based on the results of the biopsy and there will likely be further management and referral.
Preventing and managing treatment complications
Epiphora
Dacrycystectomy is avoided if possible, particularly in patients that have preoperative complaints of epiphora or are likely to develop epiphora postoperatively as detailed above.
Infection
Wound infection
- Treat with oral and topical antibiotics.
- Evaluate and follow for orbital involvement.
- If there are orbital signs or concern for abscess collection, consider CT of the orbits and possible admission for intravenous antibiotics, +/- abscess drainage.
Recurrent dacryocystitis
- If the lacrimal sac is incompletely removed, patients can develop recurrent dacryocystocele and dacryocystitis.
- If the lacrimal sac is completely removed, there is still a potential for infection in the lacrimal sac fossa.
Lacrimal cutaneous fistula
Treat with excision of fistulous tract and any residual lacrimal sac.
Vision Loss
Retrobulbar hematoma
- Rare, only a single reported case
- Although the authors have experienced a retrobulbar hematoma following injection of local anesthetic in preparation for a DCR.
Orbital cellulitis
Disease-related complications
Chronic dacryocystitis
- Recurrent disease as detailed above
Lacrimal sac tumors
A relatively rare group of benign and malignant tumors:
Benign
- Recurrence
- Bleeding
- Nasolacrimal obstructive
Malignant
- Local and distant spread
- Destruction of lacrimal system and surrounding tissues
- Invasion of Orbit and sinuses
- Death
Historical perspective
First described by Woolhouse in 1724 as a treatment for NLDO, however after the description of the DCR by Toti and subsequent modifications, the dacryocystectomy is primarily reserved for the mentioned indications
References and additional resources
- http://www.asoprs.org/i4a/pages/index.cfm?pageid=3676
- Black EH, et al. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. 3rd ed. New York: Springer; 2012; 611-613.
- Scruggs R. T., Hurwitz J. J. (In Press). Lacrimal Sac Tumors. Z. A. Karcioglu (Ed.). Orbital Tumors: Diagnosis and Treatment. New York, NY: Springer.
- Holds JB, Anderson RL, Wolin MJ. Dacryocystectomy for the treatment of dacryocystitis patients with Wegener’s granulomatosis. Ophthalmic Surg 1989; 20(6):443–444.
- Boynton JR, Anawis MA. Role of dacryocystectomy in the management of failed dacryocystorhinostomy associated with chronic dacryocystitis. Ophthalmic Surg Lasers 1996;27(2): 133–136.
- Mauriello JA, Vadehra VK. Dacryocystectomy: surgical indications and results in 25 patients. Ophthalmic Plastic Reconstruct Surg 1997; 13(3): 216–220.
- Matayoshi S1, Van Baak A, Cozac A, Sardinha M, Fernandes JB, da Mota Moura E. Dacryocystectomy: indications and results. Orbit. 2004 Sep;23(3):169-73.
- Cook HL, Olver JM. Dacryocystectomy as treatment of chronic dacryocystitis in a frail, elderly patient. Eye. 2004;18:334-336.
- Baddeley PA, Lewis GD, Lane CM. A novel technique to facilitate dacryocystectomy using viscoelastic substances. Orbit. 2011 Jun;30(3):158-9.
- Shams PN, Selva D. Orbit. An endoscopic endonasal approach to dacryocystectomy. 2013 Apr;32(2):134-6.
- Pai VH, Rao DK, Bhandary SV. Visual loss following dacryocystectomy. Ophthalmic Surg Lasers Imaging. 2006 Nov-Dec;37(6):494-6.
- Duke-Elder S, MacFaul PA. The ocular adnexa. In: Duke-Elder S (ed). System of Ophthalmology, Vol 13. Part II. Lacrimal,Orbital and Para-orbital Diseases. Henry Kimpton: London,1974, pp 715–718.
