Eosinophilic orbital disease
Updated July 2024
Establishing the diagnosis
Etiology
The differential diagnosis for eosinophilic disorders with orbital involvement includes:
- Eosinophilic granulomatosis with polyangiitis (EGPA)
- Kimura’s Disease (KD)
- Angiolymphoid hyperplasia with eosinophilia (ALHE)
- Eosinophilic angiocentric fibrosis (EAF)
- Hypereosinophilic syndrome (HES)
- Eosinophilic asthma
- Parasitic infection
Epidemiology
EGPA
- Prevalence 2-22 per million
- Annual incidence 0.3-3.7 per million
- Occurs primarily during adulthood in bimodal distribution, with peak at 30-40 years-old, and is rare in children (Akella, Ophthalmic Plast Reconstr Surg 2019)
- No gender predominance or ethnic predisposition
Kimura’s disease
- Occurs most frequently in young East Asian men in the 2nd to 4th decades of life
- Orbital involvement may occur in older patients (Buggage, Surv Ophthalmol 1999)
ALHE
- Commonly seen in middle-aged Caucasian individuals, often in the 3rd and 4th decades
- Female predominance
EAF
- Unknown prevalence and epidemiology
HES
- Unknown prevalence
- Most often affects people ages 20-50
Eosinophilic asthma
- Unknown prevalence
- Approximately 10% of all asthma is categorized as severe adult-onset eosinophilic asthma
- Most commonly diagnosed in adults 35-50 years old, although it can be seen in older adults and children (Walford, J Asthma Allergy 2014)
Parasitic infection
- More prevalent in geographic areas where environmental factors and poor sanitary conditions favor transmission from animal hosts
- Toxocariasis is the most prevalent human helminthic infection in industrialized countries (Padhi, Surv Ophthalmol 2017)
Clinical features
EGPA
- Systemic vasculitis of small-to-medium sized blood vessels
- Typically presents in three phases: (Akella, Ophthalmic Plast Reconstr Surg 2019)
- Prodromal asthmatic and allergic phase: second and third decades of life, asthmatic and allergic symptoms, such as nasal congestion, shortness of breath, and cough
- Eosinophilic phase: peripheral eosinophilia and eosinophilic infiltration of multiple organs, typically lungs and gastrointestinal tract, manifesting with asthma and/or gastroenteritis
- Vasculitic phase: life-threatening vasculitis, occurs 8-10 years after asthmatic phase
- Ocular involvement can be divided into 2 groups (Takanashi, Ophthalmology 2001)
- Orbital inflammatory-type
- Conjunctival nodules, myositis, diffuse orbital inflammation, dacryoadenitis, cranial nerve palsy
- Ischemic vasculitis-type
- Retinal artery and vein occlusions, ischemic optic neuropathy, retinal vasculitis
Kimura’s Disease
- Nontender subcutaneous inflammatory nodules of the head and neck (Kanazawa, Graefe’s Arch Clin Exp Ophthalmol 1999)
- Orbital signs include palpable mass, proptosis, motility restriction, and eyelid edema
- Often have regional lymphadenopathy, salivary gland involvement, nephropathy, systemic eosinophilia (Buggage, Surv Ophthalmol 1999)
- Disease duration up to 25 years
- Believed to be autoimmune-related
ALHE
- Similar to Kimura’s Disease with nontender subcutaneous nodules in the head and neck
- Orbital signs include proptosis and eyelid edema
- Disease duration generally shorter than Kimura’s Disease (1-4 years) (Azari, JAMA Ophthalmol 2014)
- Believed to be a reactive or neoplastic proliferation of vascular endothelium
EAF
- Unclear whether it is a neoplasm or a fibroinflammatory lesion mimicking a neoplasm
- Some believe it to be on the spectrum of IgG4-related disease and/or related to granuloma faciale (Roberts, Histopathology 1985)
- Typically affects the sinonasal and respiratory tracts and rarely involves the orbit (Deshpande, Am J Surg Pathol 2011)
HES
- A myeloproliferative disorder characterized by eosinophilia
- Diagnosis of exclusion after ruling out other causes of eosinophilia
- May be asymptomatic or with severe symptoms consistent with end-organ damage due to eosinophilic infiltration of skin, heart, lungs, and central nervous system (Curtis, Clin Rev Allergy Immunol 2016)
- Can present as orbital inflammation with proptosis and dacryoadenitis (Das Indian J Ophthalmol 2018, Zenone Presse Med 2005) or retinal vascular changes due to hypercoagulability
Eosinophilic asthma
- A subtype of asthma, which is severe, adult-onset, and resistant to corticosteroids
- Asthmatic and allergic symptoms such as nasal congestion, shortness of breath, cough
- May involve dacryoadenitis
Parasitic infection
- Various presentations including cyst or solid nodule in the orbit, extraocular muscles, eyelid, or conjunctiva, as well as uveitis, retinitis, and optic neuritis (Padhi, Surv Ophthalmol 2017)
- Inflammatory signs if cyst ruptures
- Systemic manifestations including gastrointestinal, hepatobiliary, pulmonary, cardiovascular, and central nervous system (Padhi, Surv Ophthalmol 2017)
Testing
Laboratory testing
- EGPA
- Peripheral eosinophilia
- Positive ANCA in 30-40% of cases, most commonly myeloperoxidase-ANCA (P-ANCA) and proteinase 3 (Radice Autoimmun Rev 2013)
- Kimura’s Disease
- Peripheral eosinophilia
- Elevated serum IgE
- May have elevated serum IgG4 levels (Kamisawa Lancet 2015)
- ALHE
- Peripheral eosinophilia much less common than Kimura’s Disease
- EAF
- Peripheral eosinophilia (Deshpande, Am J Surg Pathol 2011)
- HES
- Peripheral eosinophilia
- Need to rule out other etiologies
- Parasitic infection (Padhi, Surv Ophthalmol 2017)
- Peripheral eosinophilia
- Elevated serum IgE
- Stool sample for ova/parasites
- Serological tests such as complement fixation, ELISA, and indirect hemagglutination
- Cerebrospinal fluid tests
- Eosinophilic asthma (Walford, J Asthma Allergy 2014)
- Sputum eosinophils >1-3%
- Peripheral eosinophilia
- Elevated serum IgE
- Fractional exhaled nitric oxide level
- Serum periostin levels
Imaging
- EGPA
- CT or MRI demonstrates an orbital mass or infiltration (57%), enhancement or enlargement of rectus muscles (29%), lacrimal gland enlargement (36%), and/or optic nerve sheath enhancement (14%) (Akella, Ophthalmic Plast Reconstr Surg 2019)
- Kimura’s Disease
- CT or MRI demonstrates an orbital mass, enlargement extraocular muscles
- Parasitic infection
- Ultrasonography is helpful in detecting scolex in cysticercosis (Padhi, Surv Ophthalmol 2017)
- CT or MRI demonstrates a cystic orbital lesion
Histopathology
- EGPA
- Necrotizing vasculitis
- Extravascular eosinophil rich granulomatous inflammation
- Kimura’s Disease
- 3 components (Buggage, Surv Ophthalmol 1999)
- Cellular (eosinophilic infiltrate and follicular hyperplasia)
- Fibrocollagenous
- Vascular
- Lymphoid hyperplasia within germinal centers
- Eosinophilic microabscesses (McKelvie, Pathology 2012)
- 3 components (Buggage, Surv Ophthalmol 1999)
- ALHE
- Proliferation of arterioles, venules, and capillaries (compared to mainly capillaries in Kimura’s Disease) (Azari, JAMA Ophthalmol 2014)
- Endothelial cell atypia
- Paucity of follicles and fibrosis
- Endothelial cells with epithelioid or histiocytoid changes (Buggage, Surv Ophthalmol 1999)
- Eosinophilia
- EAF
- Concentric layers of fibrosis surrounding small-caliber arterioles (Benlemlih, Ann Pathol 2012)
- Eosinophilic infiltrate
- HES
- Eosinophilic tissue infiltration
- Eosinophilic asthma
- Eosinophilic cellular infiltrate
- Parasitic infection
- Parasite at the center of a lesion with eosinophilic or necrotizing granuloma
Diagnostic criteria
EGPA: Per the American College of Rheumatology, diagnosis requires the presence at least 4 of 6 conditions (Masi, Arthritis Rheum 1990)
- Asthma
- Eosinophilia of greater than 10%
- Neuropathy
- Migratory or transient pulmonary opacities
- Abnormalities of the paranasal sinuses
- Extravascular eosinophils on biopsy
HES: As defined by Chusid et al. there are 3 criteria (Chusid, Medicine (Baltimore) 1975)
- Eosinophil count >1500 cells/microliter persisting longer than 6 months
- Single or multiple organ system dysfunction attributable to cytotoxic injury by eosinophils
- No identifiable etiology to explain the eosinophilia
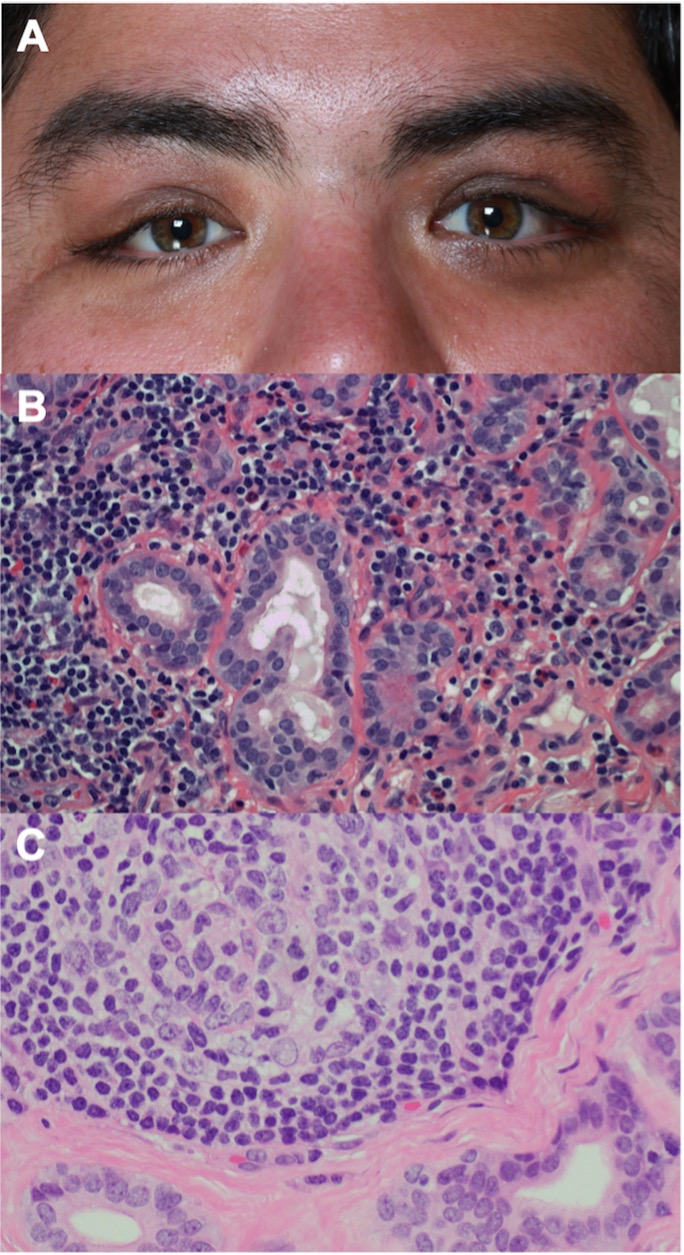
Figure 1. Case 1. (A) Clinical photograph demonstrating mild, bilateral lacrimal gland enlargement. (B) Biopsy of the left lacrimal gland reveals infiltration of eosinophils, lymphocytes, and plasma cells without granuloma, necrosis, or vasculitis (Hematoxylin and eosin x400). (C) Biopsy of the right lacrimal gland demonstrates dense lymphoid infiltrate with follicular hyperplasia and fibrosis without eosinophils (Hematoxylin and eosin x400).
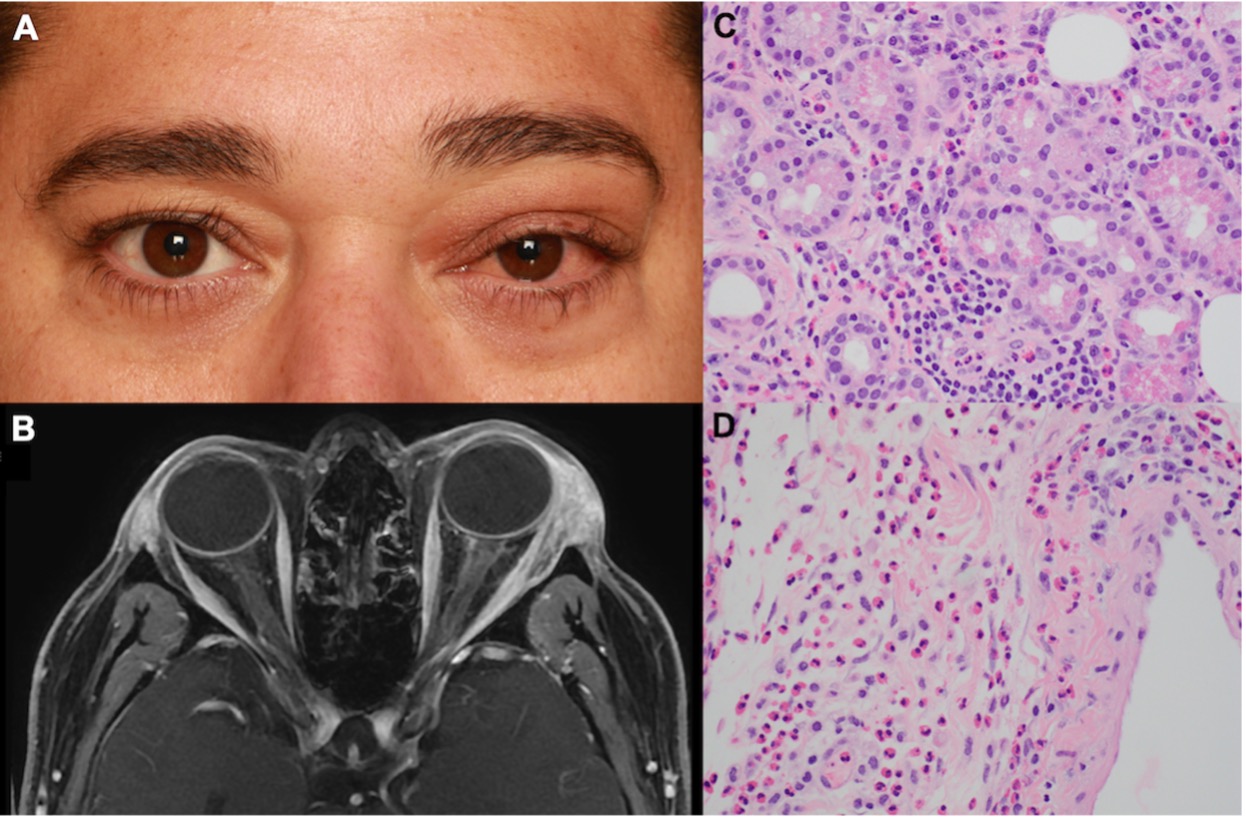
Figure 2. Case 2. (A) Clinical photograph showing left upper eyelid edema, ptosis, chemosis, and injection. (B) Axial T1 post-contrast with fat suppression MR image demonstrating enlargement of the left lacrimal gland. Biopsy of the left lacrimal gland reveals the presence of marked eosinophils in the glandular tissue (C) and stroma (D) without granuloma or vasculitis (Hematoxylin and eosin x400).
Differential diagnosis
- Granulomatosis with polyangiitis (Wegener’s granulomatosis)
- Microscopic polyangiitis
- Lymphoma
- Sarcoidosis
- Tuberculosis
- Idiopathic orbital inflammation
Patient management: treatment and follow-up
Treatment options
EGPA
- Systemic corticosteroids (high-dose prednisone 1 mg/kg/day until remission attained with gradual taper) – if acute multiorgan disease, higher dose 1 g IV methylprednisolone 1g/day for 3 days followed by above therapy) (Akella, Ophthalmic Plast Reconstr Surg 2019)
- Immunosuppressants (cyclophosphamide is first line, others include azathioprine, methotrexate, leflunomide)
Kimura’s Disease
- Primarily surgical excision (Kanazawa, Graefe’s Arch Clin Exp Ophthalmol 1999)
- Other treatments: radiation, oral and/or intralesional steroids (though with recurrence after cessation of treatment), chemotherapeutic agents (Buggage, Surv Ophthalmol 1999)
ALHE
- Primarily surgical excision or debulking (Cunniffe, Int Ophthalmol 2014)
- Other treatments: radiation, oral and/or intralesional steroids, chemotherapeutic agents, and laser (Buggage, Surv Ophthalmol 1999)
- Observation after biopsy is reasonable, as most lesions regress spontaneously
EAF
- Surgical excision of lesions
- Immunosuppressive therapy (systemic corticosteroids, steroid-sparing agents) may be less effective with recurrence of the lesion (Deshpande, Am J Surg Pathol 2011)
HES
- Systemic corticosteroids (high-dose prednisone 1 mg/kg/day)
- Other treatments: hydroxyurea, cyclosporin, interferon-alpha
- Biologics: imatinib mesylate, mepolizumab (anti-IL5 antibody), stem cell transplantation (Curtis, Clin Rev Allergy Immunol 2016)
Parasitic infection (Padhi, Surv Ophthalmol 2017)
- Treatment depends on the parasite
- Surgical excision of the nodule, removal of worm
- Anti-helminthic therapy (albendazole, mebendazole, praziquantel, ivermectin, etc.) – agent depends on the pathogen
- Systemic or periocular corticosteroids
- Laser ablation of worm
Eosinophilic asthma
- Systemic corticosteroids (high-dose prednisone 1 mg/kg/day)
- T-helper type 2 (Th2) targeted treatments, such as mepolizumab (IL-5 inhibitor) (Drick BMC Pulm Med 2018, Corren, Discov Med 2012)
- IL-4 and IL-13 inhibitors are undergoing studies (Walford, J Asthma Allergy 2014)
- Omalizumab (anti-IgE monoclonal antibody) (Walford, J Asthma Allergy 2014)
Preventing and managing treatment complications
- Systemic corticosteroid complications – avoid long-term use of high-dose systemic corticosteroids
- Surgical complications
- Immunosuppressant complications
- Anti-helminthic therapy can cause cyst rupture – rule out cysts in brain before starting cysticidal medications and monitor neurologic status
Disease-related complications
EGPA
- Cardiovascular compromise, renal failure, and neurologic decline
- Untreated patients have a 50% risk of death within 3 months of vasculitis onset, whereas treated EGPA patient has a 70-90% survival at 5 years (Takanashi, Ophthalmology 2001)
- Heart disease most common cause of death (50%) (Akella, Ophthalmic Plast Reconstr Surg 2019)
Kimura’s Disease
- Lesions gradually enlarge and increase over time or spontaneously regress (Buggage, Surv Ophthalmol 1999)
- Recurrence can occur with incomplete excision
AHLE
- Recurrence can occur with incomplete excision (Azari, JAMA Ophthalmol 2014)
EAF
- Lesions are benign but progressive and tend to recur with many patients undergoing multiple surgeries for alleviation of symptoms
HES
- Eosinophilic infiltration can cause end-organ damage of the heart, lungs, and central nervous system (Curtis, Clin Rev Allergy Immunol 2016)
Parasitic infection
- End-organ damage from worm (neurologic, cardiac, ocular)
Historical perspective
EGPA
- First described in 1951 by Churg and Strauss (Churg and Strauss, Am J Pathol 1951)
- Previously known as Churg-Strauss syndrome or allergic granulomatosis and angiitis
- In 1956 Cury et al. became the first to describe ophthalmic involvement (Cury, AMA Arch Ophthalmol 1956)
Kimura’s Disease
- First reported in 1937 by Kimm and Szeto as eosinophilic hyperplastic lymphogranuloma
- Kimura et al. in 1948 described similar cases (Kimura, Trans Soc Pathol Jpn 1948)
ALHE
- Described by Wells and Whimster in England in 1969, hey suggested similarity to Kimura’s Disease (Wells, Br J Dermatol 1969)
- Rosai et al. were the first to suggest Kimura’s Disease and ALHE were different entities due to the lack of cellular atypia in Kimura’s Disease (Rosai, Am J Dermatopathol 1982) (Rosai, Hum Pathol 1979)
EAF
- First described by Roberts and McCann in 1985 (Roberts, Histopathology 1985)
HES
- First described by Hardy and Anderson in 1968 (Hardy, Ann Intern Med 1968)
References and additional resources
- Akella SS, Schlachter DM, Black EH, Barmettler A. Ophthalmic eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome): A systematic review of the literature. Ophthalmic Plast Reconstr Surg 2019;35(1):7-16.
- Walford HH, Doherty TA. Diagnosis and management of eosinophilic asthma: a US perspective. J Asthma Allergy 2014;7:53-65.
- Radice A, Bianchi L, Sinico RA. Anti-neutrophil cytoplasmic autoantibodies: Methodological aspects and clinical significance in systemic vasculitis. Autoimmun Rev 2013;12(4):487-95.
- Corren J. Inhibition of interleukin-5 for the treatment of eosinophilic diseases. Discov Med 2012;13(71):305-12.
- Drick N, Seeliger B, Welte T, et al. Anti-IL-5 therapy in patients with severe eosinophilic asthma – clinical efficacy and possible criteria for treatment response. BMC Pulm Med 2018;18(1):119.
- Buggage RR, Spraul CW, Wojno TH, Grossniklaus HE. Kimura disease of the orbit and ocular adnexa. Surv Ophthalmol 1999;44(1):79-91.
- Kanazawa S, Gong H, Kitaoka T, Amemiya T. Eosinophilic granuloma (Kimura’s disease) of the orbit: a case report. Graefe’s Arch Clin Exp Ophthalmol 1999;237(6):518-21.
- Kamisawa T, Zen Y, Pillai S, Stone JH. IgG4-related disease. Lancet 2015;385(9976):1460-71.
- Li J, Ge X, Ma J, et al. Kimura’s disease of the lacrimal gland mimicking IgG4-related orbital disease. BMC Ophthalmol 2014;14:158.
- McKelvie PA, Lyons B, Barnett G, Allen PW. Kimura’s disease in two Caucasians, one with multiple recurrences associated with prominent IgG4 production. Pathology 2012;44(3):275-8.
- Lee JH, Kim JH, Lee SU, Kim SC. Orbital mass with features of both Kimura Disease and immunoglobulin G4-related disease. Ophthal Plast Reconstr Surg 2018;34(4):e121-3.
- Benlemlih A, Szableski V, Bendahou M, et al. Fibrose angiocentrique à éosinophiles: une manifestation de la maladie systémique liée au IgG4? [Eosinophilic angiocentric fibrosis: a form of IgG4-related systemic disease?]. Ann Pathol 2012;32(4):271‐5.
- Deshpande V, Khosroshahi A, Nielsen GP, Hamilos DL, Stone JH. Eosinophilic angiocentric fibrosis is a form of IgG4-related systemic disease. Am J Surg Pathol 2011;35(5):701‐6.
- Huang L, Appleton JA. Eosinophils in helminth infection: Defenders and dupes. Trends Parasitol 2016;32(10):798-807.
- Padhi TR, Das S, Sharma S, et al. Ocular parasitoses: A comprehensive review. Surv Ophthalmol 2017;62(2):161-89.
- Curtis C, Ogbogu P. Hypereosinophilic Syndrome. Clin Rev Allergy Immunol. 2016;50(2):240-251.
- Das JK, Gupta K, Deshmukh S, Shrivastava R. A rare case of hypereosinophilic syndrome presenting with unilateral proptosis and torticollis. Indian J Ophthalmol. 2018;66(10):1508-1511.
- Zenone T, Ligeon-Ligeonnet P. Hypereosinophilic syndrome and orbital inflammatory pseudotumor. Presse Med 2005;34(16 Pt 1):1141-1142.
- Takanashi T, Uchida S, Arita M, et al. Orbital inflammatory pseudotumor and ischemic vasculitis in Churg-Strauss syndrome: report of two cases and review of the literature. Ophthalmology 2001;108:1129–33.
- Cury D, Breakey AS, Payne BF. Allergic granulomatous angiitis associated with uveoscleritis and papilledema. AMA Arch Ophthalmol 1956;55:261–6.
- Masi AT, Hunder GG, Lie JT, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum 1990;33:1094–100.
- Cunniffe G, Alonso T, Dinarès C, Medina FJ, Medel R. Angiolymphoid hyperplasia with eosinophilia of the eyelid and orbit: the Western cousin of Kimura’s disease. Int Ophthalmol 2014;34(1):107-10.
- Azari AA, Kanavi MR, Lucarelli M, et al. Angiolymphoid hyperplasia with eosinophilia of the orbit and ocular adnexa: report of 5 cases. JAMA Ophthalmol 2014;132(5):633-6.
- Kimura T, Yoshimura S, Ishikawa E: On the unusual granulation combined with hyperplastic changes of lymphatic tissues. Trans Soc Pathol Jpn 1948;37:179–80.
- Wells GC, Whimster IW: Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969;81:1–14.
- Rosai J: Angiolymphoid hyperplasia with eosinophilia of the skin: Its nosological position in the spectrum of histiocytoid hemangioma. Am J Dermatopathol 1982;4:175–84.
- Rosai J, Gold J, Landy R: The histiocytoid hemangiomas: A unifying concept embracing several previously described entities of skin, soft tissue, large vessels, bone, and heart. Hum Pathol 1970;10:707–30.
- Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: Analysis of fourteen cases with review of the literature. Medicine (Baltimore) 1975;54:1‑27.
- Roberts PF, McCann BG. Eosinophilic angiocentric fibrosis of the upper respiratory tract: a mucosal variant of granuloma faciale? A report of three cases. Histopathology. 1985;9:1217–1225.
- Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol 1951;27(2):277-301.
- Hardy WR, Anderson RE. The hypereosinophilic syndromes. Ann Intern Med 1968;68(6):1220-9.
- Cohen LM, Danesh K, Liu Y, Karlin JN, Rootman DB. Atypical systemic eosinophilic disease presenting as dacryoadenitis. Poster presentation at ASOPRS 51st Annual Fall Scientific Symposium; 2020 Nov. 20-22; Virtual Meeting.
