External (Transcutaneous) Levator Advancement (Resection) for Ptosis
Updated August 2024
Goals, indications, contraindications
- Primary goal: Improvement of superior and peripheral visual field, and to prevent amblyopia in young children with ptosis obstructing pupil
- Secondary goal: Improved functioning in daily activities, aesthetic improvement and symmetry of lids
- Indications
- Ptosis with good or moderate levator function
- Advancement (or repair) in cases of levator dehiscence
- Contraindications
- Absolute
- Ptosis with poor levator function (generally 4 mm or less)
- Relative
- Severe dry eyes
- Superior trabeculectomy
- Corneal hypesthesia
- Significant lagophthalmos
- Bell’s palsy
Preprocedure evaluation
Patient history
- Congenital vs. acquired
- Trauma
- Rapid or insidious onset
- Associated diplopia
- Generalized weakness
- Difficulty swallowing
- Visual obstruction/effect on daily activities
- Variable or fluctuating symptoms
Clinical examination
- Levator function
- Amount of ptosis (margin reflex distance, MRD1)
- Motility evaluation (ophthalmoplegia, congenital fibrosis of EOM)
- Pupillary evaluation (miosis, anisocoria)
- Bell’s reflex
- Corneal sensation
- Tear film, tear meniscus height, tear breakup time
- Basal secretion — Schirmer test
- Lid crease height
- Orbicularis function
- Lagophthalmos
- Epicanthal fold
- Dermatochalasis and hooding: External approach is easily performed after the blepharoplasty flap is removed.
Preoperative assessment
- Better levator function is associated with better results.
- Poorer levator function is associated postoperatively with lagophthalmos, lid height drop, less natural movement of the lid.
- Consider conservative elevation if levator function is poor; discuss with patient that elevation might be less optimal.
- Intraoperative dynamic adjustment helps avoid postoperative lagophthalmos.
- Highly asymmetric levator function should be evaluated for possible orbital mass affecting superior orbit/levator muscle.
Procedure alternatives
Nonsurgical alternatives are of limited usefulness.
- Ptosis eyelid crutches
- Taping of the eyelids
- Phenylephedrine drops
Surgical alternatives depend on the amount and type of ptosis and the degree of levator function.
- Conjunctivomullerectomy (internal ptosis approach)
- Frontalis sling
Surgical techniques
These cases are preferably performed under local anesthesia with sedation. In children, levator resection can be done by formula (Beard or Berke) under general anesthesia (Table 1 and Table 2).
- Preoperative factors influencing choice of technique and amount of advancement
- Amount of ptosis
- Levator function (poor, fair, good, excellent)
- Contour deformities
- Presence or absence of normal globe supraduction
- Presence and amount of jaw-winking
- Intraoperative factors influencing decision-making
- State of levator elasticity
- Intraoperative position of lid margin achieved by advancement
Table 1. Estimation of levator resection (Beard, 1976).
|
Amount of Ptosis |
Upper lid excursion |
Amount of Resection |
|
2 mm (mild) |
0-5 mm (poor) |
22-27 mm |
|
6-11 mm (fair) |
16-21 mm |
|
|
12 or more (good) |
10-15 mm |
|
|
3 mm (moderate) |
0-5 mm (poor) |
Maximum (30 mm) |
|
6-11 mm (fair) |
22-27 mm |
|
|
12 or more (good) |
16-21 mm |
|
|
4 mm or more (severe) |
0-5 mm (poor) |
Maximum (30 mm) |
|
6-11 mm (fair) |
25-30 mm |
|
|
12 or more (good) |
25-30 mm |
Table 2. Intraoperative eyelid height (Berke 1959, Berke 1961).
|
Upper lid levator function |
Superior corneal coverage by upper lid |
|
0–5 mm (poor) |
0 mm (lid margin at superior limbus) |
|
6-11 mm (fair) |
2 mm |
|
12 or more (good) |
4 mm |
Dissection
- Lid crease incision (or following blepharoplasty flap excision)
- Small-incision technique can be performed through a small 8-mm incision at the central lid (Figure 1).
- Useful for reoperations or in cases of minimal skin redundancy
- Expose the central superior tarsal plate.
- Open orbital septum, taking care to avoid injury to the levator muscle.
- Elevate fat off the anterior aspect of the levator aponeurosis (Figure 2).
Levator surgery
If dehiscence of the levator aponeurosis is present, advancement of the upper edge of aponeurosis is appropriate as first step.
The superior aponeurosis should be sutured to the tarsus, and lid height checked.
- Suture to superior third of tarsus with partial thickness bite.
- Evert the lid to confirm no suture exposure on posterior lid.
- Patient can be moved to a seated position and asked to open and close lids.
- Adjust margin contour by placement of second suture if needed.
- If significant lagophthalmos is noted intraoperatively, consider lowering lid slightly.
If inadequate height has been achieved, the levator aponeurosis can be further advanced by placing the suture higher up on the aponeurosis, sutured lower on the tarsus, and the excess excised.
- Suturing too inferior on the tarsus can result in lid margin eversion or peaking of contour.
If no dehiscence is present (i.e., congenital), the levator is resected and advanced appropriately based on preoperative measurements and algorithms (Beard 1976; Berke 1959 and 1961), often leaving a 1–2 mm overcorrection.
- Levator resections typically vary between 8 and 30 mm.
- A Berke ptosis clamp is useful to isolate and measure the tissue (Figure 3).
- To achieve larger resections, carefully dissect levator muscle off the underlying Muller muscle.
- Resection often approaches or includes Whitnall’s ligament, as opposed to levator advancement surgery in adults.
- Approximately 3 nonabsorbable sutures are placed at the edge of the resected levator complex to secure it to the tarsus.
- Intraoperative adjustment is not needed, making this approach ideal for children or patients with limited cooperation.
- Final lid height is set intraoperatively based on levator function, with the principle that a lid with poor excursion should be set higher because it might fall postoperatively, whereas a lid with better function tends to rise after surgery.
Closure
Reformation of the eyelid crease is sometimes performed with skin closure.
The orbicularis muscle is sometimes closed as a separate layer than the skin.
If a more defined lid crease is desired, suture the pretarsal orbicularis edge to the superior tarsus or underlying levator aponeurosis at the desired crease height.
Closure should blend smoothly into any existing epicanthal fold.
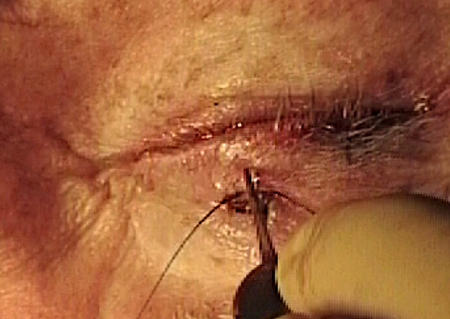
Figure 1. Small-incision ptosis technique performed through a small 8-mm lid crease incision.

Figure 2. Levator muscle and aponeurosis complex of the upper lid.
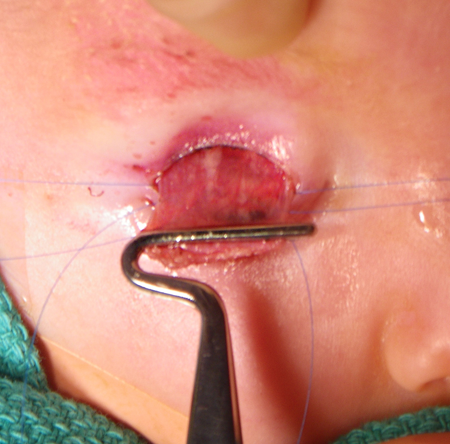
Figure 3. Levator muscle clamped with a Berke ptosis clamp in levator resection procedure.
Patient management: treatment and follow-up
Postoperative instructions
- Apply cold compresses for 48 hours postoperatively to minimize edema and ecchymosis.
- Lubricate the cornea with artificial tears liberally until normal blink returns.
- Elevate head of bed for 1 week.
- No strenuous activity, lifting, or bending for 1 week
- Avoid rubbing the face and lids for 1–2 weeks to avoid dehiscence.
- May apply makeup carefully in 1 week
- Follow-up visit in several days to 1 week after surgery
- Evaluate lid position, lid closure, corneal surface, wound healing, infection.
Medications prescribed
Antibiotic ointment can be applied to sutures 2–4 times a day for 1–2 weeks. This might temporarily blur vision.
Other management considerations
Patient should call the office for any sudden bleeding that does not stop, or for worsened pain, tenderness, purulent discharge, fever, or decrease in vision.
Nonessential vitamins and herbals that might risk bleeding should be discontinued for 1–2 weeks after the procedure.
Aspirin and NSAIDS can be resumed judiciously within several days to a week postoperatively depending on medical need.
Consider use of oral Arnica Montana pills or topical cream perioperatively to decrease swelling and bruising, although this is considered anecdotal.
Common treatment responses, follow-up strategies
Ecchymosis is common for 1–2 weeks after surgery.
Edema can take several months for complete resolution, although first few weeks are most noticeable.
Mild asymmetry within first few weeks might be secondary to edema and can be observed for spontaneous improvement.
Large asymmetry can be revised in the office within 1–2 weeks as tissue fibrosis is minimal.
Use local anesthesia with epinephrine for hemostasis
Incision and planes can be gently spread apart without cutting.
If more elevation is needed, tighten sutures or replace lower on tarsus.
Preventing and managing treatment complications
Overcorrection
If possible, ask patient to open and close during the procedure to assess lid height.
- Sedation should be discontinued in advance so that patient is completely alert and cooperative.
- Lid should be set at the desired position for cases with good levator function.
- Alternate cover testing might uncover Hering’s law fixation influences.
Mild overcorrection is managed with lubrication, massage, and observation.
Lid stretching exercises can be started 2 weeks after surgery by instructing patient to hold the lashes down toward the anterior cheek and then looking far up and down repeatedly.
- If performed properly, this stretches the tissue layers and can titrate down the MRD up to 2 mm
Greater overcorrection requires cutting or replacing the tarsal levator suture in good function cases.
When the eyelid has decreased function preoperatively (e.g., severe congenital ptosis), the lid can drop slightly postoperatively.
Undercorrection
Observation to determine whether eyelid edema or hematoma is mechanically pushing the lid down
Reoperation to elevate the lid more might be necessary for visual or appearance reasons.
- Advance suture higher up on aponeurosis or pass tarsal suture lower.
Dry-eye symptoms
- Aggressive lubrication with monitoring of ocular surface integrity
- Massage of lid to stretch tissues
- Punctal plugs
- Observation for return of normal eyelid blink postoperatively
Disease-related complications
Short-term
- Infection
- Hemorrhage, ecchymosis
- Loss of vision
- Asymmetry
- Overcorrection, undercorrection
- Dry eyes
- Suture granulomas
Long-term
- Lagophthalmos
- Dry eyes
- Recurrence, need for additional surgery
- Hypertrophic scar
Historical perspective
Levator resection
(Berke R, Beard C)
Surgery does not require patient involvement, thus amount of resection is predetermined based on degree of ptosis and levator muscle function. Large excisions often approach Whitnall’s ligament or higher. Final intraoperative height is set based on levator function, with the principle that a lid with poor excursion should be set higher as it may fall postoperatively. A supramaximal (greater than 30 mm) resection of levator muscle can result in a better cosmetic outcome than a unilateral sling in some cases, although conjunctival prolapse and significant lagophthalmos may occur.
Levator advancement
(Jones LT, Older JJ, Lui D)
Many variations of this technique exist with one to several sutures used to advance or plicate the dehisced levator complex to the superior tarsus. Some have advocated dissection in the plane between the levator muscle and the Muller’s muscle, and other variations describe intraoperative adjustment with the patient seated or lying down, and absorbable versus nonabsorbable sutures.
Small-incision ptosis technique
(Lemke BN)
Surgery is performed via a small 8-mm central lid crease, thus minimizing scar, intraoperative time, dissection, edema, and recovery time. One to two sutures are placed to advance levator aponeurosis to upper tarsus, with intraoperative dynamic adjustment. Contour typically excellent as less of the lid crease attachments of the terminal levator aponeurosis fibers have been disrupted.
Marcus-Gunn jaw-winking bilateral correction
(Beard C, Dortzbach RJ)
In patients with moderate to severe jaw-winking ptosis, levator extirpation or disinsertion of both lids, followed by bilateral slings, was advocated to provide better lid symmetry in downgaze and to stimulate frontalis recruitment as both lids would be equally ptotic. However, this adds the complications and risks of surgery to a healthy lid. A variation that does not disturb the integrity of the contralateral lid is the “chicken beard” technique in which the healthy levator is not disinserted, but a sling is placed.
References and additional resources
- AAO, Surgery of the Eyelid, Orbit & Lacrimal system, Vol. 2, 1994, p.100-109.
- AAO, Focal Points: Congenital Ptosis, Module #2, 2001, p.5-7.
- AAO, Focal Points: Management of Acquired Ptosis, Module #8, 1999, p.5-6.
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2013-14.
- Anderson R, et al. Whitnall’s sling for poor function ptosis. Arch Ophthalmol 1990; 108: 1628-1632.
- Baldwin H and Manners R. Congenital blepharoptosis. Ophthal Plast Reconstr Surg 2002; 18(4): 301-307.
- Beard C. A new treatment for severe unilateral congenital ptosis and for ptosis with jaw-winking. Am J Ophthalmol 1965; 59:252-8.
- Beard, C. “Congenital Ptosis” in Ptosis St. Louis, MO. CV Mosby Company: 1976, 91-115.
- Berke, R. Results of resection of the levator muscle through a skin incision in congenital ptosis AMA Arch Ophthalmol. 1959; 61(2):177-201.
- Berke, R. The surgical correction of congenital ptosis. Trans Pa Acad Ophthalmol Otolaryngol 1961;14:57-61.
- Demirci H, et al. Marcus Gunn Jaw-Winking Synkinesis. Ophthalmology 2010;117(7):1447-52.
- Epstein G and Putterman A. Supermaximum levator resection for severe unilateral congenital ptosis. Ophthalmic Surg 1984; 15(12): 971-9
- Frueh BR, Musch DC, McDonald HM. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology 2004; 111(12):2158-63.
- Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol 1975; 93:629–34.
- Kersten R, Bernardini FP, et al. Unilateral frontalis sling for the surgical correction of unilateral poor-function ptosis. Ophthal Plast Reconstr Surg 2005; 21(6): 412-417.
- Lucarelli MJ, Lemke BN. Small incision external levator repair: technique and early results. Am J Ophthalmol 1999;127:637–644.
- Liu D. Ptosis repair by single suture aponeurotic tuck: Surgical technique and long term results. Ophthalmology 1993;100:251–9.
- Older JJ. Levator aponeurosis tuck: a treatment for ptosis. Ophthalmic Surg 1978; 9:102-10.
