Eyelid edema
Updated August 2025
Imran Jarullazada, MD; Costas Papageorgiou, MD; Robert Alan Goldberg, MD, FACS
Establishing the diagnosis
Etiology
- Eyelid edema is the result of a fluid shift into the soft tissue of the eyelid structures with subsequent swelling; this can occur from a variety of etiologic factors.
- Infectious
- Inflammatory
- Neoplasm related
- Medication related
- Trauma/ Postsurgical/post injection
- Metabolic
- Generalized senescence of the lymphatic networ as a consequence of aging
- Others
Epidemiology
- This is a sporadic event which could be idiopathic or related to the underlying disease
- Can occur at any age, and no sex predilection
- Depending on the causative factor a single eyelid, unilateral, bilateral or all four eyelids could be affected
History
- Acute or chronic
- Unilateral/bilateral, upper eyelids/lower eyelids, single eyelid
- Number of episodes (first time or recurrent), age at onset
- Determine how long it is present (is it present all day long, worse in the morning, etc)
- Presence of itching or pain
- Any recent trauma
- previous surgeries
- traumas
- insect bites
- Medicine used:
- Orally or parentally not around orbit ( list of drugs reported to produce edema, Table 1)
- Recent periorbital injections or within last few years1.
- Recent contact with skin care products
- Any other reason for contact dermatitis (detergent, etc)
- Systemic symptoms of swelling, collagen vascular disease
Table 1: Systemic medications with a history of inducing ocular adnexal edema
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pertinent clinical features
- External examination should be done in 3 steps: eyelids and orbit, periorbital region including face and rest of the body.
- Eyelids and Orbit
- Eyelids
- Swelling
- Color change
- erythematous
- violaceous
- yellowish or xanthomatous Fig. 1
- Skin texture
- Cigarette paper like skin associated with blepharochalasis. Recurrent swelling bilaterally. Extremely rare unilateral 21. Fig 2.
- Lichenification is frequently seen in atopic dermatitis, eyelids are affected in about 15% of cases 22 Fig. 3.
- Signs of local local trauma, or insect bite 23
- Edema with vesicles is associated with herpes simplex. Vesicles can appear later in course 24.
- Orbit
- Evidence of mass effect, orbital inflammation, motor or sensory nerve involvement.
- Conjunctiva
- Chemosis.
- Salmon patch, lacrimal gland enlargement or other mass
- Pain on touch or with globe movement.

Fig.1. Yellowish discoloration of the skin in orbital xanthogranuloma

Fig 2. Cigarette paper like skin in blepharochalasis

Fig 3. Eczema and lichenification in atopic dermatitis
- Face
- Rosacea dermatitis, suggested by malar flushing, rhinophyma (Fig. 5)
- Periorbital dermatitis or vasculitis (dermatomyositis, lupus, Smarts, etc) 25
- Angioedema. Predominantly eyelids, lips and upper airways are involved. Could be acute or chronic. If acute try to avoid a causative agent. List of drugs used should be evaluated. ACE are responsible for more than 30% of cases. Ask for episodes of abdominal pain, about 93% of patients with hereditary angioedema experience recurrent abdominal pain 26. If chronic look for dietary and drug history. Screen for C1 inhibitor deficiency. Bare in mind that there is a so called type III hereditary angioedema with normal C1inhibitor with the female predominance 27
- Paralysis, fissured tongue, facial swelling suggesting Melkerson_Rosenthal syndrome 28. Fig. 4.
- Eyebrow and cheek fat enlargement associated with thyroid-associated orbitopathy 29
- Body. Look for signs of edema. Hepatic, cardiac, renal disease, hypothyroid state, low protein state are among the disorders that cause generalized edema. A hallmark of systemic edema is exacerbation of the swelling in the morning followed by gradual improvement during the day.
- Superior vena cava syndrome (SVCS). Early in clinical course may be asymptomatic. Look for minor signs. Dyspnea 63%, head fullness, cough, arm swelling, chest pain. Check for malignant mediastinal tumors, these represent more than 80% of SVCS 30.
- Nephrotic syndrome may be associated with lower extremity and eyelid edema 31.
- Eyelid swelling can be the first sign of Thyroid Eye Disease; Graves thyroid disease with goiter and hyperthyroid symptoms may be present.
- The musculoskeletal system should be evaluated in case of suspected dermatomyositis. Edema with violaceous color change. Skin changes such as heliotrope, gottron papules may be found. Proximal muscle weakness, arthralgia 32.
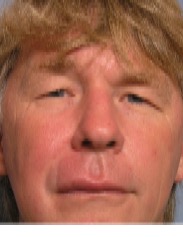
Fig.4 Melkerson-Rosenthal syndrome

Fig. 5 Rosacea and eyelid edema
Establishing the diagnosis
- Laboratory Testing: Lab tests should be based on the suspected etiologic factors. Infectious, autoimmune, renal, cardiovascular systems should evaluated. Thyroid function, CBC with differential, erythrocyte sedimentation rate, C-reactive protein, ANCA, angiotensin-converting enzyme, antinuclear antibody, lysozyme, syphilis serologies, purified protein derivative test
- Imaging: CT or MR imaging is appropriate if orbitofacial or cranial lesion is suspected as a causative factor.
- Biopsy should be solicited in case if systemic work out and imaging are inconclusive to establish the diagnosis 33.
Risk factors
- Autoimmune disease (Graves, lupus, sarcoid, vasculitis, etc)
- Atopy
- Periorbital surgery/trauma/injections
- Systemic edema
- Travel to endemic region for parasites.
- Trauma of craniofacial region cause eyelid swelling in up to 97 % of cases.
- Contact with animals (cutaneous anthrax) 34.
- Periorbital surgery
- Drugs
Differential diagnosis
- Allergy is one the most frequents causes of eyelid edema. A number of drugs have been associated with edema (Table 1.) The differential for conditions that cause edema is actually quite long. (Table 2.)
|
INFECTIOUS |
|
Herpetic 35 |
|
Chaga’s disease 36 |
|
Trichinellosis 37 |
|
Epstein–Barr virus 38, 39 |
|
Ophthalmofilariasis 40 |
|
Pott’s puffy tumor 41 |
|
Necrotising fasciitis 42 |
|
Ophthalmomyiasis 43 |
|
Blister beetle dermatitis 44 |
|
Rocky Mountain spotted fever 45 |
|
Amebiasis 46 |
|
Acute Infectious mononucleosis 47 |
|
Hepatitis B 48 |
|
Preseptal and Orbital cellulitis 49 |
|
|
|
INFLAMMATORY |
|
Thyroid Eye Disease 50 |
|
Rosacea 51, 52 |
|
Sarcoidosis 53 |
|
Idiopathic orbital inflammation 54 |
|
Cold urticaria 55 |
|
Hereditary angioedema 56 |
|
Type B Niemann–Pick disease 57 |
|
Polyarteritis nodosa 58 |
|
Relapsing polychondritis 59 |
|
Lupus erythematosus 60 |
|
Scleredema adultorum of Buschke 61 |
|
Melkersson–Rosenthal syndrome 62, 63 |
|
Juvenile dermatomyositis 32, 64 |
|
Discoid lupus 65, 66 |
|
Tumor necrosis factor receptor-associated periodic syndrome 67 |
|
Dermatographism 68 |
|
Dermatomyositis 69, 70 |
|
Tolosa–Hunt syndrome 71 |
|
Orofacial granulomatosis 72 |
|
Adult onset xanthogranuloma 73 |
|
Cutis laxa 74 |
|
GPA (Wegener’s granulomatosis) 75 |
|
Dacryoadenitis 76 |
|
|
|
NEOPLASIA |
|
Sinus and Orbital Neoplasms 77 |
|
Leukemia 78 |
|
Lymphoma (Including Mycosis Fungoides) 79 |
|
Kaposi’s sarcoma 80 |
|
Eyelid metastasis 81 |
|
Langerhans cell histiocytosis 82 |
|
Esthesioneuroblastoma 83 |
|
|
|
TRAUMA/POSTSURGICAL/POSTINJECTION |
|
Periorbital injections (e.g. fillers) 1 |
|
Lymphedema (e.g. postsurgical or post-radiation) |
|
Periorbital surgery |
|
|
|
OTHERS |
|
Superior vena cava syndrome 30 |
|
Migrane 84 |
|
Sickle cell orbital infarction 85 |
|
Protein-losing enteropathy 86 |
Patient management: treatment and follow-up
- The key is a definitive diagnosis and subsequent treatment of the causative factor.
- Allergic reaction should be managed by revealing the inciting agent. Most of the time a thorough history is the key. Antihistamines and corticosteroids may be appropriate.
- Systemic disease should be treated in conjunction with the specialist in the field.
- Post-surgical edema occurs after all surgeries. Infection, toxoallergic blepharoconjunctivitis, and rarely primary acquired cold urticaria, as well as lymphatic drainage disruption can be precipitating factors 87. Preoperative list of allergies to medications should be thoroughly taken. Minimal anatomical manipulation of lateral periorbita should be considered in order to prevent the disruption of the lymphatic drainage. Four eyelid blapharoplasty may have higher risk of prolonged post op edema if the lateral incisions are too close to each other, less than 2 mm 88.
- In the absence of a specific diagnosis, nonspecific treatment can include salt avoidance, sleeping with the head of the bed elevated, diuretics, and rarely corticosteroids.
Preventing and managing treatment complications
- Surgical intervention or any other inflammation mediators could worsen the edema.
Patient instructions
- Sleep with head elevated for fluid retention
- Avoid known allergens, or precipitating medications
- Have the list of all known allergies and inform the physician prior any treatment.
- Contact physician if worsening
References and additional resources
- Mancini R1, Taban M, et al. Use of hyaluronic Acid gel in the management of paralytic lagophthalmos: the hyaluronic Acid gel "gold weight"Ophthal Plast Reconstr Surg. 2009 Jul-Aug;25(4):259-63
- Borchard K, Puy R, Nixon R. Hyaluronidase allergy: a rare cause of periorbital inflammation. Australas J Dermatol 2010; 51:49–51.
- Procianoy F, Procianoy E. Orbital inflammatory disease secondary to a singledose administration of zoledronic acid for treatment of postmenopausal osteoporosis. Osteoporos Int 2010; 21:1057–1058.
- Rafiq R. Isolated periorbital angio-oedema induced by aspirin: a case report and review of the literature. Dent Update 2007; 34:302–304.
- Cohen PR. Irbesartan-associated persistent edema of the eyelids, face, and neck. J Drugs Dermatol 2002; 1:329–330.
- el-Azhary RA, Yiannias JA. Allergic contact dermatitis to epoxy resin in immersion oil for light microscopy. J Am Acad Dermatol 2002; 47:954–955.
- Mylonakis E, Vittorio CC, Hollik DA, Rounds S. Lamotrigine overdose presenting as anticonvulsant hypersensitivity syndrome. Ann Pharmacother 1999; 33:557–559.
- Fraunfelder F, Fraunfelder F, Chambers W. Clinical Ocular Toxicology. Philadelphia: Elsevier Saunders; 2008. pp. 343–344.
- Visscher AJ, Cohen D. Periorbital oedema and treatment-resistant hypertension as rare side effects of clozapine. Aust N Z J Psychiatry 2011; 45:1097–1098.
- Eguia B, Ruppert AM, Fillon J, et al. Skin toxicities compromise prolonged pemetrexed treatment. J Thorac Oncol 2011; 6:2083–2089.
- Soumya RN, Grover S, Dutt A, Gaur N. Angioneurotic edema with risperidone: a case report and review of literature. Gen Hosp Psychiatry 2010; 32:646; e641–e643.
- Pelizza L. Long-acting risperidone-induced periorbital edema. J Clin Psychopharmacol 2008; 28:709–710.
- McClelland CM, Harocopos GJ, Custer PL. Periorbital edema secondary to imatinib mesylate. Clin Ophthalmol 2010; 4:427–431.
- Larson JS, Bergstrom LK, Cameron JD, et al. Severe periorbital edema secondary to imatinib mesylate for chronic myelogenous leukemia. Arch Ophthalmol 2007; 125:985–986.
- Balas M, Plakogiannis R, Sinnett M. Periorbital edema associated with separate courses of ibuprofen and naproxen. Am J Health Syst Pharm 2010; 67:906–909.
- Park HS, Nahm D. Localized periorbital edema as a clinical manifestation of sulfite sensitivity. J Korean Med Sci 1996; 11:356–357.
- Friedland S, Kaplan S, Lahav M, Shapiro A. Proptosis and periorbital edema due to diltiazem treatment. Arch Ophthalmol 1993; 111:1027–1028.
- Curran CF, Luce JK. Ocular adverse reactions associated with Adriamycin (doxorubicin). Am J Ophthalmol 1989; 108:709–711.
- Cohen AY, Frank G. Periorbital edema after atracurium administration. Anesthesiology 1987; 66:431–432.
- Tordjman K, Rosenthal T, Bursztyn M. Nifedipine-induced periorbital edema. Am J Cardiol 1985; 55:1445.
- R M Manners, J R Collin. Localised unilateral blepharochalasis. Br J Ophthalmol. 1994 Nov; 78(11): 881–882.
- Rich, LF, Hanifin, JM. Ocular complications of AD, and other eczemas. Int Ophthalmol Clin. 1985;25:61–76.
- Quach KA, Zaenglein AL. The eyelid sign: a clue to bed bug bites. Pediatr Dermatol. 2014 May-Jun;31(3):353-5
- Kurimoto T, Tonari M, Ishizaki N, et al. Orbital apex syndrome associated with herpes zoster ophthalmicus. Clin Ophthalmol 2011;5:1603-8
- Chen DM1, Crosby DL. Periorbital edema as an initial presentation of rosacea. J Am Acad Dermatol. 1997 Aug;37(2 Pt 2):346-8.
- M Aamir Ali, Marie L Borum. Hereditary angioedema: what the gastroenterologist needs to know.Clin Exp Gastroenterol 2014 20;7:435-45. Epub 2014 Nov 20.
- Riedl MA1. Hereditary angioedema with normal C1-INH (HAE type III). J Allergy Clin Immunol Pract. 2013 Sep-Oct;1(5):427-32.
- Rawlings NG1, Valenzuela AA, Allen LH, Heathcote JG. Isolated eyelid edema in Melkersson-Rosenthal syndrome: a case series. Eye (Lond). 2012 Jan;26(1):163-6. doi: 10.1038/eye.2011.285. Epub 2011 Nov 4.
- Papageorgiou KI1, Hwang CJ, et al. Thyroid-associated periorbitopathy: eyebrow fat and soft tissue expansion in patients with thyroid-associated orbitopathy.Arch Ophthalmol. 2012 Mar;130(3):319-28.
- Escalante CP1. Causes and management of superior vena cava syndrome. Oncology (Williston Park). 1993 Jun;7(6):61-8; discussion 71-2, 75-7.
- Meyer-Lehnert H, Vetter H. Eyelid and ankle edema. Schweiz Rundsch Med Prax. 1990 Mar 6;79(10):296-300.
- Taban M1, Perry JD. Juvenile dermatomyositis presenting with periorbital edema.Ophthal Plast Reconstr Surg. 2006 Sep-Oct;22(5):393-5.
- Pandya VB1, Conway RM, Taylor SF. Primary cutaneous B cell lymphoma presenting as recurrent eyelid swelling.Clin Experiment Ophthalmol. 2008 Oct;36(7):672-4.
- Tekin R1, Ari S, Dal T, Kaya S, Kortak MZ, Dursun B, Dayan S. Evaluation of cutaneous palpebral anthrax. Cutan Ocul Toxicol. 2013 Oct;32(4):294-8.
- Differential Diagnosis of the Swollen Red Eyelid Papier A,Tuttle D, Mahar T, MD Am Fam Physician. 2007 Dec 15;76(12):1815-1824.
- Bastos CJ, Aras R, Mota G, et al. Clinical outcomes of thirteen patients with acute Chagas disease acquired through oral transmission from two urban outbreaks in northeastern Brazil. PLoS Negl Trop Dis 2010;4:e711.
- Kennedy ED, Hall RL,Montgomery SP, et al. Trichinellosis surveillance: United States, 2002–2007. MMWR Surveill Summ 2009; 58:1–7.
- Decker GR, Berberian BJ, Sulica VI. Periorbital and eyelid edema: the initial manifestation of acute infectious mononucleosis. Cutis 1991; 47:323–324.
- Bass MH. Periorbital edema as the initial sign of infectious mononucleosis. J Pediatr 1954; 45:204–205.
- Gregory AR, Schatz S, Laubach H. Ophthalmomyiasis caused by the sheep bot fly Oestrus ovis in northern Iraq. Optom Vis Sci 2004; 81:586–590.
- Morley AM. Pott’s puffy tumour: a rare but sinister cause of periorbital oedema in a child. Eye (Lond) 2009; 23:990–991.
- Balaggan KS, Goolamali SI. Periorbital necrotising fasciitis after minor trauma. Graefes Arch Clin Exp Ophthalmol 2006; 244:268–270.
- Fodor E, Fok E, Maka E, et al. Recently recognized cases of ophthalmofilariasis in Hungary. Eur J Ophthalmol 2009; 19:675–678.
- Poole TR. Blister beetle periorbital dermatitis and keratoconjunctivitis in Tanzania. Eye (Lond) 1998; 12 (Pt 5):883–885.
- Park JM, Ahn SY, Shin JI, et al. A systemic lupus erythematosus patient with protein losing enteropathy. Yonsei Med J 2004; 45:923–926.
- Baez Mendoza J, Ramirez Barba EJ. Cutaneous amebiasis of the face: a case report. Am J Trop Med Hyg 1986; 35:69–71.
- Gomez-Puerta JA, Levy S, Khamashta MA, Hughes GR. Periorbital oedema in systemic lupus erythematosus. Lupus 2003; 12:866–869.
- van Aalsburg R, de Pagter AP, van Genderen PJ. Urticaria and periorbital edema as prodromal presenting signs of acute hepatitis B infection. J Travel Med 2011; 18:224–225.
- Bedwell J1, Bauman NM. Management of pediatric orbital cellulitis and abscess. Curr Opin Otolaryngol Head Neck Surg. 2011 Dec;19(6):467-73.
- Ayabe R, Rootman DB, Hwang CJ, Ben-Artzi A, Goldberg R.Adalimumab as steroid-sparing treatment of inflammatory-stage thyroid eye disease. Ophthal Plast Reconstr Surg. 2014 Sep-Oct;30(5).
- Chen DM, Crosby DL. Periorbital edema as an initial presentation of rosacea. J Am Acad Dermatol 1997; 37 (2 Pt 2):346–348.
- Morales-Burgos A, Alvarez Del Manzano G, Sanchez JL, Cruz CL. Persistent eyelid swelling in a patient with rosacea. P R Health Sci J 2009; 28:80–82.
- Yaosaka M, Abe R, Ujiie H, et al. Unilateral periorbital oedema due to sarcoid infiltration of the eyelid: an unusual presentation of sarcoidosis with facial nerve palsy and parotid gland enlargement. Br J Dermatol 2007; 157:200–202.
- Krymchantowski AV, Oliveira T, Bigal ME. Side-locked headache as the chief complaint of inflammatory orbital pseudotumor (myositic form): a case report. Headache 2006; 46:683–686.
- Burroughs JR, Patrinely JR, Nugent JS, et al. Cold urticaria: an underrecognized cause of postsurgical periorbital swelling. Ophthal Plast Reconstr Surg 2005; 21:327–330.
- Bork K, Craig TJ, Bernstein JA, Feuersenger H, Machnig T, Staubach P. Efficacy of C1 esterase inhibitor concentrate in treatment of cutaneous attacks of hereditary angioedema.Allergy Asthma Proc. 2015 Mar 23.
- Filling-Katz MR, Fink JK, Gorin MB, et al. Ophthalmologic manifestations of type B Niemann-Pick diseases. Metab Pediatr Syst Ophthalmol 1992; 15:16–20.
- Fernandes SR, Coimbra IB, Costallat LT, Ribeiro Filho JE. Uncommon features of polyarteritis nodosa: psychosis and angio-oedema. Clin Rheumatol 1998;17:353–356.
- Alatas F, Ozkan R, Metintas M, et al. Relapsing polychondritis. Respirology 2003; 8:99–103.
- Ghaninejad H, Kavusi S, Safar F, et al. Persistent periorbital edema as a sole manifestation of cutaneous lupus erythematosus: report of two cases. Dermatol Online J 2006; 12:14.
- Ioannidou DI, Krasagakis K, Stefanidou MP, et al. Scleredema adultorum of Buschke presenting as periorbital edema: a diagnostic challenge. J Am Acad Dermatol 2005; 52 (2 Suppl 1):41–44.
- Akarsu C, Atasoy P, Erdogan S, Kocak M. Bilateral upper eyelid edema in Melkersson-Rosenthal syndrome. Ophthal Plast Reconstr Surg 2005; 21:243–245.
- Cocuroccia B, Gubinelli E, Annessi G, et al. Persistent unilateral orbital and eyelid oedema as a manifestation of Melkersson-Rosenthal syndrome. J Eur Acad Dermatol Venereol 2005; 19:107–111.
- Dwivedi N, Michael C, Lew DB, et al. A fatal presentation of dermatomyositis with facial swelling. Int J Pediatr Otorhinolaryngol 2012; 76:745–749.
- Braun RP, French LE, Massouye I, Saurat JH. Periorbital oedema and erythema as a manifestation of discoid lupus erythematosus. Dermatology 2002; 205:194–197.
- Park JM, Ahn SY, Shin JI, et al. A systemic lupus erythematosus patient with protein losing enteropathy. Yonsei Med J 2004; 45:923–926.
- Cantarini L, Rigante D, Lucherini OM, et al. Role of etanercept in the treatment of tumor necrosis factor receptor-associated periodic syndrome: personal experience and review of the literature. Int J Immunopathol Pharmacol 2010;23:701–707.
- Gupta S, Aakalu VK, Sajja K, et al. Periorbital physical urticaria in an anophthalmic patient with dermatographism. Ophthal Plast Reconstr Surg 2011; 27:e20–e21.
- Dicken CH. Periorbital edema: an important physical finding in dermatomyositis. Cutis 1991; 48:116–117.
- Hall VC, Keeling JH, Davis MD. Periorbital edema as the presenting sign of dermatomyositis. Int J Dermatol 2003; 42:466–467.
- Lachanas VA, Karatzias GT, Tsitiridis I, et al. Tolosa-Hunt syndrome misdiagnosed as sinusitis complication. J Laryngol Otol 2008; 122:97–99.
- Mignogna MD, Fedele S, Lo Russo L, Lo Muzio L. The multiform and variable patterns of onset of orofacial granulomatosis. J Oral Pathol Med 2003; 32:200–205.
- Kiratli H, Kiliç M, Tarlan B, Söylemezoglu F.Adult orbital xanthogranulomas: clinical features and management. Eur J Ophthalmol. 2015 Jan 15:0
- Fatmi LE, Haque MS, Mollah AH, et al. Cutis laxa: a case report and an update. Mymensingh Med J 2010; 19:137–141.
- Vanwynsberghe D1, Van Den Broecke C, Bauters W, Decock C. Ocular presentation of Wegener granulomatosis. Bull Soc Belge Ophtalmol. 2007;(303):7-11.Ricketti AJ1, Cleri DJ, Moser RL, Bilyk JR, Vernaleo JR, Unkle DW. A 44-year-old man with bilateral eyelid swelling.Allergy Asthma Proc. 2012 Mar-Apr;33(2):205-11.Hammami B1, Mnejja M, Chakroun A, Achour I, et al. Cholesteatoma of the frontal sinus.Eur Ann Otorhinolaryngol Head Neck Dis. 2010 Dec;127(6):213-6.
- Nusz KJ, Pang NK, Woog JJ. Periorbital edema as the initial presentation of T-cell prolymphocytic leukemia. Ophthal Plast Reconstr Surg 2006; 22:215–216.
- Dragan LR, Baron JM, Stern S, Shaw JC. Solid facial edema preceding a diagnosis of retro-orbital B-cell lymphoma. J Am Acad Dermatol 2000; 42 (5 Pt 2):872–874.
- Harrison M, Tomlinson D, Stewart S. Periorbital edema in Kaposi’s sarcoma. N Engl J Med 1995; 333:799–800.
- Martorell-Calatayud A, Requena C, Diaz-Recuero JL, et al. Mask-like metastasis: report of 2 cases of 4 eyelid metastases and review of the literature. Am J Dermatopathol 2010; 32:9–14.
- Wladis EJ, Tomaszewski JE, Gausas RE. Langerhans cell histiocytosis of the orbit 10 years after involvement at other sites. Ophthal Plast Reconstr Surg 2008; 24:142–143.
- Rakes SM, Yeatts RP, Campbell RJ. Ophthalmic manifestations of esthesioneuroblastoma.Ophthalmology 1985; 92:1749–1753.
- May A1, Evers S, Straube A, Pfaffenrath V, Diener HC; Deutschen Migräne- und Kopfschmerzgesellschaft. Treatment and prophylaxis for cluster headaches and other trigeminal autonomic headaches. Revised recommendations of the German Migraine and Headache Societ 2005 Jun;19(3):225-41.
- Ganesh A, Al-Zuhaibi S, Pathare A, et al. Orbital infarction in sickle cell disease. Am J Ophthalmol 2008; 146:595–601.
- Dyken JR, Pagano JP, Soong VY. Superior vena caval syndrome presenting as periorbital edema. J Am Acad Dermatol 1994; 31 (2 Pt 1):281–283.
- Nield LS. Milk intolerance presenting solely as periorbital edema. Clin Pediatr (Phila) 1995; 34:265–267.
- Stephen R. Klapper1 , James R. Patrinely2 Management of Cosmetic Eyelid Surgery Complications Seminars in Plastic Surgery 2007; 21(1): 080-093.Soparkar CS, Patrinely JR. Palpebral surgical approaches for orbital fracture repair Semin Plast Surg 2002; 16: 273-282
- Additional Resources
- AAO, Basic and Clinical Science Course. Section 7. Orbit, Eyelids & Lacrimal system, 2014.
- Eyelid edema. Sami, MS, Soparkar CNS, Patrinely JR, Tower RN. Semin Plast Surg. 2007 February; 21(1): 24–31.
- Differential Diagnosis of the Swollen Red Eyelid ART PAPIER, MD; DAVID J. TUTTLE, MD; and TARA J. MAHAR, MD Am Fam Physician. 2007 Dec 15;76(12):1815-1824.
- Periorbital edema: a puzzle no more? Rachel K. Sobela, Keith D. Carter, and Richard C. Allen. Curr Opin Ophthalmol. 2012 Sep;23(5):405-14.
Financial disclosures
Reviewers
Simeon Lauer: No disclosures
