Horizontal Eyelid Tightening
Updated August 2024
Indications and contraindications
Indications
- Involutional ectropion
- Involutional entropion
- Cicatricial ectropion
- Cicatricial entropion
- Congenital ectropion
- Congenital entropion
- Eyelid reconstruction after tumor removal
- Cosmetic improvement in postblepharoplasty rounded lateral canthus
- Floppy eyelid syndrome
- Flaccid lower lids with poor tear pump mechanism and symptomatic tearing
Contraindications
- Absence of sufficient tissue to tighten lids
- Patients with prominent eyes and maxillary hypoplasia
- In patients with these conditions, horizontal tightening may induce retraction and worsen keratopathy.
Preprocedure evaluation
- Review past medical and surgical history.
- Especially previous eyelid and orbital surgery and/or trauma
- Use of anticoagulants
- Recent intraocular surgery or ongoing disease
- Complete eye examination, paying particular attention to the ocular surface.
- Evaluate lid and orbit:
- Anterior lamella: integrity and adequacy
- Posterior lamella: integrity and adequacy
- Position of puncta: Note ectropion or stenosis.
- Recognition of maxillary vector: Negative vector is noted when the inferior orbital rim lies posterior to the lower lid margin.
- Evaluate potential donor sites, for example, hard palate, upper lid, periauricular, supraclavicular.
- Consult with patient’s primary care/prescribing physician if the patient takes medically-indicated blood thinners.
Alternatives to procedure
- Lower-eyelid retractor surgery: appropriate if retractor scarring is the primary problem
- Midface lift can be helpful as an alternative to skin graft when the anterior lamella is inadequate.
- Malar augmentation can be helpful when negative vector is present.
- Observation
Instrumentation, anesthesia, and technique
Instrumentation:
- Wescott and Stevens scissors
- Cautery
- Forceps
- Sutures
- Periosteal elevator
Anesthesia:
- Most can be performed with local anesthesia, in an office or operating room setting.
- Sedation if needed for patient comfort
Technique:
Lower-eyelid canthoplasty:
- Perform lateral canthotomy and inferior cantholysis with Stevens or Wescott scissors.
- Determine amount of horizontal tightening of lower lid by redraping to the lateral canthal crus.
- Excise full thickness wedge resection of the lateral aspect of lower lid.
- Secure lower lid to intact superior lateral canthal tendon (Figure 1).
- Close skin.
Lateral tarsal strip (Figure 2):
- Perform lateral canthotomy and inferior cantholysis with Stevens or Wescott scissors.
- Determine amount of horizontal tightening of lower lid by redraping to the lateral canthal crus.
- Score lid margin at medial extent of potential lateral tarsal strip.
- Release septum and inferior retractors from inferior aspect of lower lid.
- Divide anterior and posterior lamellae lateral to scored lid margin.
- Remove mucocutaneous junction of eyelid laterally.
- Scrape conjunctiva from the posterior aspect of strip.
- Fixate to periosteum of internal lateral orbital rim at approximate site of Whitnall’s tubercle with sutures—for example, horizontal mattress suture.
- Place gray line suture.
- Close skin.
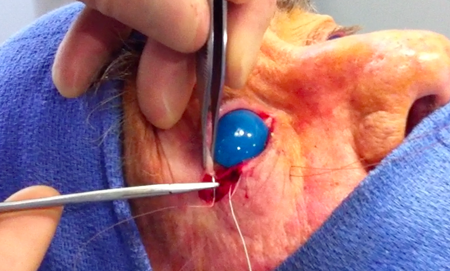
Figure 1. Fixation of the lower lid to the intact superior lateral canthal tendon.
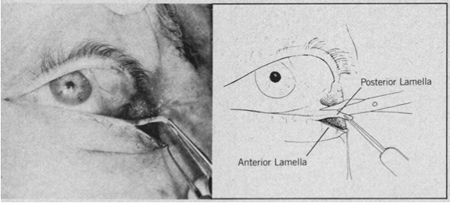
Figure 2. Formation of the lateral tarsal strip (from Anderson and Gordy 1979).
Lateral canthopexy:
- Entire canthus is moved by changing its attachment from the eyelid to the lateral orbital wall.
- To elevate or depress the canthus en bloc:
- Make a Z-plasty incision at lateral canthus (Figure 3).
- Dissect to periosteum where it is incised and perform a subperiosteal dissection to release the canthus en bloc (Figure 4).
- Mark the lateral orbital rim at the desired canthal position at the intended site of the canthus.
- Insert a malleable retractor to protect the globe.
- Use a drill to pass from interior to exterior of the lateral orbital rim.
- Use a permanent suture or metal wire to engage the body of the canthus, and then pass it through the hole(s).
- If you made 2 drill holes, tie the suture or wire to itself over the bridging bone.
- If you made 1 drill hole, pass the suture into the temporalis tissue and tie.
- Rotate the arms of Z-plasty with layered closure.

Figure 3. Marking of the Z-plasty.
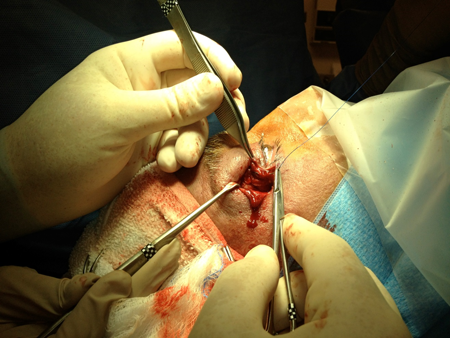
Figure 4. En bloc elevation of lateral canthus via subperiosteal dissection and placement of permanent suture through the canthal body.
- To secure either the upper or lower lid to bone
- Perform a lateral canthotomy and inferior cantholysis with Stevens or Wescott scissors.
- Determine the amount of horizontal tightening of the lower lid by redraping to the lateral canthal crus.
- Score lid margin at medial extent of potential lateral tarsal strip.
- Release septum and inferior retractors from inferior aspect of lower lid.
- Divide anterior and posterior lamellae lateral to scored lid margin.
- Remove mucocutaneous junction of eyelid laterally.
- Scrape conjunctiva from posterior aspect of strip.
- Incise periosteum and elevate it over the internal and external lateral orbital rim at the site of fixation.
- Insert a malleable retractor to protect the globe.
- Use a drill to pass from interior to exterior of the lateral orbital rim.
- Use a permanent suture or metal wire to engage the body of the canthus, and then pass it through the hole(s).
- If you made 2 drill holes, tie the suture or wire to itself over the bridging bone.
- If you made 1 drill hole, pass the suture into the temporalis tissue and tie.
Special circumstances:
- Tissue augmentation might be needed in cicatricial disease.
- Partial/split-thickness skin grafting for anterior lamellar deficiencies
- Hard palate or acellular dermal matrix graft for posterior lamellar deficiencies
- Lazy “T” for lower-lid laxity and punctal ectropion
- Traction suture to lower lid is initially placed
- Insert a lacrimal probe in lower punctum and canaliculus.
- Excise conjunctiva/retractors/septum to orbicularis in form of medial spindle of 7 mm x 10 mm.
- A vertical incision is made through lid margin about 5 mm lateral to inferior punctum
- Redrape lid medially to determine amount of excess
- Perform a full-thickness wedge resection of lower lid
- Bury the closure of conjunctiva.
- Closure of full thickness margin using usual techniques
- Upper-eyelid horizontal tightening
- Upper eyelid canthoplasty
- Perform a lateral canthotomy and superior cantholysis with Stevens or Wescott scissors.
- Determine amount of horizontal tightening of upper lid by redraping to the lateral canthal crus.
- Excise full-thickness wedge resection of the lateral aspect of upper lid.
- Secure lower lid to intact inferior lateral canthal tendon.
- Close skin.
- Pentagonal wedge resection of upper eyelid
- Mark medially on lid margin to lid crease about 5 mm lateral to punctum and about 10 mm lateral the initial site depending on laxity.
- If concurrent upper-lid blepharoplasty will be performed, construct the apex of the pentagonal wedge to assimilate to the blepharoplasty incision.
- Use Stevens scissors to excise the previously marked full-thickness portion of the eyelid; incision must extend through entire vertical dimension of tarsus.
- Close as full thickness eyelid laceration.
Preventing and managing complications
- Intraoperative
- Bleeding
- Failure to fixate tarsal strip to periosteum or bone
- The suture should pass through the periosteum, creating a tactile “gritty sensation.”
- Some surgeons gently lift the suture to ensure adequate tension.
- Malposition of eyelid with lid under equator of globe, especially in those with shallow orbits, prominent eyes, and maxillary hypoplasia
- Postoperative
- Bleeding
- Retrobulbar hemorrhage with visual loss
- Infection: very low incidence, reported at 0.04% (Lee OPRS 2009)
- Wound dehiscence
- Recurrence of ectropion or entropion
- Lid notching in upper-lid pentagonal wedge resection
- Prevention of complications
- Stop blood thinners if medically cleared with primary physician.
- Careful attention to hemostasis
- Careful dissection to ensure adequate lateral fixation
- Management of complications
- Drain orbital hemorrhage immediately.
- Treat infections with antibiotics.
- Reoperate if there is a recurrence or dehiscence.
Patient instructions
- Use antibiotic ointment on wounds as directed.
- Keep wounds dry and clean.
- Apply cold to incisions Q1hr x 72 hours.
- Come back immediately if bleeding, proptosis, significant pain, or loss of vision.
- Return within 1 week for suture removal.
References and additional resources
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System. 2010-11.
- Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979; 97:2192-6.
- Barrett, RV, Meyer, DR. The modified Bick quick strip procedure for surgical treatment of eyelid malposition. Ophthal Plast Reconstr Surg. 2012; 28(4): 294-9.
- Callahan M., Callahan, A. Ophthalmic Plastic and Orbital Surgery, Aesculapius Publishing, 1979
- Lee EW et al. Infection rates in outpatient eyelid surgery. Ophthal Plast Reconstr Surg. 2009; 25:109-10.
- Valenzuela, AA, Sullivan, TJ. Medial upper eyelid tightening to correct medial eyelid laxity in floppy eyelid syndrome: a new surgical approach. Ophthal Plast Reconstr Surg. 21(4): 259-263.
