Internal (Transconjunctival) Levator/Mullers Muscle Resection Approaches for Ptosis
Updated August 2024
Goals, indications, contraindications
- Primary goal: Improvement of superior and peripheral visual field
- Secondary goal: Improved functioning in daily activities, aesthetic improvement and symmetry of lids, avoidance of skin incision
- Indications
- For patients with ptosis whose upper lids raise to normal levels with instillation of 2.5% phenylephrine drops
- Minimal to moderate congenital ptosis
- Minimal to moderate acquired ptosis, usually with minimal dermatochalasis (Figure 1)
- Cosmetic patients interested in avoiding scars
- Horner syndrome
- Contraindications — all relative
- Eyelids that do not raise to satisfactory levels with 2.5% phenylephrine drops
- Anophthalmic ptosis repair in socket contracture
- Severe ptosis
- Conjunctival inflammatory/cicatricial disease that is active or not well-controlled
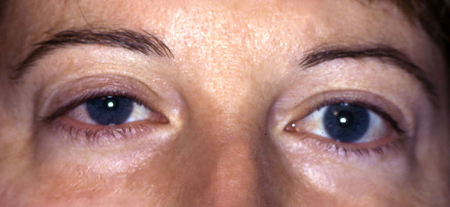
Figure 1. Minimal right upper lid ptosis with mild dermatochalasis that would not require blepharoplasty.
Preprocedure evaluation
Patient history
- Presentation for a troublesome ptosis
- Trauma
- Rapid or insidious onset
- Associated diplopia
- Generalized weakness
- Difficulty swallowing
- Visual obstruction/effect on daily activities
- Variable or fluctuating symptoms
Clinical examination
- Levator function
- Amount of ptosis (margin reflex distance (MRD1))
- Motility evaluation
- Pupillary evaluation (miosis, anisocoria)
- Bell’s reflex
- Corneal sensation
- Tear film, tear meniscus height, tear break up time
- Basal secretion – Schirmer test
- Lagophthalmos
- Minimal dermatochalasis
- Eyelid contour
- 5% phenylephrine test
Preoperative assessment
- If the eyelid raises to a normal level with phenylephrine, approximately 8 mm of conjunctiva and Müller muscle is resected, based on numerous algorithms and charts in the literature.
- If lower than the fellow eyelid, 9–10 mm is often resected.
- If higher than the fellow eyelid, 6–7 mm is resected.
Palpation along superior rim
Procedure alternatives
- External levator resection or advancement
- Fasanella-Servat tarsectomy
Surgical techniques
Anesthesia
- Anesthetic infiltration
Technique
- Eversion of upper eyelid over a Desmarres retractor
- Calipers used to mark one-half the desired number of mm resected above the superior tarsus; markings placed centrally, medially, and laterally (Figure 2)
- Three silk marking sutures are placed into the conjunctiva and deep to the Müller muscle at these markings such that when elevated at these half-markings, the total removed will be the desired excision amount.
- Avoid incorporating the levator complex with the marking sutures.
- The conjunctiva and Müller muscle are grasped with a forceps to separate it from the underlying levator aponeurosis.
- The traction sutures are elevated and the Putterman clamp grasps the folded elevated tissues flush to the superior tarsal border.
- A double-armed 5-0 plain gut running suture is preplaced between superior tarsus and conjunctiva/Müller just below the clamp (Figure 3).
- The clamped tissues in the clamp are excised with a 15-blade scalpel directed against the clamp so as not to cut the plain suture (Figure 4).
- The conjunctiva is closed by running the previously placed plain suture.
- Overlying levator complex effectively is imbricated and elevates the lid.
- Alternatively, prolene suture can be used and the 2 ends tied externally over skin.
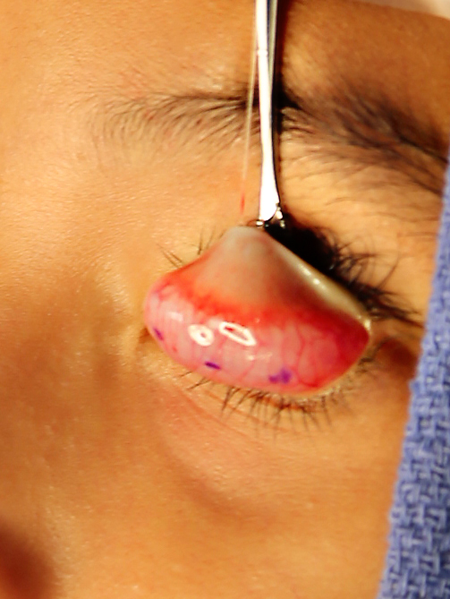
Figure 2. Upper lid is everted over a Desmarres retractor and half the desired resection amount is marked at three sites.
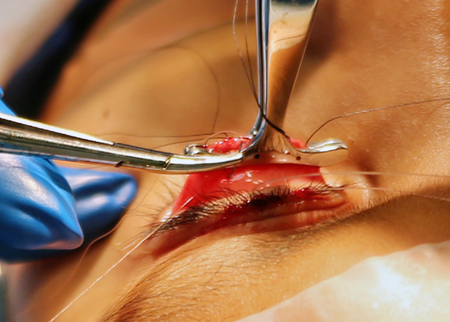
Figure 3. Suture is passed below the clamp, thus securing the superior edge of the conjunctive/Muller muscle to the superior tarsus.
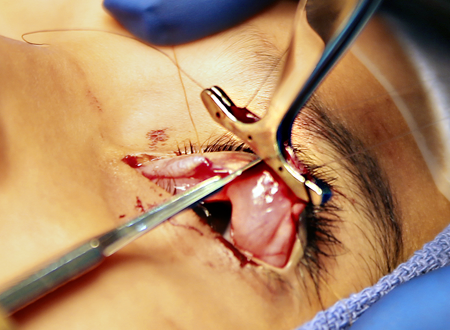
Figure 4. Scalpel excises the enclosed tissues, taking care to avoid cutting the pre-placed sutures.
Patient management: treatment and follow-up
Postoperative instructions
- Apply cold compresses for 48 hours postoperatively to minimize edema and ecchymosis.
- Lubricate the cornea with artificial tears liberally until normal blink returns.
- Elevate head of bed for 1 week.
- No strenuous activity, lifting, or bending for 1 week
- Avoid rubbing the face and lids for 1–2 weeks to avoid dehiscence.
- Follow-up visit in several days to 1 week after surgery
- Evaluate lid position, lid closure, corneal surface, wound healing, infection.
Medications prescribed
Antibiotic ointment can be applied to ocular surface 2–4 times a day for 1–2 weeks. This might blur vision temporarily, but minimizes discomfort from sutures.
Other management considerations
Patient should call the office for any sudden bleeding that does not stop, or for worsened pain, tenderness, purulent discharge, fever, or decrease in vision.
Nonessential vitamins and herbals that might risk bleeding should be discontinued for 1–2 weeks after the procedure.
Aspirin and NSAIDS can be resumed judiciously within several days to a week postoperatively depending on medical need.
Common treatment responses, follow-up strategies
Ecchymosis is common for 1–2 weeks after surgery, although much less than with external approach.
Edema can take several months for complete resolution, although first few weeks are most noticeable.
Mild asymmetry within first few weeks might be secondary to edema and can be observed for spontaneous improvement.
Large asymmetry might need revision in the operating room.
Preventing and managing treatment complications
Corneal abrasion due to posterior lid suture
- Place closer bites on the tarsus and farther apart on the conjunctival surface.
- Bury the knot or externalize the suture ends.
- Place a soft contact lens for 7 days until suture absorbs.
Overcorrection
- Massage downward during the immediate postoperative period.
- Levator recession procedure
- Early suture removal
Abnormal contour
- Segmental internal ptosis repair or small-incision external levator approach at the site of desired elevation
Undercorrection
- External levator resection
- Small repeat internal ptosis repair, but may shorten fornix
Dry eye symptoms
- Lubrication
- Punctal plugs or cautery
Disease-related complications
Short-term
- Infection
- Corneal abrasion
- Hemorrhage, ecchymosis
- Loss of vision
- Asymmetry
- Overcorrection, undercorrection
- Dry eyes
- Temporary exposure keratitis
Long-term
- Lagophthalmos
- Dry eyes due to removal of conjunctival and tarsal glands
- Shortening of fornix (may affect prosthesis in anophthalmic patient)
- Recurrence
- Abnormal contour
- Need for additional surgery
Historical perspective
Fasanella-Servat
(Fasanella RM)
- Described in 1961 in which a curved hemostat was used to clamp the tarsus prior to excision
- Typically reserved now for patients with minimal ptosis (1-2mm) and a negative phenylephrine test
Müller muscle-conjunctiva resection technique
(Putterman AM, Dresner SC)
- Originally described in 1975 by Putterman and Urist, with many modifications and formulas subsequently
- Preserves tarsus, thus eliminating risks associated with tarsal excision (dry eyes, contour abnormality, loss of lid integrity)
Conjunctivomullerectomy with limited tarsectomy
(Linberg JV, Perry JD)
- Modification that includes benefits from both the conjunctivomullerectomy with a calculated amount of limited tarsal resection
- A graded levator advancement technique can be performed simultaneously.
References and additional resources
- AAO, Surgery of the Eyelid, Orbit & Lacrimal system, Vol. 2, 1994, p.124-125.
- AAO, Focal Points: Management of Acquired Ptosis, Module #8, 1999, p.6.
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2013-14.
- Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA. External levator advancement vs Müller’s muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol 2005;140:426-32.
- Buckman G, Jackobiec FA, Hyde K, Lisman RD, Hornblass A, Harrison W. Success of Fasanella-Servat operation independent of Muller’s muscle excision. Ophthalmology 1989;96:413-8.
- Cohen AJ, Weinberg DA. Müller’s muscle-conjunctival resection for blepharoptosis with poor levator function. Ophthalmic Surg Lasers 2002;33:491-2.
- Dresner SC. Further modifications of the Muller’s muscle-conjunctival resection procedure for the blepharoptosis. Ophthalmic Plast Reconstr Surg 1991;7:114-22.
- Fasanella RM, Servat J. Levator resection for minimal ptosis: another simplified operation. Arch Ophthalmol 1961;65:493-6.
- Glatt HJ, Fett DR, Putterman AM. Comparison of 2.5% and 10% phenylephrine in the elevation of upper eyelids with ptosis. Ophthalmic Surg 1990;21:173-6.
- Glatt HJ, Putterman AM, Fett DR. Muller’s muscle-conjunctival resection procedure in the treatment of ptosis in Horner’s syndrome. Ophthalmic Surg 1990;21:93-6.
- Karesh JW, Putterman AM, Fett DR. Conjunctiva-Müller’s muscle excision to correct anophthalmic ptosis. Ophthalmology 1986;93: 1068-71.
- Kiyoshi M. Stretching the Muller muscle results in involuntary contraction of the levator muscle. Ophthalmic Plast Reconstr Surg 2002;18:5-10.
- Patel SM, Linberg JV, Sivak-Callcott JA, Gunel E. Modified tarsal resection operation for congenital ptosis with fair levator function. Ophthal Plast Reconstr Surg 2008; 24(1):1-6.
- Perry JD, Kadakia A, FosterJA. A new algorithm for ptosis repair using conjunctival Müllerectomy with or without tarsectomy. Ophthal Plast Reconstr Surg 2002;18:426-9.
- Putterman AM, Urist MJ. Müller muscle-conjunctiva resection. Technique for treatment of blepharoptosis. Arch Ophthalmol 1975;93:619-23.
- Putterman AM, Urist MJ. Müller’s muscle-conjunctival resection ptosis procedure. Ophthalmic Surg 1978;9:27-32.
- Putterman AM, Fett DR. Müller’s muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg 1986;17:354-60.
- Samimi DB, Erb MH, Lane CJ, Dresner SC. The modified fasanella-servat procedure: description and quantified analysis. Ophthal Plast Reconstr Surg 2013; 29(1):30-4.
