Intraorbital Foreign Bodies
Updated May 2024
Establishing the diagnosis
Etiology
- Occupational trauma: hammering metal on metal, grinding, nail guns, barbed wire
- High-velocity projectiles: firearms, BB, pellet guns
- Organic materials: tree branches, cacti, other thorny vegetation
- Resulting from lawn mowing or other gardening activity
- Falling and being impaled by object
- Nighttime activities frequently involving running
- Objects that are less than the diameter of the bony orbital entrance that have a pointed end and can be projectile in nature: fish hooks, blow darts, arrowheads
- Blast injuries with resultant building debris, particulate matter, or adjacent anatomy such as teeth
- Motor vehicle related accidents
- Assault with a relatively sharp object, e.g., pencils, ballpoint pens, fingernails, plastic fork, knife
- Protective eyewear frequently not worn
Epidemiology
- More common in children and adults younger than 30
- Males more than females
History
- Take a thorough history of the event, including any seemingly incidental trauma, especially in children. Notably, organic material may present well after the inciting injury with fistulas/tracts, granuloma formation or abscess (Fulcher, Ophthalmology, 2002)
- Mechanism of injury (velocity and size of object) with a high index of suspicion when patient reports self-removal of penetrating object as well as in unconscious, intoxicated, and pediatric patients
- Larger, low-velocity objects tend to displace the globe.
- Smaller, higher-velocity objects tend to perforate the globe, ending up in the posterior orbit.
- Composition of foreign body
- Metallic, inorganic, e.g., steel, nickel (Figure 1)
- Nonmetallic, inorganic, e.g., plastic, glass
- Nonmetallic, organic, e.g., tree branch, thorn
- Use of protective eyewear
- Decreased vision or gaze-evoked amaurosis
- Floaters, flashes of light
- Diplopia
- Pain or pain on eye movement
- Fever, chills, neurologic deficits
- Tetanus immunization status

Figure 1. BB-gun pellet. Courtesy Brett Davies, MD.
Clinical features
- External injury might initially seem trivial with small or occult entry wound.
- Decreased vision might indicate associated ocular injury or traumatic optic neuropathy.
- Afferent pupillary defect (APD): traumatic optic neuropathy, optic nerve avulsion
- Decreased ocular motility
- Blepharoptosis
- Orbital fat visualized through eyelid laceration indicating septal penetration
- Periorbital edema and ecchymosis
- Subconjunctival hemorrhage or conjunctival discharge, uveal prolapse
- Perform close inspection of fornices for occult conjunctival entrance wound.
- Chronic, unresponsive or recurrent conjunctivitis following completion of antibiotic course of treatment
- Proptosis or globe dystopia
- Fistula formation with discharge or extruding foreign body
- Subcutaneous palpable mass
- Intraocular injuries: commotio retinae, choroidal rupture, retinal sclopetaria, vitreous hemorrhage, posterior globe indentation, globe perforation
- Mental status changes: subdural hemorrhage, intracranial penetration, pulsatile proptosis
Testing
- Complete eye exam with close attention to vision, pupils, motility, globe integrity, and careful inspection of the periorbita looking for entrance wound(s)
- Medial and lateral canthal tendon integrity
- Culture open wound and any purulence if present
- Do not remove partially embedded objects in an uncontrolled setting without knowledge or visualization of the full length of the object. If necessary, stabilize the object to safely complete imaging in preparation for controlled surgical removal.
- Computed tomography (CT) scan
- Axial, sagittal, and direct coronal views when possible
- Excellent visualization of metal, glass, and stone foreign bodies
- Organic foreign bodies (Figure‰Ûø2)
- Fresh wood
- Increased water content makes it appear hyperintense or isointense to muscle.
- Dry wood
- Hypointense to fat, can look like air particularly if linear in appearance; absorption coefficients can be helpful in differentiating.
- Eventually becomes more hydrated, appearing more intense over time
- Discuss with the radiologist the possibility of an organic foreign body; expand the window width to 1,000 Hounsfield units; fine axial, coronal, and sagittal cuts (Shelsta, OPRS 2010).
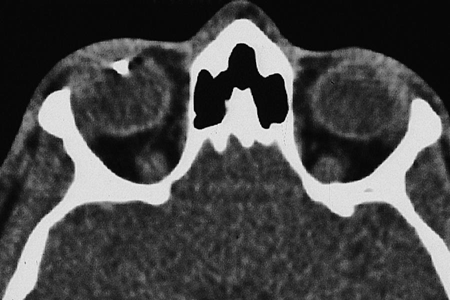
Figure 2. CT scan, organic foreign body.
- Orbital bone defects
- Orbital hemorrhage
- Intracranial injury
- Magnetic resonance imaging (MRI)
- Should never be the initial imaging modality due to concern for possibly metallic foreign body that is easily visualized on CT
- Superior soft tissue resolution can help in identification of some wooden foreign bodies.
- Wood appears hypointense on T1-weighted images; ring enhancement with gadolinium might be seen (Shelsta, OPRS 2010).
- Contraindicated for suspected metallic foreign body
Differential diagnosis
Perforating or penetrating orbit injury without retention of foreign body
Patient management: treatment and follow-up
Natural history
- Anterior location and good initial visual acuity associated with better outcome
- Posterior metallic fragments (bullet or pellets) are typically well tolerated and do not require surgical removal (Ho, OPRS 2004).
- Late presentation with orbital symptoms should alert the clinician to the possibility of a retained foreign body particularly organic foreign bodies.
- Decreased visual acuity is frequently due to associated ocular injury at the time of the initial event (Fulcher, Ophthalmology 2002).
Medical therapy
- Antibiotics
- Consider hospitalization and IV antibiotics for contaminated objects or organic material
- Tetanus immunization
- Foreign bodies deeper in the orbit can often be observed without surgery.
- Metallic and nonmetallic inert foreign bodies usually well tolerated (Callahan, Int Ophthalmol Clin 2013)
- Smooth edges
- For example: BBs, bullet fragments, steel, lead, aluminium, other alloys, glass, ceramics, stone, and plastic
- Exceptions are some copper and iron foreign bodies
- Iron: The concern is for siderosis and slow retinal deterioration with loss of vision.
- Iron foreign bodies in direct contact with the globe have been shown to cause focal retinal atrophy in animal models (Ho, OPRS 2004).
- Most BBs and gunshot pellets are made of 80%–90% lead and only 10%–20% iron.
- Serial ERGs can be done to monitor for the development of retinal degeneration in those foreign bodies with increased adverse surgical risk.
- Copper: The concern is for chalcosis.
- Alloys that are less than 85% copper such as bronze and brass are fairly well tolerated.
- Again serial ERGs can be done to monitor for a decrease in b-wave amplitude with relative preservation of the a-wave (Ho, OPRS 2004).
Surgery
- The following foreign bodies should be surgically removed (Fulcher, Ophthalmology 2002)
- Organic or vegetable foreign bodies
- Contaminated foreign bodies
- Toxic foreign bodies as mentioned above when surgically accessible, when causing orbital symptoms, or visual compromise
- If there is a risk of aerobic or anaerobic infection
- Large foreign bodies with sharp edges
- Foreign bodies compressing the globe
- If located near optic nerve and causing decreased vision or gaze evoked amaurosis
- If penetrating intracranially
- Visible, palpable or superficially located
- Readily accessible metallic foreign bodies to allow for the unforeseen need of future MRI studies
- Endoscopy, ultrasonography, surgical electromagnetic instruments, and intraoperative fluoroscopy can be useful surgical adjuncts (Cho, OPRS 2009 and Fulcher, Ophthalmology 2002 and Close, OPRS 2009).
- If there is fistulization to the skin, the tract can be followed to aid in the location of the foreign body.
- Nasal endoscopic approach for visualization of the sphenoid sinus can be useful if movement of the object might jeopardize the internal carotid artery.
- Foreign bodies should be cultured on removal and submitted to pathology.
- Neurosurgical consultation for all foreign bodies suspected of intracranial and/or cavernous sinus penetration
Preventing and managing treatment complications
- Damage to orbital/ocular structures during surgical manipulation
- Inability to find the foreign body
- Fragmentation of the foreign body with incomplete removal (Nasr, Ophthalmology 1999)
- Postsurgical cicatricial changes to the periorbita resulting in facial asymmetry/disfigurement, lagophthalmos, enophthalmos, dysmotility
Disease-related complications
- Traumatic optic neuropathy
- Globe injury
- Diplopia secondary to extraocular dysmotility
- Orbital hemorrhage
- Orbital compartment syndrome
- Orbital granulomatous inflammation
- Orbital cellulitis
- Panophthalmitis, acute chalcosis or siderosis
- Blepharoptosis
- Fistula formation
- More likely with copper, stone and wood slivers
- Intracranial injury
Patient instructions
- Follow up as instructed
- Complete course of antibiotics
- Report any decrease in vision
References and additional resources
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2010-2011.
- AAO, Focal Points: Management of Orbital Trauma: Fractures, Hemorrhage, and Traumatic Optic Neuropathy. Vol. 12, No. 7, 1994: 8-11.
- Callahan AB, Yoon MK. Intraorbital foreign bodies: retrospective chart review and review of literature. Int Ophthalmol Clin. 2013; 53(4):157-165.
- Cho RI, Kahana A, Patel B, Sivak-Callcott J, Buerger DE, Durairaj VD, Vidor I, Mawn LA. Intraoperative fluoroscopy-guided removal of orbital foreign bodies. Ophthal Plast Reconstr Surg. 2009; 25(3):215-218.
- Close JK, Shiels WE 2nd, Foster JA, Powell DA. Percutaneous ultrasound-guided intraorbital foreign body removal. Ophthal Plast Reconstr Surg. 2009; 25(4):335-337.
- Cooper WC, Haik BG, Brazzo BG. Management of Orbital Foreign Bodies. In: Smith’s Ophthalmic Plastic and Reconstructive Surgery. 2nd Ed. Nesi FA, Levine MR, Lisman RD. St. Louis, MO: Mosby-Year Book, Inc. 1998.
- Finkelstein M, Legmann A, Rubin PAD. Projectile metallic foreign bodies in the orbit: a retrospective study of epidemiologic factors, management, and outcomes. Ophthalmology. 1997; 104:96-103.
- Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology. 2002; 109(3):494-500.
- Ho VH, Wilson MW, Fleming JC, Haik BG. Retained intraorbital metallic foreign bodies. Ophthal Plast Reconstr Surg. 2004; 20(3):232-236.
- McGuckin JF Jr, Akhtar N, Ho VT, Smergel EM, Kubacki EJ, Villafana T. CT and MR evaluation of a wooden foreign body in an in vitro model of the orbit. Am J Neuroradiol. 1996;17:129-133.
- Nasr AM, Haik BG, Fleming JC, Al-Hussain HM, Karcioglu ZA. Penetrating orbital injury with organic foreign bodies. Ophthalmology. 1999; 106(3):523-532.
- Shelsta HN, Bilyk JR, Rubin PA, Penne RB, Carrasco JR. Wooden intraorbital foreign body injuries: clinical characteristics and outcomes of 23 patients. Ophthal Plast Reconstr Surg. 2010; 26(4):238-244.
