Lateral and Medial Canthoplasty
Updated August 2024
Goals, indications, contraindications
Goals
Restore normal anatomic eyelid position
- Correction of involutional lower lid ectropion, entropion, and/or retraction
Maintain anatomic apposition of lid to globe
- Lid laxity causes poor lid-to-globe apposition leading to tear film instability and exposure keratopathy.
Restore normal lid tension
- Tear pump failure can result from excessive lid laxity or facial nerve palsy (Vick, OPRS 2004).
- Floppy eyelid syndrome, eyelid imbrication (see below)
Improve aesthetic appearance of eyelid
- Eyelid contour can be affected by laxity of lateral or medial canthal tendons.
- Rounding of lateral commissure
- Contour abnormality can result from performing lower lid blepharoplasty without addressing lid laxity.
- Lateral canthal dystopia can be involutional, traumatic, or developmental.
- Normal position of lateral commissure slightly higher than medial commissure
- Medial canthal deformities (e.g., telecanthus, dystopia, epicanthal folds) are usually traumatic or congenital.
Indications
Lid malposition due to horizontal laxity
- Involutional ectropion (Bedran, Semin Ophthal 2010) (Figure 1)
- Poor lid-to-globe apposition causing exposure keratopathy
- Punctal ectropion causing epiphora
- Involutional entropion (Pereira, Semin Ophthal 2010) (Figure 2)
- Significant ocular discomfort caused by lashes and keratinized skin rubbing directly on cornea
- Pathophysiology:
- Lower-lid laxity
- Dehiscence of lower lid retractors
- Overriding orbicularis — often exacerbated by irritative symptoms causing blepharospasm (“spastic” entropion)
- Enophthalmos
- Lower-lid retraction (Chang OPRS 2011) (Figure 3)
- Involutional — lid laxity
- Cicatricial — infection, inflammation, trauma, burns, postsurgical (e.g., lower-lid blepharoplasty, laser skin resurfacing)
- Mechanical — midface ptosis, craniofacial anomalies, tumor
- Paralytic — facial nerve palsy

Figure 1. Involutional right lower lid ectropion.
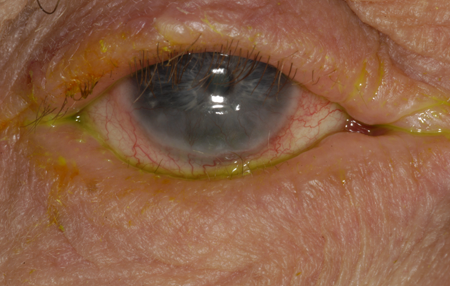
Figure 2. Involutional right lower lid entropion. Note inferior corneal scarring and pannus due to chronic mechanical and exposure keratopathy.

Figure 3. (Left) Mixed mechanism (involutional, paralytic, cicatricial, and mechanical) right lower lid ectropion and retraction in patient with history of right facial nerve palsy and resection/free flap reconstruction of squamous cell carcinoma. (Right) Postoperative photograph following right subperiosteal midface lift and lateral canthopexy with drill hole fixation.
Tear pump failure
(Meyer, Curr Opin Ophthal 1993)
- Involutional and/or paralytic
Medial canthal tendon (MCT) laxity
- Severe laxity, especially in setting of facial nerve paralysis, can cause punctal ectropion, medial lower lid retraction, lagophthalmos/exposure keratopathy, and epiphora (Figure 4).
- Performing lateral canthal tendon (LCT) tightening in presence of MCT laxity can lateralize punctum and cause lacrimal outflow deficiency.
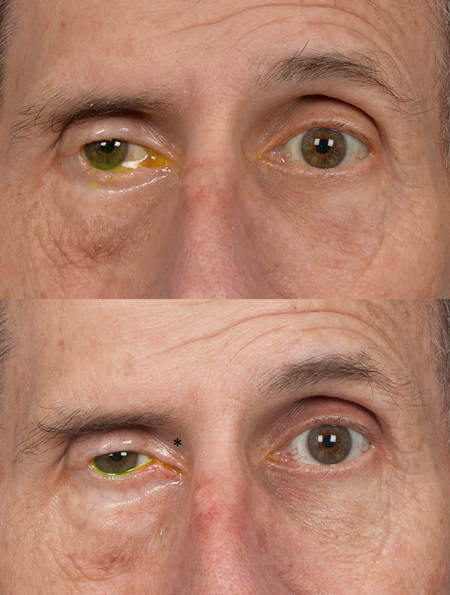
Figure 4. (Top) Medial right lower lid retraction and lagophthalmos in patient with facial nerve palsy. Epiphora and exposure keratopathy persist despite upper lid weight implantation and lateral tarsorrhaphy. (Bottom) Postoperative photograph following transcaruncular medial canthal tendon (MCT) plication with suture fixation to superomedial orbital rim (suture placement indicated by asterisk).
Canthal malposition
- Involutional, developmental, postsurgical, or traumatic
Floppy eyelid syndrome
(Culbertson, AJO 1981; Moscato, Compr Ophthal Update 2007)
- Marked lid laxity associated with softening of tarsus
- Multiple possible factors implicated in pathogenesis:
- Prone or side sleeping position causes mechanical pressure on lids
- Ischemia and reperfusion injury
- Upregulation of matrix metalloproteinases (MMP) implicated in elastin degeneration
- Lids can spontaneously evert during sleep, causing exposure keratopathy and chronic papillary conjunctivitis
- Associated with obstructive sleep apnea and obesity
- Surgical treatment involves upper-eyelid tightening
Eyelid imbrication
(Karesh, Ophthalmology 1993)
- Lid laxity causes upper-lid margin to overlap lower lid
- Upper palpebral conjunctiva rubs across lower lashes, leading to chronic irritation
- Sometimes associated with floppy eyelid syndrome
- Can be addressed with lower- and/or upper-lid tightening
Reconstruction following trauma or surgery
- Traumatic LCT/MCT avulsion
- Must rule out canalicular injury with MCT avulsion
- LCT resuspension following emergent lateral canthotomy and cantholysis for orbital compartment syndrome
- Tumor resection
Mild lower-lid laxity or lateral canthal deformity
- Open or closed lateral canthoplasty often performed in conjunction with various facial rejuvenation procedures (Taban, OPRS 2010) (e.g., upper- and/or lower-lid blepharoplasty, midface lift)
Contraindications
Relative
- Significant medial canthal tendon laxity (see above)
- Proptosis: surgical tightening of lids in presence of proptosis can lead to lid retraction
- Options for amelioration:
- Supraplacement of LCT on orbital rim (McCord 2008)
- Midface lift with possible malar augmentation to improve negative vector between cheek and orbit (Steinsapir, PRS 2003)
- Correction of proptosis (orbital decompression) or lateral rim repositioning (Kikkawa, Ophthalmology 2002)
Absolute
- Presence of malignancy, infection, or other pathology that would compromise surgical result
Preprocedure evaluation
Patient history
HPI
- Inquire about complaints of tearing, ocular discomfort, exposure symptoms.
- Tearing often multifactorial: excessive reflex tearing and deficient lacrimal outflow
Conditions that can cause or exacerbate involutional changes
- Facial nerve paralysis
- Bell’s palsy
- Facial trauma
- Surgery (e.g., vestibular schwannoma resection)
- CNS tumor
- Blepharospasm
- Obstructive sleep apnea (OSA)
- Risk factor for floppy eyelid syndrome (Moscato, Compr Ophthal Update 2007)
- Should be referred for sleep study if OSA suspected due to risk of systemic complications
Conditions that can cause or exacerbate cicatricial abnormalities
- Infection
- Trachoma
- HSV/HZV
- Necrotizing fasciitis
- Inflammation
- Stevens-Johnson syndrome
- Ocular cicatricial pemphigoid (OCP)
- Sarcoidosis
- Sezary syndrome, mycosis fungoides
- Tumors (primary or following resection/reconstruction)
- Basal cell carcinoma
- Squamous cell carcinoma
- Sebaceous carcinoma
- Melanoma
- Trauma
- Periorbital lacerations
- Burns (thermal or chemical)
- Surgery
- Lower-lid blepharoplasty
- Laser skin resurfacing
- Facial/orbital fracture repair
Conditions associated with medial or lateral canthal deformities
- Congenital anomalies (Jones 2013; Fries, Surv Ophthalm 1990)
- Down syndrome
- Craniosynostoses (Crouzon, Apert syndrome etc.)
- Euryblepharon
- Mandibulofacial dysostosis (Treacher-Collins syndrome)
- Oculoariculovertebral dysplasia (Goldenhar syndrome)
- Blepharophimosis syndrome (Figure 5)
- Narrowed horizontal palpebral fissure
- Ptosis
- Epicanthus inversus
- Trauma
- Naso-orbito-ethmoid (NOE) fractures (Markowitz, PRS 1991)
- Zygomaticomaxillary complex (ZMC) fractures
- Under-reduced frontozygomatic fracture (Converse, Clin Plast Surg 1975)
- Failure to resuspend midface following subperiosteal dissection, resulting in midface ptosis and lateral canthal dystopia (Lee 2008) (Figure 6)
- Periocular lacerations

Figure 5. Blepharophimosis syndrome.

Figure 6. Left midface ptosis and lateral canthal dystopia following open repair of zygomaticomaxillary complex and orbital floor fractures.
Clinical examination
Lid laxity
- Snap-back test, lid distraction
- MCT laxity: Distract lid laterally and observe punctal position
- Laxity significant if punctum moves close to or beyond nasal limbus
- Floppy eyelids
- Easily evertable upper lids
- Papillary conjunctivitis
- Eyelid imbrication: upper lid overlaps lower with lid closure
Lid malposition
- Ectropion, entropion, or retraction
- Punctal ectropion or override (“kissing puncta”)
Lagophthalmos
Retractor disinsertion
- Associated with involutional entropion and severe involutional ectropion
- With lower lid eversion, edge of disinserted retractor can be visualized subconjunctivally as a transition from white to pink below the inferior border of the tarsus
Lamellar shortening
- Scarring or shortening of anterior or posterior lamella can cause ectropion or entropion, respectively
- Scarring of the orbital septum (middle lamella) can cause tethering of the lid to the orbital rim
Midface ptosis and/or hypoplasia
- Downward traction exerted by cheek on lower lid can exacerbate retraction and ectropion
- Malar hypoplasia (developmental or age-related) can create negative vector of forces apposing lid to globe
Signs of corneal exposure
- Epithelial erosions/defects, scarring, etc.
Lacrimal outflow evaluation as indicated
- Primary dye test or dye disappearance test
- Canalicular probing and irrigation
Proptosis or enophthalmos
Preoperative assessment
Treatment must be individualized to each patient.
Involutional ectropion
- Distract lid laterally to estimate effect of tightening on lid position
- Consider medial spindle in addition to lower lid tightening if punctal ectropion persists (Nowinski, Arch Ophthalmol 1985)
- Evaluate for possible retractor dehiscence
Involutional entropion
- Repair typically involves lower lid tightening, retractor reinsertion, and excision of overriding orbicularis (if external approach used)
- Retractors can be approached transconjunctivally (Erb, Ophthalmology 2006) or externally through subciliary incision
Lower-lid retraction
- Critical to distinguish involutional from cicatricial, mechanical, and paralytic causes
- Depending on underlying pathology, may need to consider adjunctive procedures in addition to lid repositioning:
- Midface ptosis—midface lift
- Midface hypoplasia—malar augmentation
- Cicatricial entropion or thyroid orbitopathy—posterior lamellar spacer graft
- Anterior lamellar scarring—full thickness skin graft
- Scarring of orbital septum—dermis fat graft spacer Chang
Medial canthal tendon laxity
- MCT plication can be performed alone or concurrently with lateral canthoplasty
- Anterior crus can be plicated transcutaneously (Sodhi, J Cranio-Maxillofacial Surg 2005)
- Might not improve globe apposition
- Posterior plication can be performed through transcaruncular approach (Fante, OPRS 2001)
- Theoretical advantage in correcting globe apposition due to posterior vector
Lateral canthal dystopia
- Usually correctable with standard LCT suspension from lateral orbital wall, with or without lower lid tightening
- In recurrent or complex cases (e.g., cicatricial retraction, midface reconstruction), lateral canthopexy may be considered by securing with sutures or wires to:
- Drill holes in lateral rim
- Titanium screws
- Bone anchors (e.g., Mitek, Lactosorb syndrome etc.)
Medial canthal dystopia
- Usually post-traumatic or developmental
- Can be addressed with medial canthopexy or Z-plasty reconstruction
Telecanthus
- Usually traumatic or congenital
- Normal intercanthal distance approximately equal to horizontal palpebral fissure length
- Must determine whether abnormality is purely soft tissue, or if underlying bony deformity is present (i.e., telorbitism or hypertelorism)
- Repair technique largely depends upon this anatomic distinction
Epicanthal folds
- Numerous options involving advancement or transposition flaps
- Must determine whether attachment of MCT is in proper anatomic position; medial canthopexy may be required if not
Procedure alternatives
Nonsurgical
- Observation
- Ocular lubrication
- Corneal protection, e.g. for burns (Malhotra Surv Ophth 2009), severe cicatrization
- Moisture chambers
- PROSE lens (Kalwerisky, Ophthalmology 2012)
- Amniotic membrane (ProKera) (Pachigolia, Eye Contact Lens 2009)
- Horizontal lid taping (involutional entropion)
Surgical
- Lagophthalmos
- Tarsorrhaphy (McInnes, AJO 2006) (suture or permanent)
- Lid weight implantation (Mavrikakis OPRS 2006)
- Upper-lid recession (Ben Simon, AJO 2005)
- Full-thickness blepharotomy (Demirci OPRS 2007)
- Involutional entropion
- Quickert sutures (Quickert, Arch Ophth 1971)
- Lid tightening
- Full-thickness wedge resection (Callahan 1956) (largely historical)
Surgical techniques
Horizontal lower lid tightening
Lateral tarsal strip procedure
(Anderson Arch Ophth 1979) (Figure 7)
- Infiltrate local anesthetic
- Perform lateral canthotomy and inferior cantholysis
- Determine amount of horizontal laxity
- Place lateral traction on lid and mark point where lid crosses lateral rim and commissure
- Create tarsal strip
- Dissect anterior lamella and excise to point where lid crosses lateral commissure
- Excise marginal epithelium
- Detach retractors/conjunctiva from inferior edge
- Remove palpebral conjunctiva with blade, low energy cautery, or radiofrequency ablation
- Trim tarsal strip to point where lid crosses orbital rim
- Suspend strip from periosteum over inner aspect of rim
- 4-0 or 5-0 absorbable or nonabsorbable suture (e.g., polyglactin, polydiaxanone, or polypropylene) on a small half-circle needle (P-2 or OPS-5)
- Horizontal mattress or half-horizontal mattress pattern, ensuring positioning of strim posterior to lateral rim
- Slight overcorrection advisable (about 2–3 mm superior to intended final position of lateral commissure)
- Reform lateral canthal angle (Weber, Ophth Surg 1991)
- Trim redundant skin
- Close skin
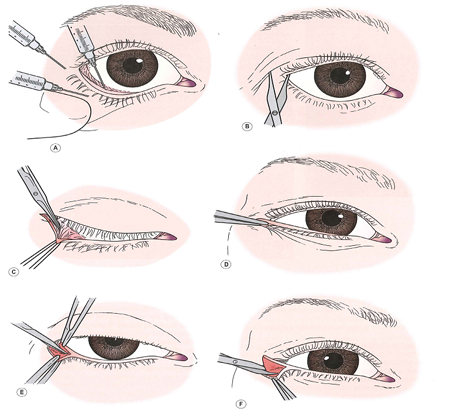
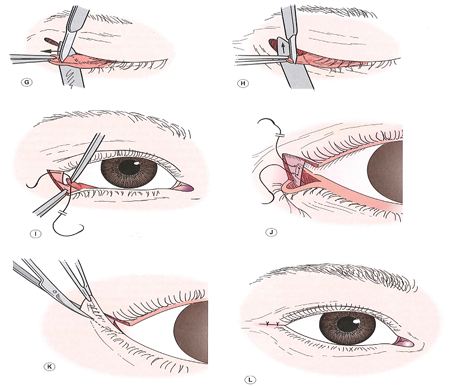
Figure 7. Lateral tarsal strip procedure. From Nerad JA, Techniques in Ophthalmic Plastic Surgery, 2010.
Modified Bick procedure
(Barrett, OPRS 2012)
- Lateral canthotomy/inferior cantholysis
- Distract lid laterally and mark point where lid crosses lateral rim
- Excise triangular wedge of lateral canthal tendon and tarsus
- Suspend end of tarsus to periosteum as above
- Reform lateral canthal angle
- Close skin
Closed lateral canthoplasty
(Taban, Georgescu, Rizvi, Lessa) (Figure 8)
- Carry dissection to lateral orbital rim through lateral upper lid crease incision.
- Pass suture internal to external through lateral commissure, then back internally at same point.
- Pass suture through periosteum behind lateral orbital rim and tie.
- Suture can also be passed through drill holes in lateral rim using “Leicester lasso” technique (Kannan OPRS 2014).
- 4-0 silk suture twisted into lasso and passed external to internal through drill holes x2
- LCT suture ends passed through lasso, pulled through drill holes with lasso, and tied

Figure 8. Closed lateral canthoplasty through lateral upper lid crease incision. From Taban M, et al. Ophthal Plast Reconstr Surg. 2010;26:190-194.
Reinforcement lateral canthoplasty — for complex or recurrent LCT laxity/dehiscence
(Dailey OPRS 2011)
- Superior and inferior crus of LCT approached through supraciliary/subciliary incisions
- LCT plicated and suspended from periosteum behind lateral orbital rim
- Y-shaped graft (e.g., autogenous fascia lata, acellular dermal matix, porcine dermal collagen) sutured to limbs of LCT and periosteum over lateral rim
Adjunctive procedures
- Medial spindle procedure (Nowinski, Arch Ophthalmol 1985)
- Excision of diamond-shaped wedge of conjunctiva/retractors inferior to lower punctum
- Double-armed absorbable suture (e.g., 6-0 polyglactin or chromic gut) passed from inferior to superior wound edges, then through inferior fornix and externalized, tied over skin
- Orbitomalar ligament suspension (Korn PRS 2010)
- Dissection carried from lateral canthotomy through orbitomalar ligament under lateral midface, suture passed through deep aspect of SOOF and suspended from lateral orbital rim periosteum
- Alternative fixation technique: LCT suture passed through single drill hole in lateral rim and tied externally to SOOF suture (Oh, OPRS 2013)
- Midface lift
- Preperiosteal (Marshak OPRS 2010) or subperiosteal (Elner, Arch Fac Plast Surg 2003) dissection
- Consider malar augmentation for midface hypoplasia (Steinsapir, PRS 2003; Binder, Fac Plast Surg 2011).
- Midface tissues suspended and fixated with sutures to drill holes, screws, malar implants, or elevated with fixation devices (e.g., Endotine™ midface (Berkowitz, Aesth Surg J 2005)
Upper-lid tightening
- Full-thickness wedge resection (traditional)
- Lateral tarsal strip procedure or modified Bick procedure can be performed on upper lid in similar manner as lower lid (Dutton, AJO 1985; Perlman, OPRS 2002)
- 4-lid lateral tarsal strip-periosteal flap technique (Burkat, OPRS 2005)
- 5-mm lateral canthus incision to expose lateral rim
- 6-mm periosteal flap created and reflected medially
- Lateral tarsal strips fashioned in standard fashion and fixated to periosteal flaps with 5-0 polyglactin suture
Medial canthoplasty
Anterior medial canthal tendon plication
(Sodhi 2005)
- Create skin incisions (single horizontal or double vertical) over anterior crus of MCT and medial end of tarsus
- Pass suture sequentially through MCT near bony insertion, subcutaneous tunnel, and medial end of tarsus, taking care to avoid canaliculus (placement of lacrimal probe helpful)
- Tie under appropriate tension
- Close skin incisions(s)
Transcaruncular (posterior) medial canthal tendon plication
(Fante OPRS 2001) (Figure 9)
- Incise conjunctiva below medial end of lower tarsus
- Create transcaruncular incision between caruncle and plica semilunaris, dissect bluntly to medial orbital wall
- Engage medial end of tarsus with suture (4-0 polypropylene on P-2 needle), avoiding canaliculus, and pass suture subconjunctivally to transcaruncular incision
- Pass same suture through periosteum at or above posterior lacrimal crest, then back through subconjunctival space to exit incision beneath tarsus
- If medial lower lid retraction is present, suture can be fixated more superiorly on medial rim Moe
- Adjust suture tension and tie
- Rotate knot to bury it in medial orbit
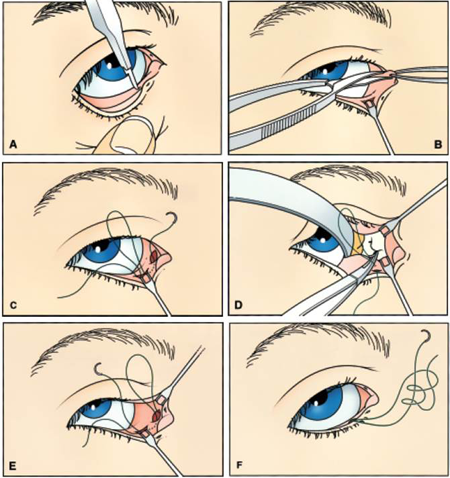
Figure 9. Transcaruncular medial canthal tendon plication. From Fante RG, Elner VM. Ophthal Plast Reconstr Surg. 2001:17;16-27. (A) Horizontal conjunctival incision is made at the base of the medial tarsus. (B) A second conjunctival incision is made in the medial fornix just posterior to the caruncle. Blunt dissection proceeds to the medial periorbita. (C) The medial end of the tarsus is engaged by 4-0 polypropylene suture, which is then passed subconjunctivally from the lower-eyelid incision to the medial fornix incision. (D) Periorbita at or above the posterior lacrimal crest is secured with the suture under direct headlamp observation while an assistant provides exposure. (E) The needle is passed subconjunctivally from the medial fornix incision to the lower eyelid incision. At this point, both ends of the suture exit from the lower-eyelid incision. (F) A fisherman’s knot is tied to achieve appropriate tension. Once permanently tied, the ends are cut and the knot is rotated into the medial orbit.
Medial tarsal suspension — for medial lower lid retraction
(Frueh OPRS 2002)
- Create horizontal skin incisions from medial commissure to within 2 mm medial to each punctum (Figure 10).
- Dissect pockets in suborbicularis plane medial to lower punctum (avoiding canaliculi) and in superomedial upper lid.
- Pass suture (5-0 or 4-0 nonabsorbable) through periosteum over superomedial rim.
- Pass same suture through medial end of lower tarsus and tie under appropriate tension, rotate knot to bury next to superomedial rim.
- Sew edges of upper and lower lid skin incisions together (medial tarsorrhaphy).
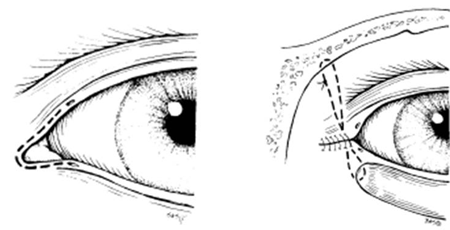
Figure 10. Medial tarsal suspension. From Frueh BR, Su CS. Ophthal Plast Reconstr Surg. 2002:18;133-137.
Repair of epicanthal folds
- Create canthoplasty incisions
- Mustarde “stick man” (Anderson, Arch Ophth 1989) (Figure 11A)
- 5-flap technique (Figure 11C)
- Skin redraping method (Sa, Ophthalmology 2012)
- Undermine and transpose myocutaneous flaps, excise excess soft tissue
- Close skin and soft tissues
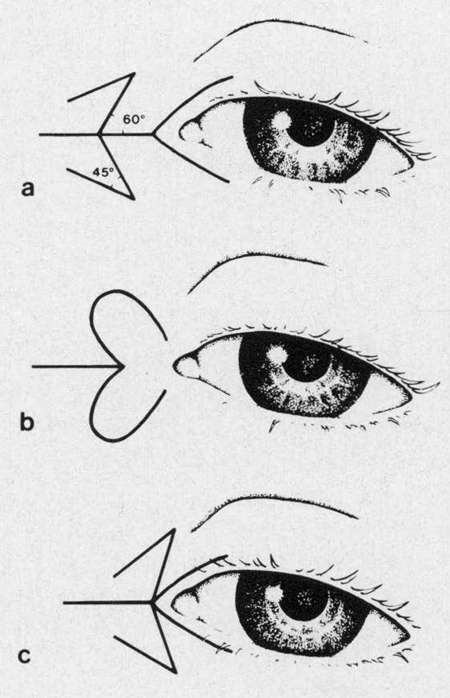
Figure 11. (A) Mustarde medial canthoplasty. (B) Johnson modification of Blair technique (historical). (C) Anderson 5-flap technique (double Z-plasty and V-to-Y advancement). From Anderson RL, Nowinski TS. Arch Ophthalmol. 1989;107:448-452.
Medial canthal z-plasty — for MC dystopia
(Fox 1976)
- Create z-plasty incision, incorporating anterior crus of MCT into lower limb of Z (Figure 12).
- Dissect MCT from lacrimal sac, undermine flaps
- Transpose flaps and resuspend MCT in higher position with suture to periosteum over frontal process of maxilla
- Close incisions

Figure 12. (A) Traumatic right medial canthal dystopia with planned Z-plasty incisions. (B) Postoperative result following medial canthus Z-plasty.
Medial canthopexy
Congenital hypertelorism
- Bony reconstruction required, multidisciplinary craniofacial team approach recommended
Primary repair of NOE fracture
- See Orbital Fractures.
Transnasal wiring
(Smith 1992; Dutton, AJO 1985)
- Bilateral telecanthus (e.g., blepharophimosis (Sebastia, Aesth Plast Surg 2011) bilateral NOE fractures)
- MCTs are wired to each other through drill holes across the nasal cavity
- Wire can aid in reduction/fixation of bony abnormalities, or in setting of normal bony anatomy can be passed through drill holes to engage MCT’s and reduce telecanthus
- Surgical approaches include bicoronal, Lynch incision, or incision directly over MCT (Nunery incision) (Timoney, OPRS 2012)
- Unilateral telecanthus (traumatic)
- MCT is wired across the nasal cavity to stable bone (frontal process of maxilla or frontal bone) on the opposite side (Kelly, OPRS 2004; Markowitz, PRS 1991)
- Titanium wire with barb and needle (Synthes®) can be used transnasally or anchored directly to frontal process (Engelstad Int J Oral Maxillofac Surg 2012)
Fixation of MCT to bone anchors
- Titanium microplates/screws (Shore, Ophthalmology 1992; Howard, Arch Ophth 1992)
- Mitek bone anchor (Antonyshyn, PRS 1996; Goldenberg, Ann Plast Surg 2008)
- Lactosorb anchor (Sharma, Arch Ophth 2006)
Patient management: treatment and follow-up
Counsel patient that lids will be tight initially and will slowly relax over time.
If nonabsorbable skin sutures used, remove 5–7 days postoperatively.
Monitor for appropriate anatomic changes and functional/aesthetic response to treatment.
Postoperative instructions
- Appropriate activity limitations
- Keep wounds clean and dry
- Monitor for signs of infection
Medications
- Antibiotic ointment to incisions
- Pain medications as needed
Preventing and managing treatment complications
- Failure to correct underlying pathology
- Suture failure with canthal dehiscence
- Multiple sutures can be placed primarily to prevent
- Suture granulomas
- Treatment: excision, steroid injection
- Lateralization of punctum
- Caused by unrecognized/unaddressed medial canthal tendon laxity
- Lid retraction
- Can occur in setting of proptosis or aggressive lower lid blepharoplasty
- Diplopia
- Due to scarring of conjunctiva or lateral rectus tendon sheath
Disease-related complications
- Uncommon, usually associated with involutional changes
- Facial nerve palsy
- Exposure keratopathy
- Epiphora
- Brow ptosis
- Floppy eyelid syndrome: associated with obstructive sleep apnea
Historical perspective
Repair of involutional lower lid ectropion
- Traditional surgery involved full-thickness wedge resection
- Kuhnt-Szymanowski procedure (Callahan 1966) (Figure 13)
- Bick procedure (Bick, AJO 1963)
- Lateral tarsal strip procedure described by Anderson in 1979 (Anderson, Arch Ophth 1979)
- Many modifications of tarsal strip now utilized
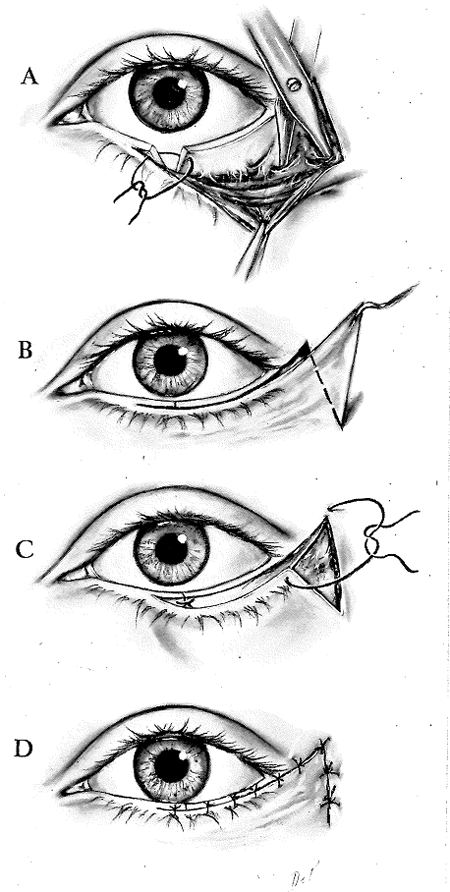
Figure 13. Kuhnt-Szymanowski procedure. From Callahan A. Reconstructive Surgery of the Eyelids and Ocular Adnexa, 1966.
Repair of involutional lower lid entropion
- Most early repair techniques focused on retractors and/or orbicularis
- Jones, Reeh, and Tsukimura (Jones 2013)
- Quickert sutures
- Full-thickness wedge resection advocated by Hill, Quickert
- Lateral tarsal strip introduced and has become standard component of entropion repair Rose
References and additional resources
- Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979:97;2192.
- Anderson RL, Nowinski TS. The five-flap technique for blepharophimosis. Arch Ophthalmol. 1989;107:448-52.
- Antonyshyn OM, Weinberg MJ, Dagum AB. Use of a new anchoring device for tendon reinsertion in medial canthopexy. Plast Reconstr Surg 1996;98:520-23.
- Barrett RV, Meyer DR. The modified Bick quick strip for surgical treatment of eyelid malposition. Ophthal Plast Reconstr Surg 2012;28:294-9.
- Bedran EG, Periera MV, Bernardes TF. Ectropion. Semin Ophthalmol 2010;25:59-65.
- Ben Simon GJ, Mansury AM, Schwarcz RM, et al. Transconjunctival Müller muscle recession with levator disinsertion for correction of eyelid retraction associated with thyroid-related orbitopathy. Am J Ophthalmol 2005;140:94-99.
- Berkowitz RL, Apfelberg DB, Simeon S. Midface lift technique with use of a biodegradable device for tissue elevation and fixation. Aesthet Surg J 2005;25:376-82.
- Bick MW. Orbital tarsal disparity. Arch Ophthalmol 1966;75:386.
- Jones LT, Reeh MJ, Tsukimura JK. Senile entropion. Am J Ophthalmol. 1963;55:463-9.
- Binder WJ. Facial rejuvenation and volumization using implants. Facial Plast Surg 2011;27:86-97.
- Burkat CN, Lemke BN. Acquired lax eyelid syndrome: an unrecognized cause of chronic ocular irritation. Ophthal Plast Reconstr Surg 2005;21:52-8.
- Callahan A. Reconstructive Surgery of the Eyelids and Ocular Adnexa. Birmingham, Alabama: Aesculapius Publishing Co., 1966: 120-157.
- Chang EL, Rubin PA. Upper and lower eyelid retraction. Int Ophthalmol Clin 2002;42:45-59.
- Chang HS, Lee D, Taban M, Douglas RS, Goldberg RA. “En-glove” lysis of lower eyelid retractors with AlloDerm and dermis-fat grafts in lower eyelid retraction surgery. Ophthal Plast Reconstr Surg 2011;27:137-41.
- Converse JM, Smith B, Wood-Smith D. Deformities of the midface resulting from malunited orbital and naso-orbital fractures. Clin Plast Surg 1975;2:107-203.
- Culbertson WW, Ostler HB. The floppy eyelid syndrome. Am J Ophthalmol 1981;92:568-75.
- Dailey RA, Chavez MR. Lateral canthoplasty with acellular cadaveric dermal matrix graft (AlloDerm) reinforcement. Ophthal Plast Reconstr Surg 2011:28;e29-31.
- Danks JJ, Rose GE. Involutional lower lid entropion: to shorten or not to shorten? Ophthalmology. 1998;105:2065-7.
- Demirci H, Hassan AS, Reck SD, et al. Graded full-thickness anterior blepharotomy for correction of upper eyelid retraction not associated with thyroid eye disease. Ophthal Plast Reconstr Surg 2007;32:36-45.
- Dutton JJ. Surgical management of floppy eyelid syndrome. Am J Ophthalmol. 1985:99:557.
- Elner VM, Mauffray RO, Fante RG, et al. Comprehensive midface elevation for ocular complications of facial nerve palsy. Arch Facial Plast Surg 2003;5:427-33.
- Engelstad ME, Bastodkar P, Markiewicz MR. Medial canthopexy using transcaruncular barb and miniplate: technique and cadaver study. Int J Oral Maxillofac Surg 2012;41:1176-85.
- Erb MH, Uzcategui N, Dresner SC. Efficacy and complications of the transconjunctival entropion repair for lower eyelid involutional entropion. Ophthalmology 2006;113:2351-6.
- Fante RG, Elner VM. Transcaruncular approach to medial canthal tendon plication for lower eyelid laxity. Ophthal Plast Reconstr Surg. 2001:17;16-27.
- Fries PD, Katowitz JA. Congenital craniofacial anomalies of ophthalmic importance. Surv Ophthalmol 1990;35:87-119.
- Frueh BR, Su CS. Medial tarsal suspension. Ophthal Plast Reconstr Surg. 2002:18;133-7.
- Fox SA. Ophthalmic Plastic Surgery, 5th Ed. New York: Grune & Strattonm 1976:210-12.
- Georgescu D. Anderson RL, McCann JD. Lateral canthal resuspension sine canthotomy. Ophthal Plast Reconstr Surg. 2011:27;371-5.
- Goldenberg DC, Bastos EO, Alonso N, et al. The role of micro-anchor devices in medial canthopexy. Ann Plast Surg 2008;61:47-51.
- Howard GR, Nerad JA, Kersten RC. Medial canthoplasty with microplate fixation. Arch Ophthalmol 1992;110:1793-7.
- Jones JL, Jones MC, Del Campo M. Smith’s Recognizable Patterns of Human Malformation, 7th Ed. Philadelphia: Saunders, 2013.
- Kalwerisky K, Davies B, Mihora L, et al. Use of the Boston Ocular Surface Prosthesis in the management of severe periorbital thermal injuries: a case series of 10 patients. Ophthalmology 2012;199:516-21.
- Kannan RY, Chuah JL, Burns J, Sampath RG. The “Leicester Lasso” lateral canthoplasty. Ophthal Plast Reconstr Surg. 2014:30;186.
- Karesh JW, Nirankari VS, Hameroff SB. Eyelid imbrication. Ophthalmology 1993;100:883-9.
- Kelly CP, Cohen AJ, Yavuzer R, Moreira-Gonzalez A. Medial canthopexy: a proven technique. Ophthal Plast Reconstr Surg 2004:20;337-41.
- Kikkawa OD, Pornpanich K, Cruz RC, et al. Graded orbital decompression based on severity of proptosis. Ophthalmology 2002;109:1219-24.
- Korn BS, Kikkawa DO, Cohen SR. Transcutaneous lower eyelid blepharoplasty with orbitomalar suspension: retrospective review of 212 consecutive cases. Plast Reconstr Surg 2010;125:315-23.
- Lee EI, Mohan K, Koshy JC, Hollier LH. Optimizing the surgical management of zygomaticomaxillary complex fractures. Semin Plast Surg 2010;24:389-97.
- McCord CD, Codner MA. Eyelid and Periorbital Surgery. St. Louis: Quality Medical Publishing, 2008:236-242.
- Lessa S, Nanci M. Simple canthopexy used in transconjunctival blepharoplasty. Ophthal Plast Reconstr Surg. 2009:25;284-88.
- Malhotra R, Sheikh I, Dheansa B. The management of eyelid burns. Surv Ophthalmol 2009;54:356-71.
- Markowitz BL, Manson PN, Sargent L, et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: the importance of the central fragment in classification and treatment. Plast Reconstr Surg. 1991:87;843-53.
- Marshak H, Morrow DM, Dresner SC. Small incision preperiosteal midface lift for correction of lower eyelid retraction. Ophthal Plast Reconstr Surg 2010;26:176-81.
- Mavrikakis I, Malhotra R. Techniques for upper eyelid loading. Ophthal Plast Reconstr Surg 2006;22:325-30.
- McInnes AW, Burroughs JR, Anderson RL, et al. Temporary suture tarsorrhaphy. Am J Ophthalmol 2006;142:344-6.
- McCord CD, Codner MA. Eyelid and Periorbital Surgery. St. Louis: Quality Medical Publishing, 2008:236-242.
- Meyer DR. Lacrimal disease and surgery. Curr Opin Ophthalmol 1993;4:86-94.
- Moe KS, Kao CH. Precaruncular medial canthopexy. Arch Facial Plast Surg 2005;7:244-50.
- Moscato EE, Jian-Amadi A. Floppy eyelid syndrome. Compr Ophthalmol Update 2007;8:59-65.
- Mustarde JC. Epicanthal folds and problems of telecanthus. Trans Ophthalmol Soc UK. 1963;83:397-411.
- Nowinski TS, Anderson RL. The medial spindle procedure for involutional medial ectropion. Arch Ophthalmol 1985;103:1750-3.
- Oh SR, Korn BS, Kikkawa DO. Orbitomalar suspension with combined single drill hole canthoplasty. Ophthal Plast Reconstr Surg. 2013:29;357-60.
- Pachigolla G, Prasher P, DiPascuale MA, et al. Evaluation of the role of ProKera in the management of ocular surface and orbital disorders. Eye Contact Lens 2009;35:172-5.
- Pereira MG, Rodrigues MA, Rodrigues SA. Eyelid entropion. Semin Ophthalmol 2010;25:52-8.
- Periman LM, Sires BS. Floppy eyelid syndrome: a modified surgical technique. Ophthal Plast Reconstr Surg 2002;18:370-2.
- Quickert MH, Rathbun E. Suture repair of entropion. Arch Ophthalmol. 1971:85;304.
- Rizvi R, Lypka M, Gaon M, et al. Minimally invasive lateral canthopexy (MILC). J Plast Reconstr Aesthet Surg. 2010;63:1434-6.
- Sa HS, Lee JH, Woo KI, Kim YD. A new method of medial epicanthoplasty for patients with blepharophimosis-ptosis-epicanthus inversus syndrome. Ophthalmology. 2012;119:2402-7.
- Sebastia R, Neto GH, Fallico E, et al. A one-stage correction of the blepharophimosis syndrome using a standard combination of surgical techniques. Aesth Plast Surg 2011;35:820-7.
- Seiff SR, Chang JS Jr. The staged management of ophthalmic complications of facial nerve palsy. Ophthal Plast Reconstr Surg 1993;9:241-9.
- Sharma V, Nemet A, Ghabrial F, et al. A technique for medial canthal fixation using resorbable poly-l-lactic acid-polyglycolic adic fixation kit. Arch Ophthalmol 2006;124:1171-4.
- Shore JW, Rubin PAD, Bilyk JR. Repair of telecanthus by anterior fixation of cantilevered miniplates. Ophthalmology 1992;99:1133-8.
- Sodhi PK, Verma L, Pandey RM, Ratan SK. Appraisal of a modified medial canthal plication for treating laxity of the medial lower eyelid. J Cranio-Maxillofacial Surg 2005;33:205-9.
- Smith B, Beyer C. Medial canthoplasty. Arch Ophthalmol 1969;82:344-8.
- Dutton JJ. Atlas of Ophthalmic Surgery, Volume II: Oculoplastic, Lacrimal, and Orbital Surgery, 1st Ed. Saint Louis: Mosby-Year Book, 1992:214-5.
- Steinsapir KD. Aesthetic and reconstructive midface lifting with hand-carved, expanded polytetrafluoroethylene orbital rim implants. Plast Reconstr Surg 2003;111:1727-37.
- Taban M, Nakra T, Hwang C, et al. Aesthetic lateral canthoplasty. Ophthal Plast Reconstr Surg 2010;26:190-4.
- Timoney PJ, Sokol JA, Hauck MJ, Lee HB, Nunery WR. Transcutaneous medial canthal tendon incision to the medial orbit. Ophthal Plast Reconstr Surg 2012;28:140-4.
- Vick VL, Holds JB, Massry GG. Tarsal strip procedure for the correction of tearing. Ophthal Plast Reconstr Surg 2004;20:37-9.
- Weber PJ, Popp JC, Wulc AE. Refinements of the tarsal strip procedure. Ophthalmic Surg. 1991;22:687-91.
