Lower Eyelid Blepharoplasty
Updated January 2025
Anatomy
Skin
- Fitzpatrick skin types
- I pale white; always burns, never tans
- II fair; usually burns, tans minimally
- III darker white; sometimes mild burn, tans uniformly
- IV light brown; burns minimally, tans easily
- V brown; rarely burns, tans darkly
- VI dark brown to black; never burns, always tans
- True dermatochalasis versus rhytids (static or dynamic)
- Active orbicularis oculi contraction is required to distinguish.
- Dynamic rhytids are more amenable to neurotoxin injections.
- Festoons
- Typically develops between potential space between the orbitomalar ligament and the zygomatic cutaneous ligament
- True festoon or interstitial edema
Orbicularis
- Hypertrophic pretarsal orbicularis
- Occurs in pretarsal region
- Common in Asian patients
Orbital fat
- Clinically apparent fat compartments
- Medial
- Central (divided from medial by inferior oblique)
- Lateral (divided from central by arcuate expansion of inferior oblique
Bone
- Infraorbital rim projection
- Negative vector with anterior globe projection
- Patients with negative are at higher risk for lid retraction following lower lid blepharoplasty.
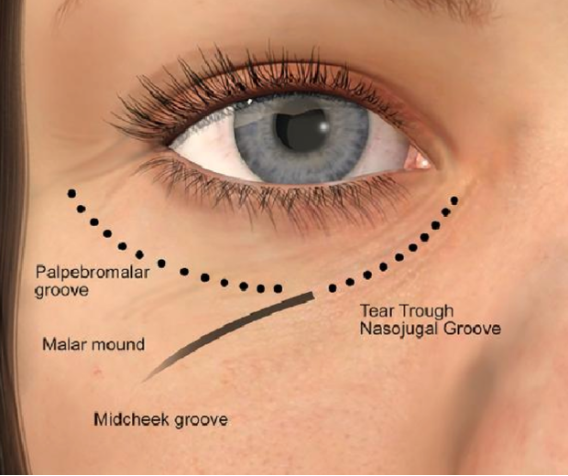
- Malar and nasojugal fold
- Tear trough develops inferomedially due to unmasking of inferior orbital rim
- Contributing factors include genetics, the aging process, and soft tissue deflation.
Ligamentous structures
- Tarsoligamentous band
- Midfacial supporting ligaments
- Orbitomalar ligament
- Zygomatic cutaneous ligament
- Masseteric ligament
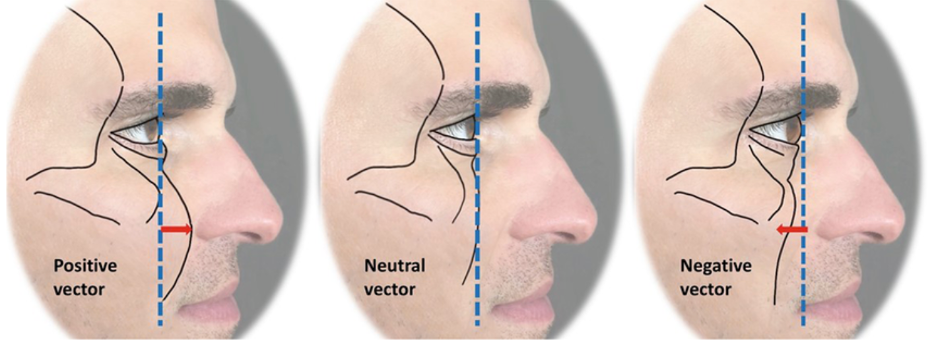
Figure 1. Positive, Neutral, and Negative vectors. A vertical line is drawn from the center of the pupil to the infraorbital rim. Patients with a positive vector have anterior projection of the rim whereas those with a negative vector have anterior projection of the globe compared to the rim.
Patient evaluation
Subjective complaints by patient
- Careful understanding of concerns: Review with mirror.
- Set realistic expectations.
Clinical examination
- Assess subtleties of each anatomic region
- Orbital fat protrusion beyond inferior orbital rim and pseudoherniation of fat pads
- Dermatochalasis, skin tone and festoons
- Tear trough and inferior orbital rim unmasking
- Malar and midface fat deflation
- Relationship of inferior orbital rim (vector)
- Lid position: pre-existing lid retraction
- Lid laxity (snap back and forward traction test)
- “Long eyelid” — lengthening of the distance of the lid margin to the malar fold (cutaneous insertion of the orbitomalar ligament — this indicates some midfacial descent.
Decision-making
- Choice of operation depends on goals and patient’s anatomy.
- The surgeon must be familiar and clinically adept at performing multiple lower lid procedures: one operation cannot accomplish all clinical objectives.
- Clinical experience will help to guide the surgeon with the proper operation.
- For patients with fat protrusion and minimal infraorbital hollowing, consider transconjunctival blepharoplasty; skin pinch or laser resurfacing can be performed as an adjunct to address skin laxity and/or mild dermatochalasis.
- For patients with fat protrusion and moderate infraorbital hollowing, consider transconjunctival fat redraping; skin pinch or laser resurfacing can be performed as an adjunct if necessary to address skin laxity and/or mild dermatochalasis
- For patients with descent, fat protrusion, and infraorbital hollowing, consider transcutaneous fat redraping with orbitomalar suspension; conservative skin removal can be performed with adjunct lid tightening, if necessary, with canthopexy or canthoplasty.
- Additional concomitant or sequential procedures such as autologous fat grafting, midface lift, filler injections, or orbital rim implants might be appropriate.
Preoperative considerations, informed consent
- Thorough medical history and physical with documentation of cardiac, renal, thyroid, pulmonary and autoimmune disease.
- Preoperative medical testing is guided by the age of the patient and medical condition; medical clearance should be obtained if indicated.
- If possible avoid anticoagulants for 7–10 days prior to surgery.
- Avoid smoking
- Informed consent
- Risks: Hemorrhage, infection, scarring, dry eyes, need for possible revision, vision loss
- Benefit: improved cosmetic appearance
- Alternatives: nonsurgical approaches, observation
Techniques
Transconjunctival blepharoplasty
- Incision through conjunctiva and lower lid retractors several millimeters beneath inferior tarsal border
- Preseptal or postseptal dissection
- Conservative fat removal in clinically distinct areas of medial, central and lateral orbital anatomic regions.
- Take care to avoid inferior oblique.
- Keep remaining fat level with inferior orbital rim.
- Residual lateral orbital fat is common complication.
- Hemostasis is important.
- Reinsertion of conjunctiva and lid retractors: optional
- Adjunct lid tightening, canthopexy if necessary
- Adjunct treatment of skin if necessary: laser resurfacing, skin pinch, or chemical peel
Fat redraping
- Transcutaneous or transconjunctival incision
- Preseptal or postseptal dissection
- Fat placement below inferior orbital rim
- Preperiosteal or subperiosteal; avoid infraorbital nerve.
- Preserve fat pedicles; many ways of fixing of orbital fat have been described:
- direct suturing with 5-0 polyglactin suture
- externalized pull out sutures
- subperiosteal placement
- tissue adhesives, “curtain of fat”
Transcutaneous blepharoplasty with orbitomalar suspension
- Infraciliary incision 1 mm below lash line
- Both skin-only versus skin-muscle dissection have been described.
- Increased risks with skin muscle dissection include possible denervation of orbicularis
- Opening of orbital septum with resection or redraping of fat
- Lifting component and vertical support created by orbitomalar suspension
- Release of orbitomalar ligament is performed with sharp and blunt dissection, inferior to orbital rim in the preperiosteal plane.
- Ensure release of lateral component.
- Suspension of cheek tissues to the lateral orbital rim can be performed through a lower lid incision or upper lid crease incision.
- Adjunct lower lid tightening:
- Canthopexy versus canthoplasty depending or pre-exiting laxity
- Consider precautionary lid tightening to lessen risk of postoperative lid retraction.
- Conservative skin excision with skin closure with 6-0 suture.
Festoon management
- True festoon versus interstitial edema
- Options
- Direct excision
- Laser resurfacing
- CO2
- erbium:YAG
- ablative versus nonablative
- Extended blepharoplasty with orbitomalar suspension
- Midface lift
Postoperative care
- Iced compresses
- Antibiotic steroid ointment
- Head elevation
- Avoid heavy exertion, lifting, bending
Complications
Vision threatening complications
- Retrobulbar hemorrhage with vision loss; risk < 1:20,000
- Ruptured globe from anesthetic injection or direct globe injury
Adnexal involvement
- Extraocular muscle damage or incarceration of inferior rectus or inferior oblique during redraping procedure
- Ciliary ganglion damage
- Lacrimal system injury
- Chemosis
- Inflammatory chemosis is more common in the early postoperative period and responds to anti-inflammatory topical medication.
- Lingering interstitial chemosis can result from lymphatic disruption or lid retraction. The latter results from a loss of squeegee effect from lid distraction and might require revisional surgery or direct excision.
Lid malposition
- Lower lid retraction
- Middle lamellar shortening
- Lower lid ectropion
- Anterior lamellar shortening
- Lower lid entropion
- Posterior lamellar shortening
- Canthal dystopia
- Canthal rounding
Undercorrected or overzealous fat resection
- If undercorrected, revision can be performed with excision of residual fat.
- For overcorrection, consider volume replacement
- Dermis fat graft can be helpful to correct lid retraction and volume deficit.
Suture-related
- Granuloma
- Inclusion cysts
- Canthal webbing
References and additional resources
- Aakalu VK, Putterman AM. Fat repositioning in lower lid blepharoplasty: the role of titrated excision. Ophthal Plast Reconstr Surg. 2011;27(6):462.
- Atiyeh BS, Hayek SN. Combined arcus marginalis release, preseptal orbicularis muscle sling, and SOOF plication for midfacial rejuvenation. Aesthetic Plast Surg. 2004;28(4):197-202.
- Baker SR. Orbital fat preservation in lower-lid blepharoplasty. Arch Facial Plast Surg. 1999;1(1):33-37.
- Baylis HI, Long JA, Groth MJ. Transconjunctival lower eyelid blepharoplasty. Technique and complications. Ophthalmology. 1989;96(7):1027-1032.
- Carter SR, Seiff SR, Choo PH, Vallabhanath P. Lower eyelid CO(2) laser rejuvenation: a randomized, prospective clinical study. Ophthalmology. 2001;108(3):437-441.
- Cohen SR, Kikkawa DO, Korn BS. Orbitomalar suspension during high SMAS facelift. Aesthet Surg J. 2010;30(1):22-28.
- Collar RM, Lyford-Pike S, Byrne P. Algorithmic approach to lower lid blepharoplasty. Facial Plast Surg. 2013;29(1):32-39.
- Einan-Lifshitz A, Hartstein ME. Treatment of festoons by direct excision. Orbit. 2012 Oct;31(5):303-306.
- Epstein JS. Management of infraorbital dark circles. A significant cosmetic concern. Arch Facial Plast Surg. 1999;1(4):303-307.
- Ghabrial R, Lisman RD, Kane MA, Milite J, Richards R. Diplopia following transconjunctival blepharoplasty. Plast Reconstr Surg. 1998 ;102(4):1219-1225.
- Goldberg RA. Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg. 2000;105(2):743-748; discussion 749-751.
- Goldberg RA, McCann JD, Fiaschetti D, Ben Simon GJ. What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg. 2005;115(5):1395-1402; discussion 1403-1404.
- Hass AN, Penne RB, Stefanyszyn MA, Flanagan JC. Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthal Plast Reconstr Surg. 2004;20(6):426-432.
- Hoenig JF, Knutti D, de la Fuente A. Vertical subperiosteal mid-face-lift for treatment of malar festoons. Aesthetic Plast Surg. 2011;35(4):522-529.
- Kim EM, Bucky LP. Power of the pinch: pinch lower lid blepharoplasty. Ann Plast Surg. 2008;60(5):532-537.
- Korn BS, Kikkawa DO, Cohen SR. Transcutaneous lower eyelid blepharoplasty with orbitomalar suspension: retrospective review of 212 consecutive cases. Plast Reconstr Surg. 2010;125(1):315-323.
- Korn BS, Kikkawa DO, Cohen SR, Hartstein M, Annunziata CC. Treatment of lower eyelid malposition with dermis fat grafting. Ophthalmology. 2008;115(4):744-751.
- Kpodzo DS, Nahai F, McCord CD. Malar mounds and festoons: review of current management. Aesthet Surg J. 2014;34(2):235-248.
- Liao SL, Wei YH. Fat repositioning via supraperiosteal dissection with internal fixation for tear trough deformity in an Asian population. Graefes Arch Clin Exp Ophthalmol. 2011;249(11):1735-1741.
- Lucarelli MJ, Khwarg SI, Lemke BN, Kozel JS, Dortzbach RK. The anatomy of midfacial ptosis. Ophthal Plast Reconstr Surg. 2000;16(1):7-22.
- Mack WP. Complications in periocular rejuvenation. Facial Plast Surg Clin North Am. 2010;18(3):435-456.
- McCann JD, Pariseau B. Lower eyelid and midface rejuvenation. Facial Plast Surg. 2013;29(4):273-280.
- McCord CD Jr. The correction of lower lid malposition following lower lid blepharoplasty. Plast Reconstr Surg. 1999;103(3):1036-1039; discussion 1040.
- McCord CD Jr, Shore JW. Avoidance of complications in lower lid blepharoplasty. Ophthalmology. 1983;90(9):1039-1046.
- McCord CD, Kreymerman P, Nahai F, Walrath JD. Management of postblepharoplasty chemosis. Aesthet Surg J. 2013;33(5):654-661.
- Patel BC, Anderson RL. Transconjunctival blepharoplasty. Plast Reconstr Surg. 1996;97(7):1514-1515.
- Sullivan PK, Drolet B. Extended lower lid blepharoplasty for eyelid and midface rejuvenation. Plast Reconstr Surg. 2013;132(5):1093-1101.
- Trelles MA, Baker SS, Ting J, Toregard BM. Carbon dioxide laser transconjunctival lower lid blepharoplasty complications. Ann Plast Surg. 1996;37(5):465-468.
- Weinfeld AB, Burke R, Codner MA. The comprehensive management of chemosis following cosmetic lower blepharoplasty. Plast Reconstr Surg. 2008;122(2):579-586.
