Reconstruction of Lower Eyelid Defects Involving the Margin
Updated May 2024
Goals, indications, contraindications
Goals
- Primary goal is to re-establish an optimally functioning of the lower eyelid by
- Reconstructing adequate anterior lamella (skin and orbicularis) and posterior lamella (tarsal plate and conjunctiva) to re-establish the original anatomic relationship
- Placing the lower eyelid on proper tension
- Medially, this involves attachment of the medial canthal tendon to the lacrimal crest. If no medial tarsus remains, this may require a medial periosteal strip procedure.
- Laterally, this involves attachment of the lateral canthal tendon to the lateral orbital rim. If no lateral tarsus remains, this may require a lateral periosteal strip procedure.
- Confirming a functional, or recreating a functional, lacrimal drainage system
- Secondary goal is to re-establish optimal lower eyelid and facial cosmesis
Indications
- Full thickness, margin-involving lower eyelid defects require repair
- Primary defect: congenital coloboma or other congenital malformations
- Secondary defect: due to tumor resection, infection (necrotizing fasciitis), or more rarely trauma
- Type of procedure depends on the size of defect and specific patient considerations (history, previous surgery, previous radiation, skin laxity, etc.)
Contraindications
- Relative: compromised vascularity of tissue (previous scar, radiation, previous surgery, etc.)
- Absolute: active infection such as necrotizing fasciitis, nonclear margins (persistent neoplasm)
Preprocedure evaluation
Patient history
- Etiology of defect?
- History of eyelid or facial surgery or trauma or previous grafts?
- History of skin cancers?
- History of radiation?
- History of skin or cutaneous disease or disorders?
- Current medications, particularly anticoagulants?
Clinical examination
- Presence of punctum or obvious disruption of lacrimal system
- Estimate the size of defect recognizing whether the defect
- Spares tarsus medially including the punctum and/or laterally or involves the medial or lateral canthal tendons
- Involves more anterior lamella (skin and orbicularis)
- Repair involves rotating or advancing skin-muscle flaps from surrounding tissue or by a free, full-thickness skin graft.
- Common donor sites include upper eyelid or pre/postauricular tissues.
- Involves significant posterior lamella (tarsus and conjunctiva)
- Repair involves tarsoconjunctival flaps, tarsal transposition, tarsal rotational flaps, free tarsal grafts, the use of various tarsal substitutes, and composite grafts.
Preoperative assessment
- Confirm baseline vision, status of eye and cornea for evidence of exposure keratopathy.
- Confirm presence or lack of a functioning lacrimal system to determine appropriate intraoperative repair/stenting.
- Confirm defect size by placing defect on tension using 2 toothed forceps.
- Determine quality of skin to help guide the choice of surgical technique for repair:
- Amount of laxity
- Previous radiation
- Previous grafting, injury, scarring
- Possible donor tissue:
- Inspect other eyelid for integrity of upper eyelid skin.
- Evert upper eyelids for status of tarsus.
Procedure alternatives
Lower eyelid defects involving the margin require surgical repair to avoid a “notch” at the healing site and re-establish properly functioning eyelids, which protect the globe.
If the defect is minimal and lateral and the eyelid is functioning well to protect the corneal health and health of the globe, one could consider allowing the defect to heal by secondary intention after discussion the risks/benefits with the patient.
Surgical techniques
Surgical techniques employed for reconstruction of lower eyelid defects involving the margin must involve repair of both the anterior and posterior lamella with the goal of re-establishing the native relationship of anterior and posterior lamellae.
Defects involving up to half of lower lid
- Primary closure (“wedge repair”) with or without internal cantholysis (and canthotomy) allowing medial mobilization of the lateral eyelid
- Lamellar repair/sutures of posterior lamella for strength
- Interrupted sutures to repair anterior lamella with care taken to evert wound edges on the eyelid margin, which will retract or flatten with healing
- Primary lamellar closure of the posterior lamella with with use of a subciliary incision to allow for anterior lamellar tissue mobility and improved anterior wound closure.
- Then repair of the anterior lamella by using interrupted sutures to reoppose the anterior lamella to the posterior lamella, “distributing” any redundancy of the anterior lamella along the repaired posterior lamella.
- This avoids the redundancy of anterior lamella noted with “wedge repair.”
- Exceptions in size may be made based on the laxity or lack of laxity of the lower eyelid skin.
Defects involving 2/3rds–3/4ths of lower lid
As always, repair must involve repair of both the anterior and posterior lamellae, re-establishing this relationship.
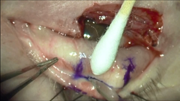
- Hughes and modified Hughes flap (tarsoconjunctival flaps from the upper eyelid)
- Method: An upper eyelid flap of tarsus and conjunctiva (posterior lamella) in conjunction with a skin graft or myocutaneous advancement flap (anterior lamella) is used to repair the lid defect.
- Advantages:
- Similarity of tissue to native lower eyelid
- Ability to repair larger defects
- Good vascular supply
- Disadvantages:
- Typically involves closure of the operative eyelid/occlusion of the eye for 4 weeks
- However, more recent literature supports earlier severing of the flap as soon as 7 days or 2 weeks.
- May require a skin graft, 2-stage procedure, postoperative erythema of the lower eyelid, and upper eyelid retraction and/or kinking

Figure 1. Hughes flap 1 of 4. Image courtesy Gregory J. Griepentrog, MD.

Figure 2. Hughes flap 2 of 4. Image courtesy Gregory J. Griepentrog, MD.
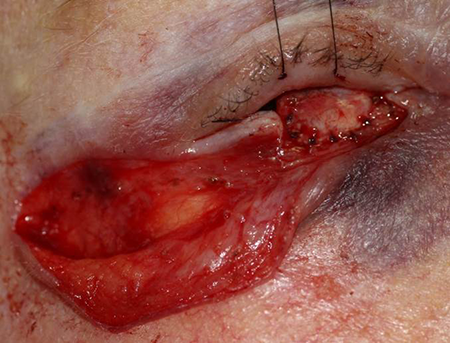
Figure 3. Hughes flap 3 of 4. Image courtesy Gregory J. Griepentrog, MD.

Figure 4. Hughes flap 4 of 4. Image courtesy Gregory J. Griepentrog, MD.
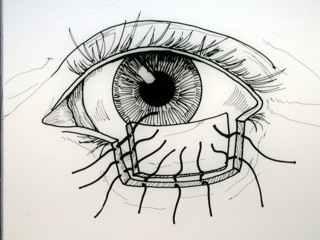
Figure 5. Free tarsoconjunctival. Image courtesy Michael J. Hawes, MD.
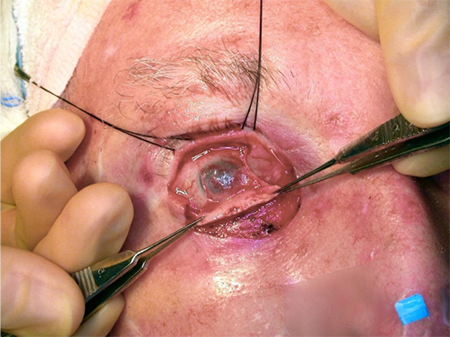
Figure 6. Hughes flap. Image courtesy Michael J. Hawes, MD.
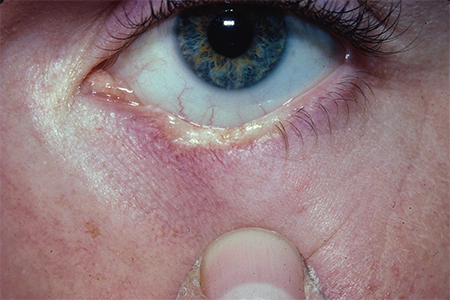
Figure 7. Hughes preoperative. Image courtesy Rona Z. Silkiss, MD, FACS.

Figure 8. Hughes intraoperative. Image courtesy Rona Z. Silkiss, MD, FACS.
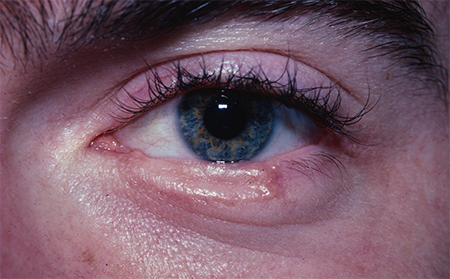
Figure 9. Hughes postoperative. Image courtesy Rona Z. Silkiss, MD, FACS.
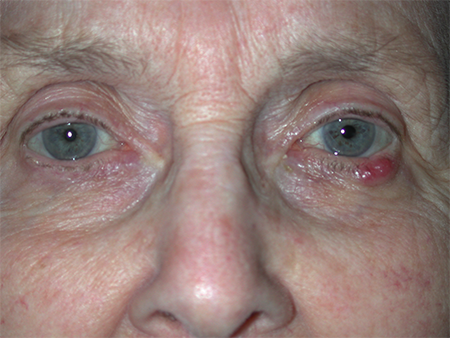
Figure 10. Merkel Hughes preoperative. Image courtesy Rona Z. Silkiss, MD, FACS.
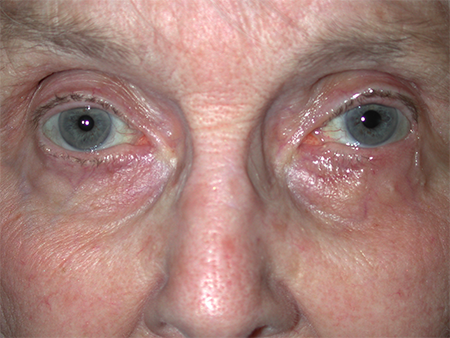
Figure 11. Merkel Hughes postoperative. Image courtesy Rona Z. Silkiss, MD, FACS.
- Hewes flap (tarsoconjunctival pedicle flap; temporal advancement flap)

Video 1. Video courtesy Michael J. Hawes, MD.
- Method:
- A tarsal transposition procedure that involves a transposition of conjunctiva and tarsus, hinged at the lateral canthal tendon, into a lateral lower eyelid defect
- Anterior lamella is reconstructed by an advancement skin-flap.
- Advantages:
- Does not require closure of the operative eyelids/occlusion of the eye
- Single stage procedure
- Excellent tissue match
- Disadvantages:
- Best suited for lateral eyelid defects but able to be used for central or medial defects when the lateral lower eyelid is preserved
- Rounding of lateral canthus
- Postoperative ectropion, particularly if the flap is too long
- Tenzel flap — semicircular rotational flap
- Method:
- A skin and muscle incision is begun at the lateral canthus and curves superiorly and temporally in a semicircular fashion.
- A lateral canthotomy is performed beneath the flap and the inferior portion of the lateral canthus is cut. This allows medial mobilization of the lateral eyelid and the margin defects and lateral canthus are repaired by primary closure.
- Advantages:
- Able to repair medial defects
- Good tissue match
- Able to provide more length due to the circumferential incision line
- Superior tension on the eyelid
- Palpebral fissure is open postoperatively
- No contralateral donor site
- Disadvantages:
- Best suited for central defects 1/2 to 3/4 of the eyelid, but can be combined with other techniques to repair all aspects of the lower eyelid
- Possible lateral canthal webbing, ectropion, lid notching, symblepharon, and tissue fullness of the lateral lid
- Unipedicle flap
- Method:
- Full-thickness unipedicle flap from the upper tarsal portion of the upper eyelid
- Best suited for shallow defects of the temporal lower eyelid
- Advantages:
- One-stage, single-pedicle, replacement of loss of tissue with identical tissue — skin, orbicularis, tarsus, conjunctiva
- Avoidance of upper eyelid retraction by graded recession of the levator and Muller’s muscle
- Pedicle suspends and supports the eyelid, resulting in a decreased incidence of lower eyelid retraction, laxity, and ectropion (similar to Hughes).
- Open palpebral fissure postoperatively
- Disadvantages:
- Theoretical risk of upper eyelid retraction limited by levator and Muller’s muscle recession
- Notching of the lower lid less ideal for medial defects
- Autologous graft
- Anterior lamella must be reconstructed from tissue with sufficient blood supply (flaps) to nourish the posterior lamella such as skin and muscle from the cheek and temporal regions, the mid-forehead, or the upper eyelid
- Must fixate to the periosteum if no tarsus remains medially or laterally
- Advantage: good support
- Disadvantages:
- Requires additional donor site and surgery for the patient
- Generally thick and immobile, providing less desirable eyelid function and cosmesis postoperatively
- Free tarsus: Medial can be combined with nasal-based, skin-muscle, pedicle flap, central or lateral lower eyelid defects.
Video 2. Video courtesy Michael J. Hawes, MD.
- “Sandwich technique”:
- The orbicularis muscle adjacent to the defect is mobilized and the inner surface is covered by a free tarsoconjunctival graft from the ipsilateral or contralateral upper eyelid.
- The outer surface is covered with a free skin graft from the ipsilateral or contralateral upper eyelid.
- Nasal cartilage (fixate to periosteum if no tarsus remains, used with Mustarde cheek-rotational
- Auricular cartilage
- Hard palate
- Nonautologous (synthetic)
- AlloDerm — acellular, human dermal graft
- Permacol — biomaterial made from acellular, cross-linked, porcine dermal collagen
- tarSys — ideal for repair of retraction
Defects involving entire lower lid
- See previous section for details on method, advantages, and disadvantages.
- A Hughes tarsoconjunctival flap can be used in some cases, but the upper eyelid tarsal plate is narrow medially and laterally in most patients, and if medial and lateral canthal defects are simultaneously present, a tarsoconjunctival flap might not be able to span the defect, however, a combination of techniques can be employed.
- Autologous grafts: See previous section.
- Bipedicle full-thickness, upper-eyelid flap from the upper eyelid into lower eyelid anterior lamella defect
- Intraoperative adjustment of the donor eyelid height is performed by recessing the levator aponeurosis, which is necessary to avoid postoperative upper eyelid retraction.
Defects involving lacrimal system
- Assess for preservation or disruption of punctum, canaliculus, lacrimal sac intraoperatively by probing and irrigating (can use fluorescein for improved visualization)
- If disrupted, place
- Bicanalicular stent such as the Crawford stent through the entire nasolacrimal system
- Bicanalicular “donut” stent if a common canaliculus is present and no disruption distal to the common canaliculus
- Mini Monoka or other unilateral stent if only disruption of the lower system and unable to place other stents
- Repair remaining canaliculus with pericanalicular, absorbable sutures such as 7-0 Vicryl.
- Repair eyelid as described above with the goal of re-establishing native relationship of anterior and posterior lamella and eyelid to facilitate drainage through the recreated lacrimal system.
Controversies
Due to the variable nature of lower-eyelid, margin-involving defects, there is a wide variety for repair. Ultimately the choice of surgical technique is based on the size and nature of the defect and the training and comfort of the surgeon.
Patient management: treatment and follow-up
- Postoperative instructions:
- Some clinicians patch the eyelid for 1 week postoperatively with care taken to support the eyelid/cheek superiorly to avoid retraction.
- If there is concern for lower lid retraction, consider placing the lower eyelid on tension by securing a Frost suture (through the lower eyelid gray line) to the patient’s ipsilateral forehead.
- If a skin graft has been placed, one can place a bolster over the graft and under the patch.
- Minimal activity for 1-2 weeks to avoid bleeding, hematoma, graft failure
- If no history of heart attack or stroke, consider asking patients’ primary care provider if anticoagulants can be held 10–14 days prior to surgery.
- Recommend deferring final decisions regarding anticoagulation to patients’ primary care provider.
- Medications prescribed:
- No current evidence to support the routine use of intraoperative IV antibiotics or postoperative oral antibiotics
- Some surgeons prescribe postoperative oral antibiotics (e.g., Doxycycline 100 mg BID x 1 week), particularly if the eyelid is patched for an entire week or if there is a donor site/graft in place.
- Once the patch is removed at the 1-week postoperative visit, antibiotic ointment (e.g., erythromycin ophthalmic ointment) is applied to the incisions TID x 1 week.
- Similar topical antibiotics are prescribed for donor sites.
- Other management considerations
- If there is concern for postoperative erythema, consider adding topical steroid or combined steroid-antibiotic ointment and following IOP.
- Common treatment responses, follow-up strategies
- The eyelids are a highly vascularized tissue and therefore tend to heal well following repair.
- Take care to re-establish the relationship of the anterior and posterior lamella, respect the vascularization of the eyelids, and place the lower eyelid on proper tension.
- Secondary treatments related to improper eyelid position, scarring, retraction, graft failure are discussed below.
Preventing and managing treatment complications
- Facial nerve paralysis
- Particularly with the cheek flap repair
- Prevent by being aware of the path and depth of the facial nerve and avoiding these planes (remaining in a subcutaneous plane) during surgical repair
- Ectropion with exposure keratopathy and/or lower eyelid retraction (lagophthalmos) with exposure keratopathy overtime
- Ensure appropriate lower lid tension by always stabilizing the lower lid with a lateral tarsal strip or periosteal strip to provide adequate stability of the lower eyelid, which is undergoing simultaneous reconstruction.
- Ensure that the anterior lamella slightly overrides the posterior lamella during the repair.
- Starting about 2 weeks following repair, massage in an upward direction, usually 20 strokes at least 3 times per day, and the more often, the better.
- Frequent lubrication, e.g., artificial tears, ointments
- If no improvement after 1 month of massage, if main etiology is scarring or cicatricial changes, consider steroid and/or 5-fluorouracil injections.
- If no improvement after 3–6 months:
- If main issue is laxity, consider further lower lid tightening.
- If main issue is retraction/cicatricial change, consider other surgical revision, e.g., grafting, spacer.
- Erythema of eyelid margin
- Common after 2nd-stage Hughes procedures
- Optimally, re-establish the original relationship between anterior and posterior lamella as well as the position of the lower eyelid to avoid exposure of the eyelid margin.
- Topical steroid-antibiotic ointment
- When placing a patient on topical steroids, follow IOP weekly, then monthly.
- If no improvement with conservative management, consider further surgical repair of the lower eyelid margin and position.
- Excessive facial scarring
- As much as possible, place incisions in the patient’s natural creases.
- Aggressive massage
- Vitamin E
- Mederma
- Steroid injections
- Other scar management
- 5-fluorouracil injections (OPRS 2020:36:222)
- If repair is following excision of neoplasm, also monitor for evidence of recurrence.
References and additional resources
- Anderson RL, Jordan DR, Beard C. Full-thickness unipedicle flap for lower eyelid reconstruction. Arch Ophthalmol 1988;106:122-125.
- Anderson RL, Weinstein GS. Full-thickness bipedicle flap for total lower eyelid reconstruction. Arch Ophthalmol 1987;105:570-576.
- Bartley GB, Kay PP. Posterior lamellar eyelid reconstruction with hard palate mucosal graft. Am J Ophthamol. 1989;107:609-612.
- Baylis HI, Rosen N, Neuhaus RW. Obtaining auricular cartilage for reconstructive surgery. Am J Ophthalmol. 1982;93:709-712.
- Bee YS, Alonzo B, Ng JD. Review of AlloDerm acellular human dermis regenerative tissue matrix in multiple types of oculofacial plastic and reconstructive surgery. Ophthal Plast Reconstr Surg. 2014 [Epub ahed of print].
- Boynton JR. Semicircle flap reconstruction “plus.” Ophthalmic Surg. 1993;24:826-830.
- Bui AD, Grob SR, Tao JP. 5-Fluorouracil Management of Oculofacial Scars: A Systematic Literature Review. Ophthalmic Plast Reconstr Surg. 2020 May/Jun;36(3):222-230. doi: 10.1097/IOP.0000000000001532. PMID: 31923097.
- Callahan MA, Callahan A. Mustarde flap lower lid reconstruction after malignancy. Ophthalmology. 1980;87:279-286.
- Cannon PS, Madge SN, Kakizaki H, Selva D. Composite grafts in eyelid reconstruction: the complications and outcomes. Br J Ophthalmol. 2011;95(9):1268-1271.
- Codner MA, McCord CD, Mejia JD, Lalonde D. Upper and lower eyelid reconstruction. Plast Reconstr Surg. 2010;126(5):231e-245e.
- Custer PL. Tarsal kinking after hughes flap. Ophthal Plast and Reconstr Surg. 1998;14(5):349-351.
- Goldstein MH. “Orbiting the orbicularis” – restoration of muscle-ring continuity with myocutaneous flaps. Plast Reconstr Surg 1983;72(3):295-299.
- Hawes MJ. Free autogenous grafts in eyelid tarsoconjunctival reconstruction. Ophthal Surg 1987;18(1):37-41.
- Hawes MJ, Grove AS Jr, Hink EM. Comparison of free tarsoconjunctival grafts and Hughes tarsoconjunctival grafts for lower eyelid reconstruction. Ophthal Plast Reconstr Surg. 2011;27(3):219-23
- Hewes EH, Sullivan JH, Beard C. Lower eyelid reconstruction by tarsal transposition. Am J Ophthalmol 1976;81:512-514.
- Hughes WL. A new method for rebuilding a lower lid. Arch Ophthalmol 1937;17:1008-1017.
- Hughes WL. Reconstructive Surgery of the Eyelids, ed 2. St. Louis, CV Mosby Co, 1954, pp 120-124.
- Khan JA and Garden VS. Combined flap repair of moderate lower eyelid defects. Ophthal Plast Reconstr Surg 2002;18(3):202-204.
- Leibovitch I, Selva D. Modified Hughes flap: division at 7 days. Ophthalmology. 2007;111(12):2164-2167.
- Leone CR, Hand SI. Reconstruction of the medial eyelid. Am J Ophthalmol 1979;87:797-801.
- Leone CR, Van Gemert JV. Lower lid reconstruction using tarsoconjunctival grafts and bipedicle skin-muscle flap. Arch Ophthalmol. 1989;107:758-760.
- Liao SL, Wei YH. Correction of lower eyelid retraction using tarSys bioengineered grafts for graves ophthalmopathy. Am J Ophthalmol. 2013; 156(2):387-392.
- Matsuo K, Hirose T, Takahashi N, Iwasawa M, Satoh R. Lower eyelid reconstruction with a conchal cartilage graft. Plast Reconstr Surg 1987;80(4):547-552.
- McNab AA. Martin P, Benger R, O’donnell B, Kourt G. A prospective randomized study comparing division of the pedicle of modified hughes flaps at two or four weeks. Ophthal Plast Reconstr Surg 2001;17(5):317-319.
- Miller EA, Boynton JR. Complications of eyelid reconstruction using a semicircular flap. Ophthal Surg 1987;18(11):807-810.
- Mustarde JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45:146-150.
- Paridaens D, van den Bosch WA. Orbicularis muscle advancement flap combined with free posterior and anterior lamellar grafts: a 1-stage sandwich technique for eyelid reconstruction. Ophthalmology. 2008;115(1):189-94.
- Peter NM, Kumar B. Permacol in eyelid reconstruction – a novel use. Orbit. 2013;32(1):57-9.
- Stephenson CM, Brown BZ. The use of tarsus as a free autogenous graft in eyelid surgery. Ophthalmic Plast Reconstr Surg 1985;1:43-50.
- Taban M, Douglas R, Li T, Goldberg RA, Shorr N. Efficacy of “thick” acellular human dermis (AlloDerm) for lower eyelid reconstruction: comparison with hard palate and thin AlloDerm grafts. Arch Facial Plast Surg 2005;7(1):38-44.
- Tenzel RR. Reconstruction of the central one half of an eyelid. Arch Ophthalmol. 1975;95:125-126.
- Tenzel RR, Stewart WB: Eyelid reconstruction by the semicircle flap technique. Ophthalmology. 1978;85:1164-1169.
- Wessels WL, Graewe FR, van Deventer PV. Reconstruction of the lower eyelid with a rotation-advancement tarsoconjunctival cheek flap. J Craniofac Surg. 2010;21(6):1786-1789.
