Mandible Fractures
Updated August 2024
Emily Bratton, MD; Brian Willoughby, MD; Aaron T. Liddell, MD, DMD, FACS; Raymond Cho, MD
Establishing the diagnosis
Etiology and epidemiology
- Mandible fractures are common facial fractures (second only to nasal fractures).
- Leading cause in developed countries is interpersonal violence followed by motor-vehicle accidents (MVAs)
- Occur most frequently in males in the third decade
- Fractures secondary to violence often occur at the angle of the mandible (King, Am J Otolaryngol, 2004).
- Fractures secondary to MVAs most often result in multiple injury sites; most commonly involving the condyle, body, and parasymphysis (King, Am J Otolaryngol, 2004).
- The majority of fractures occur at more than one site, often bilaterally (Ogundare, JOMS 2003; Kubilius, Stomatologija 2009)
- Fall to chin = bilateral condylar fractures
- Blow to mandible = ipsilateral parasymphyseal fracture + contralateral angle fracture
- 45% occur in conjunction with other injuries; 10% are lethal (Haug, JOMS, 1990).
History
- Substance abuse
- Mechanism of injury
- Concurrent injury
- Cervical spine
- Other facial fractures
Clinical features
Anatomy (Figure 1):
- Mandible
- Symphysis/parasymphysis (17–22%) (Figure 2)
- Alveolar (2–4%)
- Body (16–29%)
- Angle (25–31%)
- Ramus (2–4%)
- Condyle (26–29%)
- Subtypes: head, neck, subcondylar
- Coronoid (1–2%)
- Important muscles — determine dislocation of mandible after fracture:
- Masseter: elevates mandible
- Origin: zygomatic arch
- Insertion: mandibular angle/ramus
- Temporalis: elevates and retracts the mandible
- Origin: temporal fossa of the temporal bone
- Insertion: coronoid process
- Lateral pterygoid: protrude/depress mandible; excursive movements
- Superior head — origin: greater wing of the sphenoid
- Inferior head — origin: lateral surface of the lateral pterygoid plate
- Insertion — condyle/TMJ medial pterygoid: protrude/elevate mandible; excursive movements
- Superficial head — origin: tuberosity of maxilla
- Deep head — origin: medial surface of lateral pterygoid plate/palatine bone
- Insertion: medial surface of ramus and angle of mandible
- Anterior digastric: depresses mandible, elevates/retrudes tongue
- Geniohyoid/mylohyoid: depresses mandible and protrudes/extrudes tongue
- Mentalis: elevates the lower lip
- Depressor labii inferioris: depresses lower lip
- Mental nerve:
- Sensory somatic nerve: supplies the anterior chin, lip, buccal gingiva of mandibular anterior and premolar teeth
- Typically exits apical and inferior to the 1st and 2nd premolar roots
- Distal-most/terminal end of the mandibular nerve (V3)
- The mandibular nerve passes through the skull base through the foramen ovale into the inferotemporal fossa, where it gives rise to motor branches that innervate the muscles of mastication and sensory branches, including the inferior alveolar nerve
- Inferior alveolar nerve is the largest sensory branch of the mandibular nerve
- It enters, at the lingula, into the mandibular canal and exits between the first and second premolar roots at the mental foramen
- Teeth (Figure 3):
- Surface: Labial (surface toward lip for anterior teeth); Buccal (surface toward buccal mucosa for posterior teeth); Lingual (faces the tongue for lower teeth); Palatal (toward the palate for the upper teeth); Mesial (direction toward the anterior midline of the dental arch); Distal (direction toward the last tooth in each quadrant of the dental arch)
- Numbered 1–32:
- Right-upper 3rd molar is 1.
- Right-lower 3rd molar is 32.
- Names (Figure 3):
Fracture classification and clinical description:
- Anatomic location
- Fracture terminology
- Simple/compound/comminuted/greenstick
- Simple: External Skin and Mucosa are Intact
- Compound (open): Laceration of Skin or Mucosa present or passes through tooth root/periodontal ligament
- Comminuted: multiple fragments of bone
- Greenstick: involves only one cortex
- Pathologic fracture: occurs through bone weakened by preexisting disease
- Atrophic fracture: occurs from bone atrophy by loss of supporting alveolar bone in edentulous mandibles
- Favorable: reduced by muscle pull
- Unfavorable: fractures distracted by muscle pull; require greater fixation
- Dentition status
- Dentulous (with teeth)
- Edentulous (without teeth)
- Stability — favorable versus unfavorable fracture:
- Muscles of mastication and suprahyoid muscles lead to instability of the mandible and fracture displacement, requiring greater fixation.
- Example 1: Mandibular angle fractures are almost always unfavorable due to instability; vertical pull due to masseter, medial pterygoid, and temporalis muscles. (Figure 4)
- Example 2: In symphysis and parasymphysis fractures, masseter muscle pull will cause lingual displacement and rotation of the teeth. Distraction of the fracture site will result in lingual splay.
Sites of weakness of the mandible:
- Fractures tend to occur in areas of greatest tension
- Third molar (especially if impacted) correlated with angle fractures (Figure 5)
- Canine roots
Figure 1. (Image removed at request of copyright holder.) Anatomy of the mandible and fracture sites. The mental foramen (orange) is found between the first and second premolars (orange). Coronoid process (blue). Condylar process (red). Angle (purple). The ramus and body are labeled. Lingual (green). Alveolus (yellow).

Figure 2. A teenage girl who sustained bilateral parasymphyseal fractures after being bucked from her horse. IMF was established using her existing braces. An intraoral approach was used to expose the bilateral fracture. Note 2-point fixation with 1 miniplate and 1 reconstruction plate. The mental nerve is indicated by the green arrow.
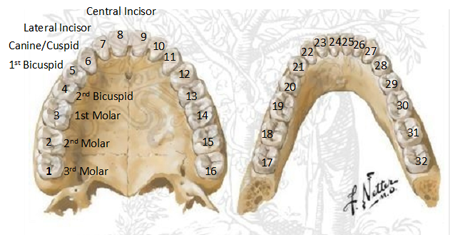
Figure 3. (Image removed at request of copyright holder.)Numbering and names of teeth. Numbering starts with the right upper (maxillary) 3rd molar as number 1 and continues to the left, so that the left 3rd upper (maxillary) molar is number 16. The numbering continues to the left lower 3rd (mandibular) molar as number 17 and then through the right 3rd (mandibular) molar as number 32.
Figure 4. Favorable versus unfavorable fractures. Upper left shows a mandibular fracture proximal to the angle. This is a favorable fracture. Lower right shows an unfavorable fracture of the mandibular angle with forces resulting in an unstable fracture.
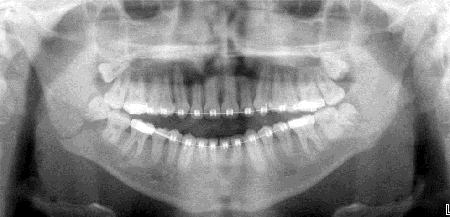
Figure 5. Panorex of angle fracture. Demonstrating a weak point at the 3rd molar root resulting in an angle fracture.
Testing
- Acute management
- Secure airway (tongue falling back)
- Blood clots (submandibular hemorrhage)
- Fractured teeth, broken fillings, dentures
- Hemorrhage
- Identify soft- tissue lacerations
- Management of food and fluid
- Symptoms
- Pain
- Occlusal abnormality
- Paresthesia
- Bleeding/swelling
- Examination
- External exam looking for changes in facial bony architecture and lacerations
- Lacerations under the chin are common in symphysis fractures
- Tenderness or step-offs with palpation along the inferior border of the mandible
- Tenderness of palpation in preauricular area can indicate condylar fracture
- Hemorrhage from external auditory canal (EAC) is frequently seen in condylar fracture (due to laceration of the cartilaginous EAC)
- Limitation of jaw movement/mandibular range of motion
- Lateral deviation on opening to the side of the fracture (condylar fractures), inability to chew, loss of opening of jaw due to muscle splinting, trismus, joint dysfunction, coronoid impingement by zygomatic fractures.
- Anesthesia, hypoesthesia, paraesthesia of lower lip, teeth, gingiva (V3 inferior alveolar nerve damage); damage to the lingual nerve causing temporary or permanent anesthesia to the ipsilateral tongue
- Intraoral bruising
- Bruising of the floor of mouth might indicate a symphysis/parasymphysis/body fracture
- Gingival laceration
- Sublingual hematoma
- Fractures of teeth
- Occlusal derangement of teeth (document preexisting malocclusion)
- Angle class I: normal anteroposterior relationship of mandible and maxilla; mesiobuccal cusp of the maxillary first molar occludes within the buccal groove of the mandibular first molar.
- Angle class II: posterior relationship of the mandible to the maxilla; mesiobuccal cusp of the maxillary first molar occludes mesial to the buccal groove of the mandibular first molar.
- Angle class III: anterior relationship of the mandible to the maxilla; mesiobuccal cusp of the permanent maxillary first molar occludes distal to the buccal groove of the mandibular molar.
- Imaging modalities
- Panoramic tomography (Panorex) (Figure 6)
- View of entire mandible
- Patient has to be able to sit upright.
- Valuable for postoperative assessment
- Maxillofacial CT without contrast (1-mm cuts)
- 3D reconstruction (Figure 7)
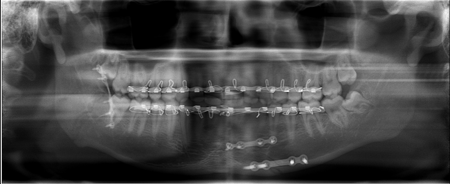
Figure 6. Panorex image showing Erich arch bars, a 2-plate technique for a parasymphysis fracture (bottom right) and a Champey technique (left).
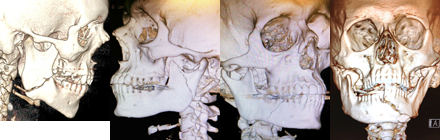
Figure 7. 3D CT reconstruction of mandible fractures. Left to right: angle, subcondylar, body, symphysis/parasymphysis.
Patient management: treatment and follow-up
General principles
- Restore premorbid occlusion.
- Repair all skeletal and soft tissue injuries.
- Use pre-existing lacerations to access fractures, when possible.
- Reduce and stabilize fractures.
- Assess for concurrent facial fractures.
Nondisplaced fractures with good occlusion
- Must have reproducible occlusion
- Liquid advancing to soft diet for 8 weeks
- Can use for nondisplaced ramus fractures or condylar fractures with reproducible occlusion
Timing of surgery
- Although repair should not be extensively delayed, multiple authors have found no correlation between delay (3–4 days) in repair and postoperative complications such as malunion/nonunion of the fracture (Barker, Laryngoscope 2011; Gutta, JOMS 2014).
Use of antibiotics
- No benefit of use past 24 hours after surgery (Ahubaker, JOMS 2001; Miles, JOMS 2006)
- Use preoperatively, especially for those fractures that extend to the dentoalveolar ridge or through the periodontal ligament.
- Closed condylar fractures do not require antibiotics.
Surgical methods
Closed reduction (secondary bone healing):
- For favorable, nondisplaced fractures, some pediatric fractures (if involve developing dentition), grossly comminuted fractures (avoids stripping periosteum from bone, but requires intermaxillary fixation or placement of external fixator), coronoid fracture, nondisplaced condylar fractures
- Maxillomandibular fixation (MMF/IMF)
- Arch bars (Erich arch bars) (Figure 8)
- Circumdental wire used to fasten each bar to the dentition of upper and lower teeth with lugs away from the crowns of the teeth
- Place patient in maximum intercuspation and place MMF wires and elastics.
- Ivy/eyelet loops
- Used in minimally displaced fractures
- Patient must have full dentition.
- Essing wire (Figure 9)
- Used for alveolar process fractures and for tooth avulsion
- Intermaxillary fixation screws (Figure 10)
- Place 2.5‑mm self-drilling/tapping screws
- Requires 2–3 screws per quadrant
- Alternative to arch bars, or temporary during open reduction
- Splints
- Frequently used in pediatric fractures and in fractures with significant comminution
- Bridal wires
- Single circumdental wire used for stabilization of mobile fracture segments
- Contraindications to closed reduction
- Compromised pulmonary function/COPD
- Poorly controlled seizures
- Severe nausea
- Psychiatric or neurologic disorders
- Length of fixation
- Age
- Adult: 3–4 weeks
- Children: 2–3 weeks
- Elderly: 6–8 weeks
- Condylar: 2–4 weeks
Open reduction:
- For unfavorable fractures, those associated with midface fractures that require a stable mandible, and edentulous/atrophic mandibles, bilateral condylar fractures
- Load-bearing versus load-sharing
- Load-bearing requires rigid plate to bear the entire force of movement at the fracture.
- Comminuted fractures
- Atrophic edentulous fractures
- Load-sharing: fracture stability supplied by shared buttressing by significant bone contact and the plate used for fixation
- Lag screw
- Compression plates
- Champy miniplate
- Materials for open reduction
- Compression plates
- Dynamic compression plate (DCP)
- Requires tension band
- Can be placed intraorally
- Eccentric dynamic compression plate (EDCP) (Figure 11)
- Avoids use of tension band
- Placed either intra or extraorally
- Screw engages plate and imparts compression across fracture segment, so that fragments are brought together with compression and interfragmentary friction
- Allows for primary bone healing
- Rigid, not bendable
- Place at inferior border of the mandible with bicortical screws.
- Must use tension band at the superior surface to counteract compressive spread of superior surface by the compression plate; examples of tension band to use concurrently:
- Arch bars
- Miniplate with monocortical screws
- Place tension band prior to compression plate.
- Lag screws (Figure 12)
- Correct occlusion must be established prior to fixation of fracture with lag screws (MMF)
- Screw placed perpendicular to fracture
- 2–3 screws placed across fracture to overcome rotational force
- Must be placed at a divergent angle
- Reconstruction plates
- Load-bearing
- Screws greater than 2‑mm diameter (2.3, 2.4, 2.7, 3.0)
- 3 screws on each side of fracture (maximum strength with 4)
- Locking plates
- Plate bears 100% of functional force at fracture site.
- For load-bearing, reduction of fracture
- Use in atrophic, edentulous, comminuted, defect fractures.
- Nonlocking plates
- Noncompression miniplates (i.e., Champy technique)
- Champy’s line of osteosynthesis
- Masticatory forces produce tension in the alveolar region and compression in the lower border of the mandible
- A transitional zone between the areas of tension and compression corresponds to a line of zero force, where the miniplate should be placed
- Load sharing reduction of fracture (non-rigid fixation)
- Bone assumes most of functional load
- Allows for primary and secondary bone healing
- Easily bent
- Short period of IMF Recommended
- Greater likelihood of failure with delay of fracture fixation (use within first 24 hours)
- Guidelines by Champy:
- Use of a single noncompression miniplate on the superior border of mandible angle fractures on the external oblique line (Figure 5)
- 1 plate applied just below root apices and above inferior alveolar nerve if fracture is posterior to mental foramen
- 2 plates if fracture anterior to mental foramen to counteract torsional forces; 1 plate below tooth root apices and one at inferior border of mandible (Figure 6, Figure 13)
- Resorbable materials
- Polylactic acid, polyglycolic acid, polydioxanone
- Indications for use: children
- Intraosseous wiring (wire osteosynthesis)
- Direct skeletal fixation
- Keeps fragments exactly aligned but must rely on other forms of fixation to maintain stability (splints, IMF)
- Straight wire, figure‑8 wire, transosseous circummandibular wire
- Mostly used in mandibular angle at superior border of fracture site with removal of 3rd molar (to prevent rotation of the proximal fracture segment)
- Can be used at the inferior border of symphyseal and parasymphyseal fractures
External fixation:
- Comminuted fractures
- Avulsive gunshot wounds
- Edentulous with severely atrophic bone
- Poor candidate for open or closed reduction

Figure 8. Erich arch bars.

Figure 9. Left: alveolar process fracture. Right: Postoperative reduction with Essing wire.
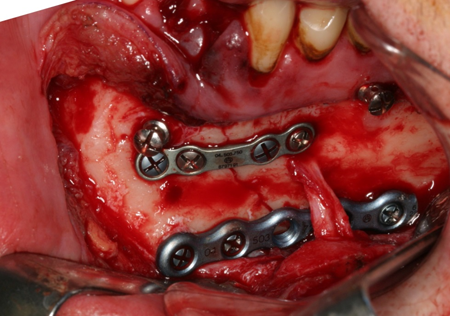
Figure 10. 2-plate technique with IMF screws for fixation visualized.
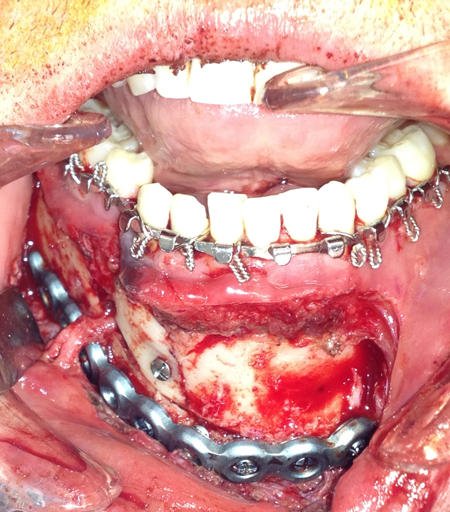
Figure 11. Eccentric dynamic compression plate at the inferior border of the mandible with arch bars used as the tension band.
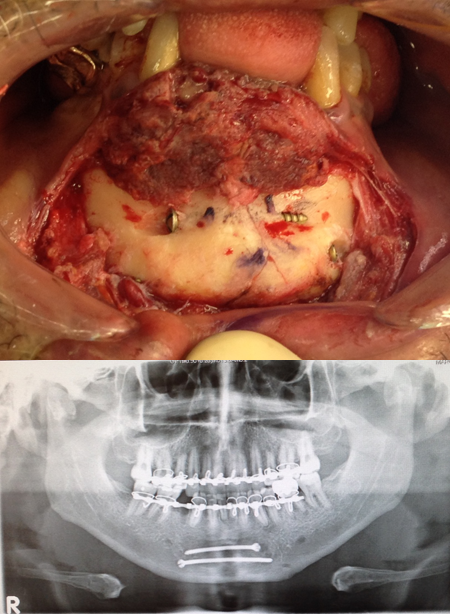
Figure 12. Top: lag screw insertion through symphysis fracture. Bottom: Panorex with lag screw fixation of a symphysis fracture and Erich arch bars.
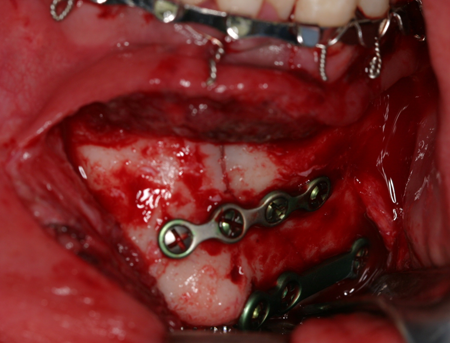
Figure 13. Champy miniplate technique for a symphysis fracture anterior to the mental foramen.
Type of fracture and principles of fixation
Condylar fracture:
- Condylar head fractures are uncommon in adults
- MMF should be avoided due to risk of TMJ ankylosis
- Aim for early functional rehabilitation
- Condylar neck/subcondylar fractures are common
- Most advocate closed reduction
- Nondisplaced with good occlusion: brief period of MMF versus elastic guidance and early functional rehabilitation
- Open reduction:
- Comparable long-term range of motion and occlusion in patients with condylar fractures treated with open reduction and internal fixation versus closed reduction and maxillomandibular fixation has been demonstrated (Palmieri, JOMS 1999;De Rui, Int JOMS 2001)
- Indications for open reduction (Zide, JOMS 1983)
- Condylar displacement into the middle cranial fossa or external auditory canal (Figure 14)
- Inability to obtain adequate occlusion using closed treatment
- Lateral extracapsular dislocation
- Contaminated, open joint wound
- Bilateral condylar fractures in an edentulous patient when splints are unavailable or impossible due to alveolar ridge atrophy
- Bilateral/unilateral condylar fractures when splinting is not recommended because of concomitant medial conditions
- Bilateral fractures associated with comminuted mid-face fractures (must re-establish posterior facial vertical dimension)
- Bilateral subcondylar fractures associated with retrognathia, open bite with periodontal problems, loss of multiple teeth, unstable occlusion due to orthodontics, unilateral condylar fracture with unstable fracture base.
- Condylar head/intracapsular fractures: rare; MMF often contraindicated given high risk for TMJ ankylosis
- Condylar neck/subcondylar fractures: most common in adults; often treated with closed reduction. Subcondylar fractures might have sufficient proximal bone for ORIF.
- Endoscopic approach
- Some surgeons advocate endoscopic approach through a transoral incision that offers comparable functional result of reduction with less risk to the facial nerve (Lee, Plastic Surgery 2006; Martin, Atlas Oral Maxillofac Surg Clin North Am 2003; Schmeizer, JOMS 2009; Kellman, Fac Plast Surg 2009)
- The operative time might be increased due to the learning curve of operating the endoscope through a transoral route.
Coronoid fracture:
- Does not require treatment unless impingement from zygomatic fracture
Angle fracture:
- Can result from area weakened by 3rd molar
- Simple fractures can be treated with 6 weeks of MMF
- 2 noncompression miniplates, inferior plate with bicortical screws
- Inferior reconstruction plate with superior monocortical mini plate
- Champy showed that functional loading of a simple angle fracture creates tension on the superior border of the fracture and is treated by a tension band. Failure to do so can allow the fracture to open (Figure 15). Compression occurs on the lower border during functional loading and stabilizes this portion of the fractured bone. The Champy miniplate fixation technique (Figure 16) extends medial to lateral over the external oblique ridge. For additional stability, a second inferior border plate via transcutaneous trocar technique can be added to the Champy technique or to a superior border plate.
- Complex fractures might require reconstruction plate fixation.
Body fracture:
- Simple fractures can be treated with arch bars and 6 weeks of MMF alone. They can also be treated with MMF with miniplate fixation.
- Osteosynthesis with two straight plates or a reconstruction plate at the inferior border
- Complex fractures and edentulous fractures require reconstruction plate fixation.
Symphyseal/parasymphyseal (Figure 2):
- Simple fractures: MMF alone (6 weeks)
- 2 straight/miniplates
- 2 lag screws
- 1 compression plate should also be accompanied by arch bars (arch bar maintained for 5–6 weeks to provide 2nd point of fixation)
Alveolar fractures:
- Alveolar bone encases the teeth
- Rare to have a pure alveolar fracture
- Usually have dentoalveolar fractures
- MMF or wire composite splinting (Essing wire; Figure 9)

Figure 14. Condylar fracture with dislocation.
Figure 15. (Image removed at request of copyright holder.) Demonstrating an open fracture without a tension band as described by Champy.
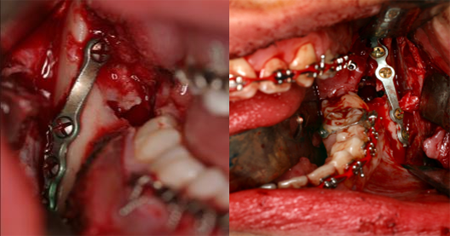
Figure 16. Champy technique. A single, noncompression miniplate is bent and placed on the superior border of the mandible angle.
Surgical approach to exposure of fracture site
- Use of existing lacerations
- Intraoral
- Labial sulcus incision: symphysis/parasymphysis and mandibular body/angle fractures; make incision on the lip vestibular mucosa, then to the bone.
- Vestibular incision: body, angle, and ramus fractures. The ramus and subcondylar region can be exposed by stripping and elevating the buccinator muscle and temporalis tendon at the coronoid process.
- Intraoral approach to the condyle:
- Extend vestibular incision superiorly ascending the ramus.
- External approaches
- Submental/submandibular approach (Risdon, J Am Dent Assoc 1934; Ellis, Surg Appr to Facial Skeleton, 2005)
- Described by Risdon
- Incision made 2 cm below the angle of the mandible in a natural skin crease
- Dissection carried down through the platysma to the superficial layer of the deep cervical fascia; Remember: The marginal mandibular nerve is deep to this layer.
- Dissect through the deep cervical fascia to the mandibular bone.
- Retromandibular approach (Figure 17)
- Described by Hinds in 1958 (Hinds J Oral Surg [Chic] 1958; Hinds Oral Surg Oral Med Oral Pathol 1967)
- Make a vertical incision 0.5 cm below the lobe of the ear; continue the incision inferiorly for 3 cm. Ensure that the incision is posterior to the posterior mandibular border.
- Extend the incision to the level of the angle.
- Dissect through platysma/SMAS/parotid capsule. Note: some surgeons use a nerve stimulator for this approach as the marginal mandibular and cervical branches of the facial nerve could be encountered (Figure 17).
- The retromandibular vein runs vertically in the parotid and should be identified and ligated or retracted to gain access to the lateral mandible.
- Elevate the muscle off the lateral surface of the mandible to get access to the ramus and subcondylar region of the mandible.
- Preauricular approach
- Use for exposure of the TMJ
- Make incision in preauricular fold 2–3 cm in length
- Dissection is carried along the lateral perichondrium of the tragal cartilage.
- Incision is made through the outer layer of the temporalis fascia from the zygomatic arch.
- The joint capsule is then exposed (violation of the joint capsule should be avoided).
- Facelift approach
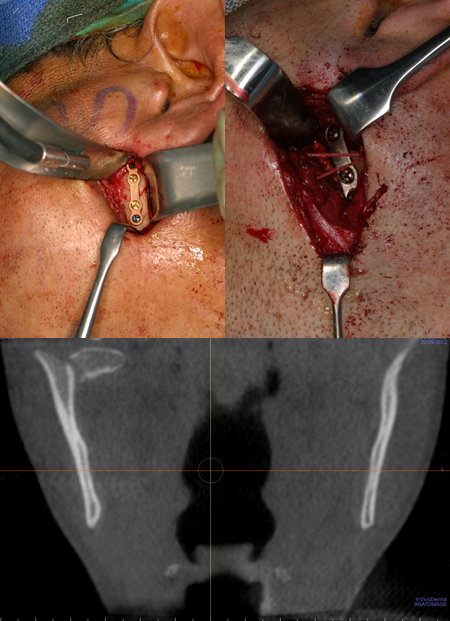
Figure 17. Upper left: retromandibular approach to reduction of condylar fracture. Upper right: facial nerve encountered during approach. Bottom: Coronal CT scan of fracture.
Bone healing
- Primary
- No callus
- Haversian remodeling (by contact; no gap across fracture)
- Lamellar bone deposition (if small gap exists)
- Requires rigid fixation with minimal gaps
- Secondary
- Callus forms
- Occurs when mobility around fracture site
- Subperiosteal hematoma forms granulation tissue thin bone forms by membranous ossification hyaline cartilage replaced by woven bone remodels to lamellar bone
Other management considerations
- How are fractures treated in the edentulous patient?
- Biomechanics are different because decreased bone height leads to decreased buttressing (alters plate selection)
- More significant effect of muscular pull (digastric muscles)
- Inferior alveolar artery absent in 40% of patients (Bradley, Int J Oral Surg 1981)
- Periosteal blood supply disturbed by stripping
- 20% nonunion despite type of treatment
- Concurrent medical conditions that delay healing
- Delayed healing with age
- Classification of the edentulous mandible (relates to vertical height of the thinnest portion of mandible):
- Class I: 16–20 mm
- Class II: 11–15 mm
- Class III: < 10 mm
- Closed Reduction
- Circummandibular wires fixated to the pyriform rim and circumzygomatic wires with patient’s dentures/Gunning splints
- Requires IMF (6–8 weeks)
- Class I edentulous fractures
- External Fixation
- With/without use of IMF
- Avoids periosteal stripping
- For comminuted edentulous fractures
- When an open procedure is contraindicated
- Larger diameter screw (4 mm) for fixation
- Open Reduction
- When fracture not healed from other treatments
- IMF contraindicated
- Splints/dentures unavailable
- Mandible is too atrophic for success with closed reduction
- Rigid fixation technique
- Can use in conjunction with bone graft if severely atrophic mandible (Ellis JOMS 2008)
- Use load-bearing plates with multiple fixation points and bicortical screws
- Lowest complication rate with extra-oral approach with rigid fixation, especially for class III atrophic mandibles (Bruce, JOMS 1993; Luhr, JOMS 1996)
- Mandibular fractures in children
- Rare (0.31/100,000 incidence in children younger than 15)
- Nonunion/fibrous union rare due to osteogenic potential
- Interference with growth potential
- Fixation in deciduous/mixed dentition
- Unerupted teeth (presence of tooth buds in the lower portion of mandible affect hardware placement and can be injured with open reduction)
- Arch bar application is more difficult due to short and less bulbous deciduous teeth
- Due to rapid healing, most treated with closed reduction (arch bars), soft diet
- Open reduction for severely displaced, unfavorable fractures, delayed treatment (> 7 days), airway/medical issues.
- Minimal risk for growth disturbance for fractures of the mandibular body, angle, symphysis, or ramus. Most growth disturbance from intracapsular condylar fractures.
- Most advocated closed reduction/MMF and early mobilization for condylar fractures in children.
- Importance of achieving immobilization
- Allows for osseous union (primary bone healing)
- Restoration of occlusion (bite), mandibular anatomy, and jaw function
- Indications for pulling teeth during fracture fixation
- Longitudinal fracture involving tooth root
- Dislocation/subluxation of tooth from socket
- Presence of periapical infection
- Infected fracture line
- Acute Pericoronitis, periodontal disease, cyst, decayed tooth
- Removal of the third molar tends to destabilize angle fractures and should be avoided
- If presence of tooth prevents adequate reduction of the fracture
Preventing and managing treatment complications
(Meaders, JOMS 1998)
- Mobility at the fracture site (nonunion or fibrous union)
- Nonunion can be determined by pain or irregular mobility at the fracture site.
- Occurs in 3–5 % of fractures overall
- Most common causes: poor reduction, immobilization, infection, periosteal stripping, traumatic ischemia
- Malocclusion
- Soft tissue deformity
- Infection
- Chronic pain
- Neurosensory/neuromotor disturbances (CN7 most worrisome; V3 most common)
- Tooth loss or devitalization
- Inability to chew hard food
- Need for alternative or additional treatment
- Complications, such as infection, nonunion, and extrusion of the implant are seen more commonly in patients who abuse tobacco and alcohol (Furr, Laryngoscope 2006; Biller, Laryngoscope 2005)
Trauma/fracture-related complications
(Mulligan, Plast Reconstr Surg 2010)
- Cervical spine injury
- 5–8% in isolated facial fractures
- 7–11% if 2 or more facial fractures are present
- Stabilize cervical spine at presentation with C-collar
Historical perspective
- Edwin Smith Papyrus (1650 BCE) described the history, physical examination, and diagnosis of mandibular fractures.
- Hippocrates described monomaxillary dental fixation and binding.
- Sulicetti (1492) described tying the teeth of the injured jaw to the uninjured jaw for fixation.
- Schede (1888) described using a bone plate of steel with 4 screws for fixation
- Luhr (1960) developed mandibular compression plates
- Michelet/Champy (1970) developed small bendable noncompression plates
References and additional resources
- Abubaker AO, Rollert MK. Postoperative antibiotic prophylaxis in mandibular fractures: A preliminary randomized, double-blind, and placebo controlled clinical study. J Oral Maxillofac Surg. Dec 2001; 59(12): 1415-1419.
- Andreasen JO, Jensen SS, Schwartz O, et al. A systematic review of prophylactic antibiotics in the treatment of maxillofacial fractures. J Oral Maxillofac Surg. 2006; 64: 1664-8.
- Barker DA, Oo KK, Allak A, et al. Timing for repair of mandible fractures. Laryngoscope. 2011; 121: 1160-3.
- Biller, Jason A., et al. “Complications and the time to repair of mandible fractures.” The Laryngoscope. 115.5 (2005): 769-772.
- Bradley JC. The clinical significant of age changes in the vascular supply to the mandible. Int J Oral Surf. 1981; 10 (Suppl 1): 71-6.
- Bruce RA, Ellis E 3rd. The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993; 51 (8): 904-11.
- De Riu G, Gamba U, Anghinoni M, Sesenna E. A comparison of open and closed treatment of condylar fractures: A change in philosophy. Int J Oral Maxillofac Surg. Oct 2001;30(5):384-389.
- Ellis E 3rd, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. Mar 2008;66(3):421-435.
- Furr, Andrea Marie, John M. Schweinfurth, and Warren L. May. “Factors Associated with Long‐Term Complications after Repair of Mandibular Fractures.” The Laryngoscope. 116.3 (2006): 427-430.
- Gutta R, Tracy K, Johnson C, James LE, Krishnan DG et al. Outcomes of mandible fracture treatment at an academic tertiary hospital: a 5-year analysis. J Oral Maxillofac Surg. 2014 Mar; 72 (3): 550-8.
- Haug et al. An epidemiologic survey of facial fractures and concomitant injuries. JOMS. 1990; 48.
- Hinds EC. Correction of prognathism by subcondylar osteotomy. J Oral Surg (Chic) . May 1958;16(3):209-214.
- Hinds EC, Girotti WJ. Vertical subcondylar osteotomy: A reappraisal. Oral Surg Oral Med Oral Pathol. Aug 1967;24(2):164-170.
- Kellman RM, Cienfuegos R. Endoscopic approaches to subcondylar fractures of the mandible. Facial Plast Surg. Feb 2009; 25(1):23 -28.
- King, Robert E., Joseph M. Scianna, and Guy J. Petruzzelli. “Mandible fracture patterns: a suburban trauma center experience.” Am J Otolaryngol. 25.5 (2004): 301-307.
- Kubilius R, Keizeris T. Epidemiology of mandibular fractures treated at Kaunas University of Medicine Hospital, Lithuania. Stomatologija 2009; 11 (3): 73–6.
- Lee C, Forrest CR. Endoscopic facial fracture management. Techniques. Chapter 68 in: Mathes SJ. Plastic Surgery. Vol. 3. 2nd ed. Philadelphia, PA: Saunders Elsevier; 2006:463-4579.
- Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996; 54(3): 250-4.
- Martin M, Lee C. Endoscopic mandibular condyle fracture repair. Atlas Oral Maxillofac Surg Clin North Am . Sep 2003;11(2):169-178.
- Meaders RA, Sullivan SM. The development and use of a computerized database for the evaluation of facial fractures incorporating aspects of the AAOMS parameters of Care. J Oral Maxillofac Surg. 1998; 56(8): 924-29.
- Miles BA, Potter JK, Ellis E 3rd. The efficacy of postoperative antibiotic regimens in the open treatment of mandibular fractures: A prospective randomized trial. J Oral Maxillofac Surg. Apr 2006; 64(4): 576-582.
- Mulligan RP, Mahabir RC. The prevalence of cervical spine injury, head injury, or both with isolated and multiple craniomaxillofacial fractures. Plast Reconstr Surg. 2010; 126: 1647.
- Nasser, M., Pandis, N., Fleming, P. S., Fedorowicz, Z., Ellis, E., & Ali, K. (2013). Interventions for the management of mandibular fractures. status and date: New search for studies and content updated (no change to conclusions), published in, (7).
- Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003; 61 (6): 713–8.
- Palmieri C, Ellis E 3rd, Throckmorton G. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg. Jul 1999;57(7):764-75; discussion 775-776.
- Risdon F. Ankylosis of the temporomandibular joint. J Am Dent Assoc. 1934; 21:1933.
- Ellis 3rd E, Zide MF. Transfacial approaches to the mandible. Section 5 in: Ellis 3rd E, Zide MF. Surgical Approaches to the Facial Skeleton. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:151-189.
- Schmeizeisen, Cienfuegos-Monroy, Schon R et al. Patient benefit from endoscopically assisted fixation of condylar neck fractures-a randomized controlled trial. J Oral Maxillofac Surg. 2009; 67 (1): 147-58.
- Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983; 41(2): 89-98.
