Medial Orbital Wall Fractures
Updated July 2024
Establishing the diagnosis
Etiology
- Blunt trauma is the most common cause of medial wall fractures.
- Penetrating trauma includes knife wounds, gunshot, blast injuries.
- May also be iatrogenic surgical injury.
- Nasoethmoid fractures can cause posterior displacement and bowing of the medial orbital wall.
- In many cases, medial orbital wall fractures are considered in association with other injuries.
- As an extension of an orbital floor fracture
- In association with a nasoethmoid complex fracture that requires reduction and fixation and correction of telecanthus
- In association with Lefort III fractures
Epidemiology
- Trauma is the primary etiology, so medial wall fractures tend to occur most commonly in young males.
- They are seen frequently in motor vehicle accidents and in the elderly struck around the eye when falling.
History
- The event is recorded, including seemingly incidental trauma in children.
- Periorbital swelling can be related to air forced into the orbit from nose blowing or sneezing (orbital emphysema).
- Leakage from the nose is carefully described and epistaxis is differentiated from cerebrospinal fluid rhinorrhea.
- Diplopia is most commonly horizontal, more commonly on adduction, caused by edema and ecchymosis in the medial rectus muscle, or on abduction related to muscle entrapment.
- Decreased vision can signal traumatic optic neuropathy.
- Infraorbital numbness can be caused by concurrent floor fracture.
Clinical features
- Periorbital edema, ecchymosis, and crepitus (subcutaneous emphysema)
- Direct injury to the eye, including subconjunctival hemorrhage
- Enophthalmos or proptosis
- Horizontal restriction of eye movement and diplopia
- In cases of iatrogenic medial orbital wall breach during endoscopic sinus surgery, suspect direct medial rectus and/or inferior oblique injury or transection, particularly in patients with moderate to large exotropia and adduction deficit (Huang, OPRS 2003; and Rene et al. Br J Ophthalmol 2001).
- Global limitation of eye movement can be due to concomitant orbital fractures or significant elevation of orbital pressure from edema, hemorrhage, or orbital emphysema.
- Telecanthus and evidence of a nasoethmoid fracture
- Rhinorrhea: Hemorrhagic or cerebrospinal fluid can be seen with associated basilar skull fractures.
- Decreased sensation, particularly in the V1 distribution
- Evidence of traumatic optic neuropathy
Testing
- On orbital imaging, the fracture is evident as disruption of contour along the medial wall of the orbit
- May have opacification of ethmoid sinus (Figure 1).
- There can be blood or air in the orbit.
- Rounding or tenting suggests soft tissue injury to the medial rectus muscle (Figure 2).
- Prolapse of the medial rectus might be evident, but entrapment of the medial rectus is rare.
- Unrelated sinus or nasal pathology, such as a polyp, can confuse the radiographic appearance.
- The status of the globe and optic nerve are carefully evaluated.
- Associated injuries and retained foreign bodies, risk of infection, need for soft tissue repair, etc., are all characterized.
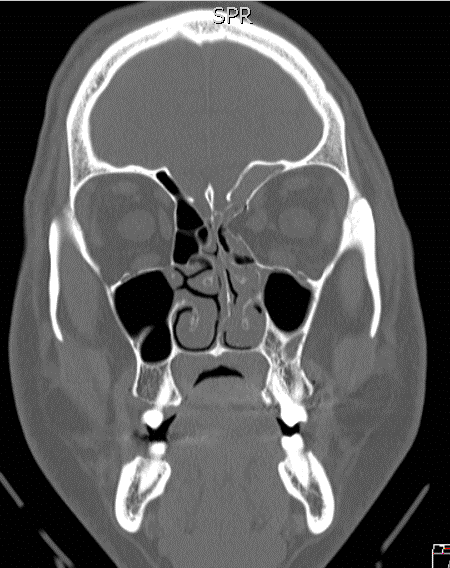
Figure 1. The fracture is evident as disruption of contour along the medial wall of the orbit with opacification of ethmoid sinus.
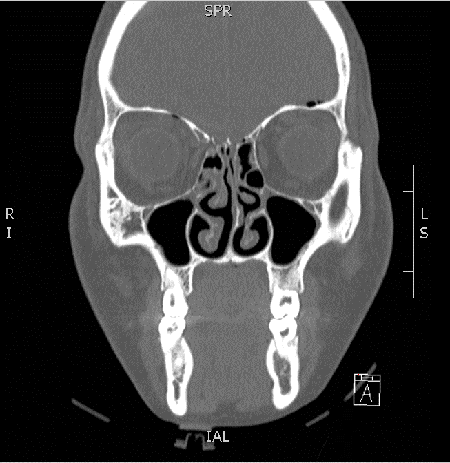
Figure 2. Rounding or tenting suggests soft tissue injury to the medial rectus muscle.
Differential diagnosis
Independent of the fracture, there might be trauma to the medial rectus muscle.
Blunt head trauma can also cause injury to the fourth or sixth cranial nerve.
Limitation of eye movement might be related to trauma to the inferior oblique muscle at its origin or in the muscle belly.
Patient management: treatment and follow-up
Observation
The decision on when to intervene is mostly dictated by the associated injuries and clinical signs.
With an isolated medial wall fracture, ecchymosis in the medial rectus muscle, rather than entrapment, is the more common cause of diplopia.
- Can cause horizontal diplopia in either adduction or abduction
- Observation is appropriate for a minimum of 7–14 days, awaiting spontaneous resolution.
- There is little published data on outcomes and management of horizontal motility deficits with pure medial blowout fracture.
- It is reasonable to treat with antibiotics (because soft tissues have prolapsed into the sinus) and corticosteroids (to unmask entrapment once the edema is reduced), but there are no published data to support the efficacy.
An isolated medial wall fracture can cause enophthalmos in the presence of substantial bony displacement.
- A period of observation allows for resolution of periorbital edema and more accurate assessment of possible enophthalmos.
- There are no specific criteria for predicting enophthalmos based on the radiographic appearance, both for a pure medial blowout fracture and for the contribution of a medial wall fracture in association with other injuries.
Observation might be necessary because of an associated ocular injury such as hyphema or a ruptured globe.
During the period of observation, it is appropriate to prescribe nasal decongestants and to have the patient to avoid nose blowing.
Surgery
Indications for repair
Vagal symptoms of nausea, vomiting, and bradycardia indicate incarceration and potentially ischemia.
- Requires urgent surgical release to prevent permanent damage
- Rare situation compared to that seen with orbital floor fracture
- Entrapment and abduction deficit as “white eye injury” is less common in the medial wall because the bone does not snap back and catch the soft tissues.
There may be restrictive abduction deficit due to soft tissue edema and/or scarring, even without absolute entrapment.
- Appropriately managed with exploration
- May need muscle surgery
The associated fractures usually dictate the need for surgical repair, but rarely the isolated medial wall fracture.
- Surgical repair does not need to be delayed.
- Large fracture likely to cause enophthalmos should be repaired before scarring potentially interferes with restoration
Approach
Transcaruncular: Visualization should be adequate for exploration of the defect, repositioning orbital contents, and placement of an implant across the defect.
- A secondary supporting implant can be inserted as a means of stabilizing the primary implant placed along the bony defect.
- The supporting implant is bent into a U-shape and inserted into the ethmoid sinus as support for the implant that lies over the defect (Kim, OPRS 2013).
Direct endoscopy through the transcaruncular incision can be helpful.
- In a study of 93 large, isolated, medial-wall fractures near the orbital apex approached by an endoscopic transcaruncular incision and repaired with 1.0-mm thick porous polyethylene implants placed over the edges of the fractures, which ranged in size from 16–30 mm vertically and 25–34 mm horizontally, there were 3 cases of residual diplopia on medial gaze from presumed paralysis of the medial rectus muscle and 1 case of postoperative orbital hemorrhage (Wu, Ophthalmology 2013).
Transantral or transnasal endoscopy can help visualize the posterior edge of the fracture, when dissecting soft tissue and inserting the implant, combined with the transorbital approach (Woog, Arch Ophthalmol 1998 & Shi, J Craniofac Surg 2012).
Incisions:
- Transcutaneous medial canthal tendon incision (Timoney, Ophthal Plast Reconstr Surg 2012)
- Medial eyelid crease incision can be adequate for access to superior medial wall fractures.
- Lynch incision or use of overlying traumatic facial laceration
- Transconjunctival with lateral canthotomy/cantholysis is often used when there is associated orbital floor fracture and more inferior medial wall fracture.
- Bicoronal incision is often used when other associated facial fractures are present (nasoethmoid or Lefort III).
Endoscopic endonasal approach alone has been described, but a rigid reconstruction of the medial wall defect is not performed, so late enophthalmos has been noted for larger fractures (Kim, Ann Plast Surg 2012).
The anterior and posterior ethmoid arteries are frequently visualized and may require cauterization or ligation.
The posterior edge of the implant should be shaved and tapered to protect against compressive optic neuropathy should there be posterior migration of the implant.
Biomedical glue can be used to fixate the implant against the bony edges.
Systemic corticosteroids and antibiotics should be prescribed postoperatively for 3–5 days to minimize the morbidity from postoperative edema.
Surgical goals
Careful release of entrapped tissue:
- Forced ductions at the start, during, and after placement of the implant with comparison to the opposite orbit to achieve equivalent globe motility by the end of the case
- Might require removal of bony fragments to fully release adherent or entrapped tissues
- May require enlargement of the fracture
Placement of implant to reproduce the anatomic position of the medial orbital wall:
- The implant margins should rest on secure bony ledges surrounding the defect tapering posteriorly to avoid abutting the optic nerve.
- Endoscopic endonasal visualization can be useful to ensure correct placement.
- Anterior implant fixation to the orbital rim with one screw is usually sufficient to avoid posterior implant migration.
- Many surgeons will not fixate a medial orbital wall implant due to difficulty in finding thick, stable bone anteriorly that will support a screw.
- Maintaining the correct alignment with respect to the orbital floor is critical to restoring normal orbital volume.
- Intraoperative CT is becoming more readily available to assess for proper implant placement and contour.
Preventing and managing treatment complications
Postoperative orbital hemorrhage
Perform urgent lateral canthotomy/cantholysis if compromising vision.
Remove implant; surgically drain if compromising vision.
Postoperative loss of vision
Treatment depends on etiology.
- Optic nerve trauma: Remove implant; consider corticosteroids.
- Orbital hemorrhage: See above.
Infection
Treat with appropriate antibiotics
Consider removal of implant
Implant extrusion
Remove/reposition/replace implant
Orbital Inflammation
Removal of the implantDamage to lacrimal drainage system or medial canthal ligament
Stay posterior to posterior lacrimal crest with transcaruncular approach
Repair medial canthal ligament
Dacryocystorhinostomy if damage is limited to the nasolacrimal sac and/or duct
Conjunctivodacryocystorhinostomy if damage involves the canaliculi
Persistent restriction
Treatment depends on etiology
Follow-up imaging can help confirm implant position and differentiate continued tissue entrapment from intrinsic muscle dysfunction.
Forced duction and forced generation testing can also be used to assess whether there is continued entrapment of tissue versus a neurogenic or myogenic etiology.
Enophthalmos
In a study of 23 patients who underwent repair of isolated medial wall fractures evaluated postoperatively by CT scan, persistent asymmetry of the orbits by 1–2 cm3 produced relatively little enophthalmos with a mean follow-up of 8 months (Lee, Arch Ophthalmol 2009).
Consider implant replacement or augmentation of orbital volume.
Disease-related complications
- Orbital emphysema and/or hemorrhage with potential for increasing intraorbital pressure and diminishing optic nerve and/or globe perfusion
- Permanent diplopia
- Enophthalmos and narrowed palpebral fissure
- Orbital cellulitis
Patient instructions
Avoid nose blowing
Avoid swimming or scuba diving or other activities associated with substantial pressure changes for 6–8 weeks
History
- Blow-out fracture of the medial wall was first described in isolated case reports in the 1960s, when they were recognized clinically (Fischbein, Arch Ophthalmol 1969).
- In 1971, blow-out fractures were studied in a larger series by Dodick, et al. (Arch Ophthalmol 1971), when they were diagnosed by hypocycloidal tomography (a precursor to CT scan in which the X-ray tube was rotated in a clover leaf pattern).
- “[If] it is postulated that the orbital floor (0.5 to 1 mm thin) is unable to withstand the raised intraorbital pressure and consequently fractures into the maxillary antrum…why do not the lamina papyracea of the ethmoid or the thin orbital medial wall fracture more frequently?”
- In 22 cases of blowout fracture of the orbit studied by hypocycloidal tomography, 8 had a concomitant medial wall fracture.
References and additional resources
- Blaydon SM, Shore JW, Neuhaus RW. Chapter 7: Medial Orbital Wall Fractures (pp. 103-117) In Evaluation and Treatment of Orbital Fractures a Multidisciplinary Approach. Ed. David Holck and John Ng. Philadelphia, Pennsylvania: Elsevier Saunders, 2006.
- Dodick JM et al. Concomitant medial wall fracture and blowout fracture of the orbit. Arch Ophthalmol 85:273, 1971
- Fischbein FI, Lesko WS, Blowout fracture of the medial orbital wall. Arch Ophthalmol 81:162, 1969
- Huang CM et al. Medial rectus muscle injuries associated with functional endoscopic sinus surgery: characterization and management. OPRS 19:25-37, 2003
- Jensen AD, Hodgson NM, Parikh R, Eberhart CG, Henderson AD, Fu R. Orbital inflammation in the setting of a nylon foil implant. Orbit. 2022 Dec;41(6):759-762.
- Kim CY et al. Supporting implant technique for repairing large medial orbital wall fractures. Ophthal Plast Reconstr Surg. 2013 May-Jun;29(3):170-4.
- Kim K et al. Endoscopic transnasal approach for the treatment of isolated medial orbital blow-out fractures: a prospective study of preoperative and postoperative orbital volume change. Ann Plast Surg. 2012 Feb;68(2):161-5
- Lee et al. Combined transconjunctival and transcaruncular approach for repair of large medial orbital wall fractures. Arch Ophthalmol. 2009 Mar;127(3):291-6.
- Rene C et al. Major orbital complications of endoscopic sinus surgery. Br J Ophthalmol 85:598-603, 2001.
- Shi W et al. Combination of transorbital and endoscopic transnasal approaches to repair orbital medial wall and floor fractures. J Craniofac Surg. 2012 Jan;23(1):71-4.
- Timoney PJ et al. Transcutaneous medial canthal tendon incision to the medial orbit. Ophthal Plast Reconstr Surg. 2012 Mar-Apr;28(2):140-4.
- Woog J et al. Paranasal sinus endoscopy and orbital fracture repair. Arch Ophthalmol 116:688, 1998.
- Wu W et al. Endoscopic transcaruncular repair of large medial orbital wall fractures near the orbital apex. Ophthalmology. 2013 Feb;120(2):404-9.
