Merkel Cell Carcinoma
Updated May 2024
Establishing the diagnosis
Etiology
- The Merkel cell is a nondendritic, nonkeratinocytic, clear epithelial cell usually located in or near the basal layer of the epidermis and associated with nerve terminations.
- The Merkel cell is believed to be a mechanoreceptor that mediates the sense of touch.
- There is increasing evidence that the Merkel cell polyomavirus (MCPyV) has a role in the development of Merkel cell carcinoma (MCC), making MCPyV the first polyomavirus to be clearly associated with human cancer (Borchert, J Virol 2014).
- Merkel cell polyomavirus (MCPyV), is integrated in about 90% of Merkel cell carcinomas and seems to interfere with tumor suppressor pathways (Borchert, J Virol 2014).
- The cell of origin in MCC might be the Pro/Pre B cell rather than the Merkel cell (Zur Hausen, Cancer Res 2013).
Epidemiology
- Incidence is estimated to be about 0.45 cases per 100,000 population
- 50% occur in the head and neck region, 40% in the extremities, and 10% in the buttocks/trunk
- 2.5–10% of Merkel cell carcinoma occurs in the eyelid.
- A review of eyelid MCC in the literature demonstrated 64% to be female, despite an overall male predominence in MCC in general (Surv Ophthalmol 2019:64:659).
History
- Rapidly expanding mass
- Symptoms usually less than 6 months
- Often confused with benign inflammation such as chalazion
Clinical features
- Purple-red swelling of the skin
- Mass effect
- AEIOU mnemonic: Asymptomatic, Expanding rapidly, Immune suppression, Older than 50, Ultra-violet exposed site on a person with fair skin (Heath, J Am Acad Dermatol 2008)
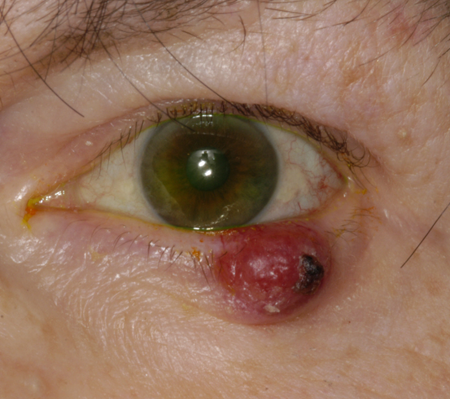
Figure 1. Merkel cell carcinoma. Image courtesy Raymond Cho, MD.

Figure 2. Merkel cell carcinoma. Image courtesy Gregory J. Griepentrog, MD.

Figure 3. Merkel cell carcinoma. Image courtesy Michael J. Hawes, MD.
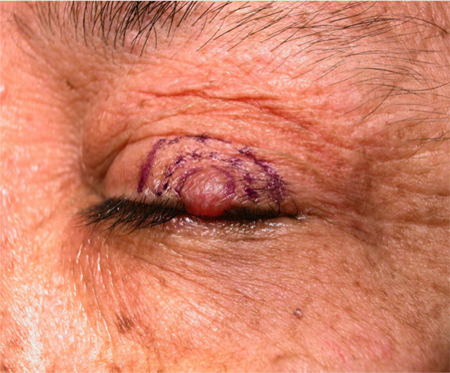
Figure 4. Merkel cell carcinoma. Image courtesy Mark. J. Lucarelli, MD.
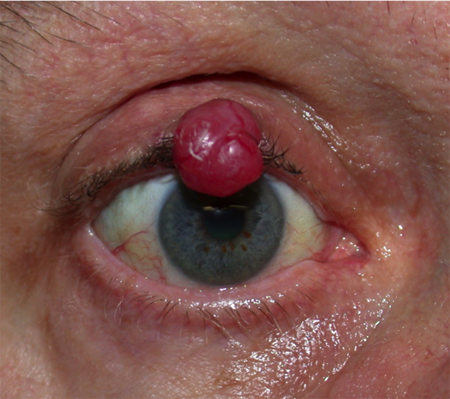
Figure 5. Merkel cell carcinoma. Image courtesy Navdeep Nijhawan, MD.
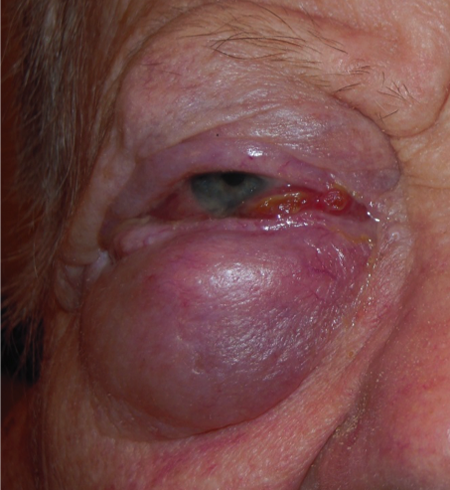
Figure 6. Merkel cell carcinoma. Image courtesy Rona Z. Silkiss, MD, FACS.
Histopathology
- Small cell carcinoma composed of granular cells with scant cytoplasm, large oval nuclei, prominent nucleoli, salt and pepper dense chromatin, and many mitoses
- Immunohistochemistry positive for low molecular weight cytokeratin markers (cytokeratin 20), neuroendocrine markers (neuron-specific enolase, chromogranin, synaptophysin), and neurofilament protein
- Negative for S-100 protein and human melanoma markers (helps differentiate it from amelanotic melanoma), vimentin, leucocyte common antigen, HMB-45, TTF-1, and high molecular weight cytokeratins
- The presence of more than 50% of Ki67+ (a marker for replication) cells is a negative prognostic indicator.
- High expression of Bcl-2 and MIB-1 also indicate a bad prognosis (Missotten, Ophthalmology 2008).
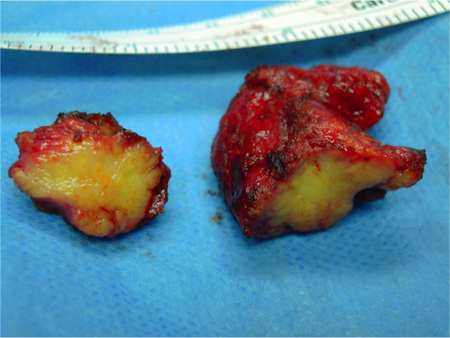
Figure 7. Merkel cell carcinoma gross appearance. Image courtesy Rona Z. Silkiss, MD, FACS.
Clinical Staging
- In a retrospective case series of 21 primary eyelid Merkel cell carcinomas from 5 tertiary care centers in the United Kingdom and Australia staged according to the American Joint Committee on Cancer, 7th Edition (Herbert, JAMA Ophthalmol 2014).
- There were 12 T2 lesions, tumor size 2–5 cm.
- There were 7 T3 lesions, tumor size > 5 cm.
- Distant metastases were detected in 19% and 2 patients died of metastatic disease.
- In 18 primary eyelid Merkel cell carcinomas (Sniegowski, OPRS 2014).
- Four patients (22%) had lymph node metastasis at presentation, the strongest predictor of reduced disease free survival and risk of distant metastases.
- Two patients died of metastatic disease.
- Patients who had T2 (eyelid carcinoma T category) or more extensive tumors had significantly worse disease free survival than patients with less than T2 tumors.
Risk factors
- Paradoxically believed related to sun exposure, yet it occurs more frequently on the upper eyelid.
- In a study of 21 MCCs, 17 (81%) developed in the upper lid.
- Age (Greater than 50 years)
- Immune suppression (organ transplant, AIDS, chronic lymphocytic leukemia)
Differential diagnosis
- Chalazion
- Basal cell carcinoma
- Vascular lesion
- Kaposi’s sarcoma
- Malignant lymphoma of the skin
- Metastasis
Patient management: treatment and follow-up
Natural history
- Locoregional recurrence rates are 30%-60% and up to one third of patients develop distant metastasis.
- Estimated mortality rate for all patients with MCC is 25-35%.
- In a review of 14 primary eyelid Merkel cell carcinomas with average follow-up of 33 months, only 3 patients received treatment beyond wide surgical excision (Peters, Ophthalmology 2001).
- In that series 21% of the patients treated with primary excision developed local recurrence.
- Regional spread to lymph nodes.
- The most common sites of systemic metastasis are bone, brain, liver, and lung.
- Complete spontaneous remission (CSR) of nonpalpebral Merkel cell carcinoma has been described in a number of cases (Connolly, Dermatol Surg 2000).
- The process of CSR is swift and dramatic and includes regression of metastases, but it is rare.
Medical therapy
- Chemotherapy for Merkel cell carcinoma is used for systemic dissemination, including cisplatin, cyclophosphamide, doxorubicin, vincristine, and 5-fluorouracil.
- Merkel cell tumors often express PD-1 ligand 1 (PD-1).
- Merkel cell polyomavirus–specific T cells express PD-1.
- Avelumab is an anti-PD1 monoclonal antibody, approved by the FDA as targeted therapy for merkel cell carcinoma.
Radiation
- For nonocular Merkel cell carcinoma, adjuvant radiotherapy at a dose of 50 Gray is reported to decrease the rate of local recurrence (Plunkett, Expert Rev Anticancer Ther 2001).
- For the eyelid, adjuvant radiotherapy is institution dependent (Missotten, Ophthalmology 2008; Sniegowski, OPRS 2014).
- In a UCLA study of 87 MCC head and neck tumors, identified between 2001-2016, adjuvant radiation therapy was associated with improved overall survival when early cases were treated (Han, Laryngoscope 2018).
- Logically, adjuvant radiotherapy would not improve overall survival once the tumor cells have the capacity to spread beyond the primary site
- In the eyelid, local cure can be expected with wide surgical excision of well defined disease
- Post-operative radioathy can be recommended if there is concern that effective surgical margins were not achieved.
- Elective radiotherapy to draining lymph nodes may also be a reasonable option.
Surgery
- Aggressive surgical approach is needed for Merkel cell carcinoma of the eyelid.
- Wide local excision is performed with frozen section evaluation.
- 5-mm margins for eyelid lesions are recommended.
- Sentinel node biopsy can be beneficial (Connolly, Dermatol Surg 2000). Some authors recommend sentinel lymph node biopsy for all Merkel cell carcinomas. (Schwartz, J Clin Oncol 2011).
- Greater likelihood of positive results in SLN with increased tumor size, higher tumor thickness, high mitotic rate, and infiltrative growth pattern. (Schwartz, J Clin Oncol 2011).
- Regional lymph node metastases are treated with neck dissection and/or radiotherapy.
Prognosis
- Prognostic factors influencing mortality include size (> 2 cm diameter have poor prognosis) and gender (higher mortality in men) (Missotten, Ophthalmology 2008).
- Metastastic disease is typically aggressive and rapidly fatal.
- In a twenty year retrospective analysis (1994-2014) at the Medical University of Vienna 23 of 54 (43%) MCC patients (all sites) were found to have progressive disease defined as relapse within one year: there was a 96% disease related mortality among these patients (Fochtmann, Clin Otolaryngol, 2018).
- Median overall survival was 15 months, median disease-free survival was 8 months and median time to disease progression was 5 months.
Complications of treatment
Related to the extent of tumor involvement, the need for surgical excision and effects of radiotherapy when used
Historical perspective
Merkel cell carcinoma bears the cell that Friedrich Merkel identified in 1875, was first described in the eyelid in 1983 (Lamping, Ophthalmology 1983).
References and additional resources
- Barrett RV, Meyer DR. Eyelid and periocular cutaneous Merkel cell carcinoma (aka. neuroendocine or trabecular carcinoma). Int Ophthalmol Clin 2009;49:63-75.
- Borchert S. High-affinity Rb binding, p53 inhibition, subcellular localization, and transformation by wild-type or tumor-derived shortened Merkel cell polyomavirus large T antigens. J Virol. 2014; 88:3144.
- Fochtmann-Frana A, Haymerle G, Loewe R, et al. Incurable, progressive Merkel cell carcinoma: A single-institution study of 54 cases. Clin Otolaryngol 2018; 43:678-682.
- Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol 2008;58:375-381.
- Connelly TJ, Cribier B, Brown TJ, Yanguas I. Complete spontaneous regression of Merkel cell carcinoma: a review of the 10 reported cases. Dermatol Surg. 2000; 26:853.
- Herbert HM, Sun MT, Selva D, et al. Merkel cell carcinoma of the eyelid: management and prognosis. JAMA Ophthalmol. 2014; 132:197.
- Han AY, Patel PB, Anderson M, et al. Adjuvant radiation therapy improves patient survival in early stage merkel cell carcinoma: A 15-year single-institution study. Laryngoscope 128:1862-1866, 2018.
- Lamping K, Fischer MJ, Vareska G, et al. A Merkel cell tumor of the eyelid. Ophthalmology. 1983; 90:1399.
- Merkel F. Tastzellen und Tastkörperchen bei den Hausthieren und beim Menschen. Arch Mikrosk Anat. 1875; 11:636.
- Missotten GS, de Wolff-Rouendaal D, de Keizer RJW: Merkel cell carcinoma of the eyelid: review of the literature and report of patients with Merkel cell carcinoma showing spontaneous regression. Ophthalmology. 2008; 115:195.
- North VS, Habib LA, Yoon MK. Merkel cell carcinoma of the eyelid: A review. Surv Ophthalmol. 2019 Sep-Oct;64(5):659-667. doi: 10.1016/j.survophthal.2019.03.002. Epub 2019 Mar 11. PMID: 30871952.
- Peters GP, Meyer DR, Shields JA, et al. Management and prognosis of Merkel cell carcinoma of the eyelid. Ophthalmology. 2001; 108:1575.
- Plunkett TA, Subrumanian R, Leslie MD, Harper PG. Management of Merkel cell carcinoma. Expert Rev Anticancer Ther. 2001; 1:441.
- Searl SS, Boynton JR, Markowitch W, diSant’Agnese A. Malignant Merkel cell neoplasm of the eyelid. Arch Ophthalmol. 1984; 102:907.
- Schwartz JL, Griffith KA, Lowe L, et al. Features predicting sentinel lymph node positivity in Merkel cell carcinomaa. J Clin Oncol 2011;29:1036-41.
- Sniegowski MC. Correlation of American Joint Committee on Cancer T category for eyelid carcinoma with outcomes in patients with periocular Merkel cell carcinoma. Ophthal Plast Reconstr Surg. 2014 Nov-Dec;30(6):480-5.
- Zeitouni NC, Cheney RT, Delacure MD. Lymphoscintigraphy, sentinel lymph node biopsy, and Mohs micrographic surgery in the treatment of Merkel cell carcinoma. Dermatol Surg. 2000; 26:12.
- Zur Hausen A. Early B-cell differentiation in Merkel cell carcinomas: clues to cellular ancestry. Cancer Res. 2013; 73:4982.
