Metastatic Tumors of the Orbit
Updated July 2024
Establishing the diagnosis
Etiology
Any solid tumor in the body that can metastasize via the hematogenous route can metastasize to the orbit.
This definition therefore excludes hematopoietic diseases and systemic lymphoma, as well as direct extension from the skin, eye, intracranial cavity and brain, paranasal sinuses, nasopharynx, and mandible.
Epidemiology
- Adult orbital metastases
- The most common ocular metastases are to the choroid.
- Metastases to the globe are about 8 times more common than to the extraocular orbit (Char, Br J Ophthalmol 1997).
- About 0.7 to 12% systemic cancers metastasize to the orbit (Shields, OPRS 2001; Font, AFIP 2006), of which breast carcinoma accounts for 50% (Shields, OPRS 2001).
- About 47%–91% of orbital metastases are accompanied by metastases in other sites (Ahmad, Curr Opin Ophth 2007).
- By some accounts, orbital metastases might be the second most common form of orbital cancer seen in the adult population after lymphoma (Font, AFIP 2006).
- Orbital metastases constitute 3% of all orbital diseases and 10% of orbital neoplasms in most series.
- Mean interval between diagnosis of primary tumor and the first orbital symptoms has been as long as 60 months.
- About 20% of metastatic tumors to the orbit were the first sign of cancer, and in 10%, the primary site could not be demonstrated (Goldberg, Surv Ophthal 1990).
- More than 90% of orbital metastases are unilateral (Shields, OPRS 2001); in other words, less than 10% have bilateral metastases.
- As cancer patients survive longer, the incidence of orbital metastasis is expected to rise.
- Pediatric orbital metastases
- In children, metastases to the orbit occur more frequently than to the globe (in contrast to adults).
- Neuroblastoma and Ewing’s sarcoma are the most common sources of metastatic disease to the orbit (Albert, 2008) in children.
- Medulloblastoma and Wilms’ tumor metastasize to the orbit less frequently than neuroblastoma and Ewing’s sarcoma (Fratkin, JAMA 1977).
- Orbital metastasis is the initial sign of abdominal neuroblastoma in 3%–4% of patients (Lau, Neuro-ophthal 2004).
- The most common site of primary tumor is the adrenal gland for patients with orbital involvement (Albert, 2008).
- Most cases (90%) occur before 5 years of age, and the prognosis is best in children younger than 1 year of age.
History
- Adults
- A history of enlarging mass, proptosis, diplopia, and pain, usually in a patient with a known history of cancer
- Compared to primary tumors of the orbit, metastatic tumors most commonly present with diplopia (Font, AFIP 2006).
- Gaze-evoked amaurosis has been reported with metastatic breast tumors (Patel, OPRS 2013).
- Rarely, metastatic lesions are found incidentally on imaging—in contrast to benign tumors, where incidental findings are more common.
- Children
- Neuroblastoma commonly presents as rapidly expanding exophthalmos with eyelid ecchymoses (Figure 1).

Figure 1. Bilateral metastatic neuroblastoma.
Clinical features
- Adult orbital metastases
- Rapid onset of symptoms, progressive over weeks or months
- Diplopia: extraocular muscle infiltration is common due to the high blood flow
- Blepharoptosis: from levator palpebrae superioris infiltration or compression
- Proptosis: mass effect
- Edema: from compression of venous outflow
- Chemosis: from compression of venous outflow
- Enophthalmos: associated with sclerotic tumors such as scirrhous breast carcinoma and gastric carcinoma (BCSC orbit)
- Imaging
- Lytic bony lesions can be seen on CT scans
- Breast carcinoma and malignant melanoma have a strong tendency to metastasize to orbital fat and extraocular muscles, while prostate and thyroid carcinomas have a predilection for bone (Figure 2)
- Lateral and superior orbit are the most commonly affected quadrants (Valenzuela, Orbit 2009)
- Metastatic melanoma might have left-sided preponderance, possibly due to direct branching of the left internal carotid from the aortic arch (Figure 3).
- Pediatric orbital metastases
- Metastatic neuroblastoma
- Frequently bilateral, with involvement of the temporal orbit with a lytic bone lesion
- 75% of children with neuroblastoma have proptosis or ecchymoses
- Can rarely cause bilateral blindness from intracranial compression of the optic nerves
- Can also be associated with paraneoplastic signs of opsoclonus and myoclonus
- Metastatic Ewing’s sarcoma
- Occurs in the second decade with sudden onset of proptosis due to hemorrhagic metastasis originating from bone
- Most commonly unilateral

Figure 2. T1-weighted MRI of metastatic breast carcinoma infiltrating the right orbital fat (Patel, OPRS 2013).
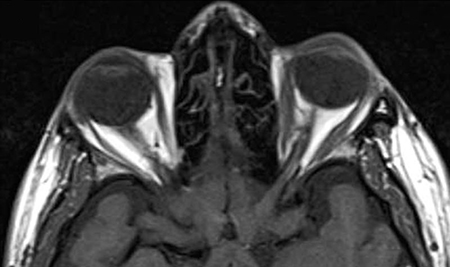
Figure 3. Metastatic cutaneous melanoma appearing as a discrete left orbital ovoid homogeneous mass with intense rim enhancement (Greene, OPRS 2014).
Testing
General review of systems, including weight loss, fatigue, or other systemic questions, should be elicited with referral to the primary physician or oncologist for further workup, as appropriate.
Initial imaging studies might include CT or MRI of the orbit, which allows for localization of the tumor within the orbit and any bony changes.
MRI has not been found to be superior to CT to establish the diagnosis of metastasis (Char, Br J Ophthalmol 1997), although modern techniques might improve MRI yield.
If there is no previous known history of cancer, a total body positron emission tomography (PET) scan or computed tomography (CT) of chest, abdomen, and pelvis as well as mammography and colonoscopy might also be indicated to look for a primary cancer.
Elevated serum levels of carcinoembryonic antigen (CEA) might suggest a metastatic process.
With carcinoid tumor, functioning metastases can be detected by the presence of elevated urinary 5-HIAA (Mehta, Ophthalmology 2006).
Risk factors
About 75% of patients have a history of known primary tumor, but in 20%–25%, the orbital metastasis is the presenting sign of cancer (Goldberg, Surv Ophthal 1990).
Most common primary sites are breast in women, lung and prostate in men, followed by cutaneous melanoma. However, incidences vary considerably by region (Wladis et al, Orbit, 2020).
Breast, thyroid, prostate, and carcinoid generally develop 3–5 years after initial diagnosis of the primary tumor.
Lung, renal, and gastrointestinal tumors are frequently diagnosed after the appearance of orbital metastatic signs and usually follow a fulminant course with short survival (Shields, OPRS 2001).
In Japan, ocular signs due to orbital metastases from hepatoma, neuroblastoma, and gastric cancer were likely to appear earlier than the signs of the primary lesion (Amemiya, Ophth Epidem 2002).
Histologic diagnosis
- The most common types of cancer leading to a metastatic orbital tumor in adults are
- Breast carcinoma
- Lung carcinoma
- Prostate carcinoma
- Renal cell carcinoma
- Cutaneous melanoma
- Sarcomas
- Carcinoid
- Thyroid carcinoma
- The most common types of cancer leading to a metastatic orbital tumor in children are
- Neuroblastoma
- Ewing’s sarcoma
- Wilms’ tumor
- Other rare reports of orbital metastases
- Cutaneous squamous cell carcinoma (Font, Cancer 1976)
- Hepatocellular carcinoma (Eldesouky, OPRS 2013)
- Choriocarcinoma (Dhrami-Gavazi, OPRS 2014)
- Merkel Cell Carcinoma (Johnson, Orbit 2013)
- Pleural solitary fibrous tumor (Patel, OPRS 2013)
- Distant rhabdomyosarcoma (Gupta, Orbit 2010)
- Retinoblastoma from contralateral eye (Mohan, Br J Ophthalmol 1990)
- Ovarian cancer (Malviya, Gynecol Oncol 1989)
- An incisional biopsy is the best way to establish the diagnosis.
- Fine needle aspiration can be used (Rootman, 2003, Magliozzi et al, Int J Ophthalmol, 2015 and Valenzuela et al, Orbit, 2009).
- Necessitates a cytopathologist to immediately process and read the specimen. If the tissue is inadequate to establish the diagnosis, open biopsy is required.
- Core biopsy can be used without image guidance for orbital tumors and has been successful in diagnosing 2 metastatic lesions (Yarovoy, Graefe’s 2013).
- Ultrasound-guided core-needle biopsy has been successful at achieving a final diagnosis in orbital tumors, including 2 adenocarcinomas (Orlandi, Euro Rad 2013).
- In the face of already established, widespread, metastatic cancer and known history of cancer, biopsy should be done only if it is likely to contribute to treatment options and decision making.
Differential diagnosis
- Primary tumors of the orbit
- Secondary tumors of the orbit—extension into the orbit from paranasal sinuses or brain (see Secondary orbital tumors)
- Nonspecific orbital inflammation
- IgG4-related orbital inflammation
- Wegener’s granulomatosis
- Thyroid orbitopathy
- Sarcoidosis
- Carotid-cavernous fistula
Patient management: treatment and follow-up
- CT or MRI of orbit
- Biopsy
- An open biopsy or a fine needle aspiration biopsy should be considered if the result would alter the management for the patient.
- Fine needle aspiration (FNA) is useful as a minimally invasive procedure if there is known systemic malignancy or if the tumor is preseptal or parabulbar (Tijl, Graefe’s 1992).
- If there is no history of a primary tumor or the presentation mimics orbital inflammation or other unknown orbital lesion, an open biopsy is preferred.
- If the metastasis is deeper in the orbit, an open biopsy might be safer than FNA (Tijl, Graefe’s 1992).
- Treatment
- Generally palliative
- Usually consists of radiation therapy, systemic chemotherapy, hormonal therapy, or a combination of these modalities, depending on the disease load elsewhere in the body.
- Radiotherapy
- Can offer a dramatic improvement in the orbital signs and symptoms, including motility disturbance, mass effect, and visual loss due to compressive optic neuropathy
- Radiotherapy is particularly useful if there are rapidly dividing cells.
- External beam radiation of 2,100–4,000 cGy is the most commonly used treatment for orbital metastasis (Mahadjer, OPRS 2005).
- Hormone therapy is mainly used in breast and prostate carcinoma.
- Chemotherapy can be used in tumors that are not responsive to hormone therapy.
- Orbital surgery and debulking is indicated only in selected cases where the tumor is small, well-circumscribed, and easily accessible, or where it threatens vision or for palliation in cases where the tumor causes extreme proptosis and pain (Shields, OPRS 1988).
- Tumor-specific considerations
- Carcinoid tumor
- For orbital carcinoid, the gold standard after diagnostic biopsy is radionucleotide localization of systemic metastases and treatment with initial local radiotherapy with additional systemic chemotherapy (Mehta, Ophthalmology 2006).
- Orbital carcinoid can also form part of a familial syndrome including multiple endocrine neoplasia (MEN) syndrome 1 or 2, von Hippel-Lindau syndrome, and neurofibromatosis 1 (Mehta, Ophthalmology 2006).
- Melanoma
- Immunotherapy agents such as interferon, interleukin-2, and monoclonal antibodies, including ipilimumab, have been used for metastatic melanoma (Greene, OPRS 2014).
- Tumors with isolated orbital metastasis carry the best prognosis for survival.
Preventing and managing treatment complications
Ocular toxicity from radiation therapy including keratitis sicca, cataracts, optic neuropathy, and radiation retinopathy are possible, but in most patients, these might not become significant if the life expectancy is not more than a year.
Disease-related complications
If untreated, orbital metastasis will lead to progressive destruction of the orbital bony and soft tissues and can extend into adjacent spaces such as the paranasal sinuses and brain.
Generally poor prognosis with the exception of breast cancer, for which there have been a recent trend towards prolongation of survival with systemic therapies despite the presence of metastatic disease in the orbit. The mean survival rates have varied from 15-18 months (Wladis et al, Orbit, 2020), and the presence of a known primary does not appear to impact survival (Magliozzi et al, Int J Ophthalmol, 2015). Nonetheless, the histologic subtype of tumor changes the prognosis considerably.
Death from carcinoid metastases is usually due to cardiotoxicity of systemic serotonin rather than the tumor in the orbit (Mehta, Ophthalmology 2006).
References and additional resources
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2010-2011.
- Char DH, Miller T, Kroll S. Orbital metastases: diagnosis and course. Br J Ophthalmol. 1997;81:386-390.
- Rootman J, ed. Diseases of the Orbit: A Multidisciplinary Approach. Philadelphia: Lippincott; 1988.
- Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opinion Ophthalmol. 2007;18:405-413.
- Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opinion Ophthalmol. 2007;18:405-413.
- Albert DM, Jakobiec FA et al. Principles and Practice of Ophthalmology. 3nd ed. Vol. 1-6 Philadelphia, PA: W.B. Saunders, 2008.
- Amemiya T, Hayashida H, Dake Y. Metastatic orbital tumors in Japan: a review of the literature. Ophthalmic Epidemiol. 2002;9:35-47
- Char DH, Miller T, Kroll S. Orbital metastases: diagnosis and course. Br J Ophthalmol 1997;81:386-390.
- Dhrami-Gavazi E, Lo C, Patel P et al. Gestational choriocarcinoma metastasis to the extraocular muscle: a case report. Ophthal Plast Reconstr Surg. 2014;30:75-77.
- Eldesouky MA, Elbakary MA, Shalaby OE et al. Orbital metastasis from hepatocellular carcinoma: Report of 6 cases. Ophthal Plast Reconstr Surg. 2013 Nov 5 [Epub ahead of print]
- Font, R. L., Croxatto, J. O., Rao, N.A. Tumors of the eye and ocular adnexa. Washington, D. C.: American Institute of Pathology.
- Font RL, Ferry AP. Carcinoma metastatic to the eye and orbit III. A clinicopathologic study of 28 cases metastatic to the orbit. Cancer; 1976;38(3):1326-1335.
- Fratkin JD, Purcell JJ, Krachmer JH, Taylor JC. Wilms’ tumor metastatic to the orbit. JAMA 1977;238:1841-1842.
- Goldberg RA, Rootman J, Cline RA. Tumors metastatic to the orbit: a changing picture. Surv Ophthalmol. 1990;35:1-24.
- Greene DP, Shield DR, Shields JA et al. Cutaneous melanoma metastatic to the orbit: Review of 15 cases. Ophthal Plast Reconstr Surg. 2014;3:233-237.
- Gupta P, Singh U, Singh SK et al. Bilateral symmetrical metastasis to all extraocular muscles from distant rhabdomyosarcoma. Orbit. 2010;29:146-148.
- Johnson D, Warder D, Plourde ME et al. Orbital metastasis secondary to Merkel cell carcinoma: case report and literature review. Orbit 2013;32:263-265.
- Karcioglu ZA. Orbital Tumors: Clinical Diagnosis and Treatment. 1st ed. New York, NY: Springer-Verlag 2005.
- Lau JJ, Trobe JD, Ruiz RE et al. Metastatic neuroblastoma presenting with binocular blindness from intracranial compression of the optic nerves. J Neuroophthalmol. 2004;24:119-124.
- Magliozzi, et al. Int J Ophthalmol, 2015.
- Malviya VK, Blessed W, Lawrence WD et al. Retroorbital metastases in ovarian cancer. Gynecol Oncol. 1989;35:120-123.
- Mehta JS, Abou-Rayyah Y, Rose GE. Orbital Carcinoid Metastases. 2006;113:466-472.
- Mohadjer Y, Holds JB. Orbital metastasis as the initial finding of breast carcinoma: A ten-year survival. Ophthal Plast Reconstr Surg. 2005;21:65-66.
- Mohan K, Gupta A, Saini JS et al. Retinoblastoma metastatic to the contralateral orbit. Br J Ophthal 1990; 74:311-312.
- Orlandi D, Sconfienza LM, Lacelli F et al. Ultrasound-guided core-needle biopsy of extra-ocular orbital lesions. Eur Radiol. 2013;23:1919-1924.
- Patel MM, Jakobiec FA, Zakka FR et al. Intraorbital metastasis from solitary fibrous tumor. Ophthal Plast Reconstr Surg. 2013;29:76-79.
- Patel MM, Lefebvre DR, Lee NG et al. Gaze-evoked amaurosis from orbital breast carcinoma metastasis. Ophthal Plast Reconstr Surg. 2013;29:98-101.
- Rootman J. Diseases of the Orbit. A Multidisciplinary Approach. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins 2003
- Shields CL, Shields JA, Peggs M. Tumors metastatic to the orbit. Ophthal Plast Reconstr Surg. 1988;4:73-80.
- Shields JA, Shields CL, Brotman HK, et al. Cancer metastatic to the orbit: the 2000 Robert M. Curtis Lecture. Ophthal Plast Reconstr Surg. 2001;17:346-354.
- Tijl J, Koornneef L, Eijpe A et al. Metastatic tumors to the orbit—management and prognosis. Graefes Arch Clin Exp Ophthalmol. 1992;230(6):527-530.
- Valenzuela AA, Archibald CW, Fleming B et al. Orbital metastasis: clinical features, management and outcome. Orbit. 2009;28:153-159.
- Yarovoy AA, Bulgakova ES, Shatskikh AV et al. CORE needle biopsy of orbital tumors. Graefes Arch Clin Exp Ophthalmol. 2013;251:2057-2061.
- Wladis E, et al. Orbit, 2020.
