Necklift (Platysmaplasty)
Updated August 2024
Natalie Homer; Tanuj Nakra
Goals, indications, contraindications
The Aging Neck
The youthful neck is described to have a distinct inferior mandibular border, a slightly visible thyroid cartilage, discernable anterior border of the sternocleidomastoid muscle, and a cervicomental angle of approximately 90-105 degrees (Figure 1). Age-related changes in the neck region result from loss of skin elasticity, mandible bone volume loss, increased visible submental liposis, platysmal banding and submandibular gland ptosis (Figure 2). The Dedo classification system can be used to specifically define the unique aging changes in an individual patient (Figure 3).
Contraindications to platysmaplasty are the same as for rhytidectomy, and include tobacco use, history of radiation, and vasculitis or autoimmune disease. Patients with unrealistic expectations should also be dissuaded from undergoing platysmaplasty.
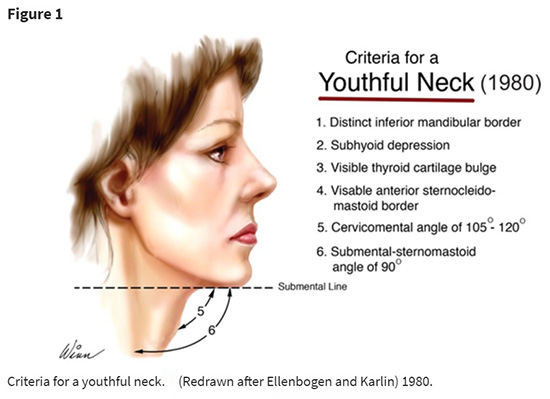
Figure 1. Criteria for a Youthful Neck
Figure credit: Daniel C. Baker, MD, Face Lift with Submandibular Gland and Digastric Muscle Resection: Radical Neck Rhytidectomy, Aesthetic Surgery Journal, Volume 26, Issue 1, January 2006, Pages 85–92
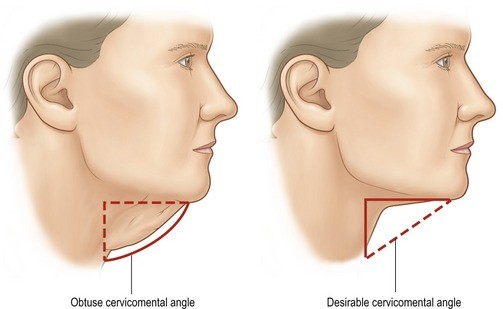
Figure 2. The Aging Neck
Figure credit: Plastic Surgery Key. Deep plane procedures in the neck. https://plasticsurgerykey.com/deep-plane-procedures-in-the-neck/

Figure 3. Dedo Classification of the Aging Neck
Figure credit: Danny Soares, MD – Facial Plastic Surgeon
Relevant Anatomy
The Dedo classification system accounts for variations of the cervicomental angle, platysmal tone, submental fat and hyoid bone projection. Class 5 and 6, with a hypoplastic mandible or anterior hyoid bone, respectively, are the most challenging cases for surgical sculpture, and may require orthognathic or mandibular augmentation for optimal results.
Platysma Muscle
The platysma muscle, analogous to the SMAS layer in rhytidectomy, is the primary instrument for soft tissue elevation in necklifting. In 1984, Dr. De Castro described three anatomical variations in configuration of the platysma muscle. The most common Type I (75%) anatomy displays an interdigitation of the platysma muscle to a point 1-2 cm posterior to the mandibular symphysis. Type II (15%) configuration shows a more extensive midline interdigitation to the level of the thyroid cartilage, whereas Type III (10%) is devoid of central platysmal interdigitation. Platysmaplasty commonly involves central suture corset to replicate a Type II anatomy type for maximal support and contouring.
Adipose Tissue
Submandibular pre and post-platysmal fat contribute to a blunted cervicomental angle in the aged population. Pre-platysmal fat may be contoured with liposuction or direct liposculpture. During surgical manipulation, a thin layer of subcutaneous fat must be preserved on the posterior skin flap surface to ensure optimum flap vascularity and also to reduce postop platysmal visibility.
Digastric Muscles
The digastric muscle functions to elevate the hyoid bone during speech and swallowing and facilitates opening of the mouth. Intraoperatively, placing the neck in a flexed position after fat removal may reveal a visible anterior digastric muscle belly, which may affect submental contouring and contribute to submandibular gland ptosis (Figure 5). Surgical debulking of the anterior belly of the digastric muscle has has not been shown to produce apparent functional consequence.
Submandibular Gland
The submandibular glands secrete approximately 45% of total salivary fluid, aiding in lubrication of food and contributing antibacterial secretory enzymes. The submandibular glands may be prominently positioned in some patients, and contribute to the cervicomental angle blunting. The submandibular gland is located within the subplatysmal space of the lateral neck, and may be partially excised at time of surgery (Figure 5). The contribution of the submandibular glands to the patient’s overall neck contour should be assessed and discussed preoperatively, as debulking carries risk for intraoperative and post-operative hemorrhage, post-operative sialocele and a theoretical risk of dry mouth.
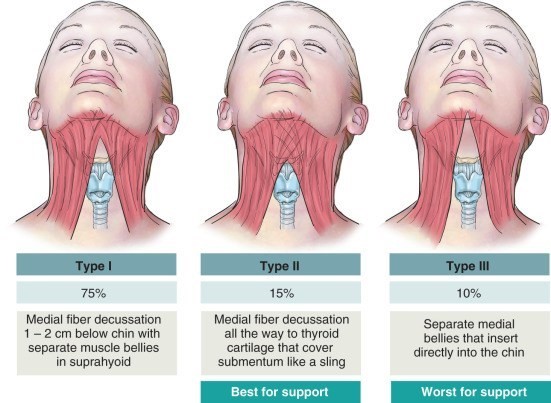
Figure 4. Platysmal Anatomy
Figure credit: Plastic Surgery Key. (Adapted from de Castro, C.C., 1984. The value of anatomical study of the platysma muscle in cervical lifting. Aesth. Plast. Surg. 8, 7–11)
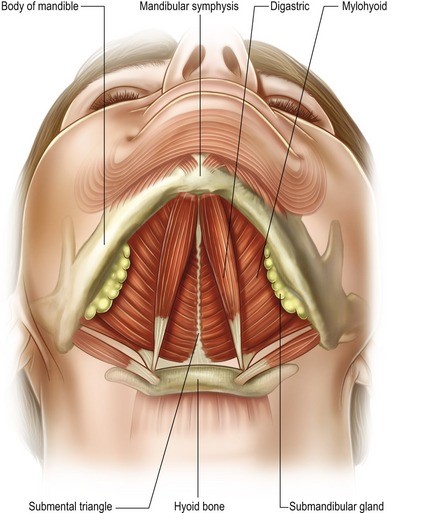
Figure 5. Submental anatomy
Figure credit: https://plasticsurgerykey.com/deep-plane-procedures-in-the-neck/
Motor Nerves
The facial nerve provides somatic innervation to the facial mimetic muscles and platysma. Relevant to necklifting surgery, the marginal mandibular nerve most often courses anteriorly above the border of the mandible, in a layer deep to the masseteric fascia, penetrates the deep cervical fascia near the mandible border, runs in a sub-platysmal plane, and crosses anterior to the facial artery and vein, at a position average 3 cm anterior to the masseteric tuberosity. Cadaveric studies have confirmed occasional initial trajectory below the inferior mandibular border. The nerve subsequently enters the buccal space to innervate the lip depressors. This nerve is susceptible to injury during sub-platysmal fat liposuction and resection.
Sensory Nerves
The great auricular nerve is the most commonly injured nerve during necklifting surgery. This nerve provides sensory innervation to the ear lobule, concha and posterior auricle. The nerve travels beneath the superficial cervical fascia but is particularly prone to injury as it crosses the posterior border of the sternocleidomastoid muscle. The nerve passes this muscle anteriorly at McKinney point, approximately 6.5cm inferior to the external auditory canal. The nerve courses between the lesser occipital nerve posteriorly) and the external jugular vein anteriorly.
Pre-procedure Evaluation
A thorough assessment of excess skin, pre- and sub-platysmal fat, platysmal banding, anterior digastric bulk, mandibular anatomy, and submandibular gland ptosis or prominence is essential. The patient should be examined both at rest and with platysmal contraction, to assess the degree of muscle hypertrophy and level of decussation. Residual soft tissue that is palpable during platysma contraction can be presumed to be subcutaneous fat.
The bony and cartilaginous neck structures should be thoroughly examined, including the hyoid bone, thyroid cartilage and cricoid cartilage. Projection of the hyoid bone anteriorly may limit the ability to redrape neck soft tissues to sharpen the cervicomental angle, which should be discussed preoperatively. Mandibular hypoplasia may also limit the redraping capacity during surgical neck rejuvenation and an alloplastic implant or sliding genioplasty should be considered.
Non-Surgical Alternatives
For mild contour issues, non-surgical alternatives are a reasonable option for neck rejuvenation.
Ultherapy
Intense focused ultrasound has been recently applied for facial rejuvenation by induction of thermal energy. The Ulthera System (Ulthera, Mesa, Arizona), released in 2004, utilizes short pulse duration (50-200ms) at high frequency (4-7 MHz) and low energies (0.5 – 10 J) to create thermal coagulation points at specific tissue depths. This treatment, initially FDA-approved for brow lifting (2009), has more recently gained approval for necklifting and can aid in neck soft tissue tone and tightening. Notably, over-reduction of subcutaneous fat can result in skin laxity and underlying platysmal visibility.
Cryolipolysis
Cryolipolysis is a method of submental fat reduction by controlled cooling and induced-apoptosis of adipocytes. Multiple sessions may be performed to achieve a desired effect. Notably, over-reduction of subcutaneous fat can result in skin laxity and underlying platysmal visibility.
Deoxycholic acid
Another minimally-invasive treatment of submental fat is with the FADA-approved deoxycholic acid (trade name Kybella; Kythera, Westlake Village, CA), injected in small aliquots into the neck subcutaneous space. This treatment has found to be safe and effective in fat reduction, with mild localized adverse effects reported. Interestingly, preliminary reports have not shown significant skin laxity to result from fat reduction, suggesting an additional effect of skin contraction from this therapy.
Laser Resurfacing and Radiofrequency Treatment
Ablative fractionated laser or radiofrequency treatment may be used in combination with the above techniques for skin tightening, typically delayed for a minimum four weeks following the primary treatment. Laser resurfacing can also aid in evening overall skin pigmentation, but should be maintained at low energy settings given risk for scarring in this region.
Chemodenervation
Prominent platysmal bands can be improved with injection of neuromodulators, though without improvement in liposis or skin laxity. This treatment is therefore best reserved for patients with retained skin elasticity and minimal submental fat.
Surgical Techniques
Submental Liposuction
Submental liposuction may be performed in isolation, or concurrent to platysmaplasty surgery. This procedure benefits from tumescent anesthetic, which allows for diffuse and safe hemostatic agent infiltration and defining of an appropriate surgical plane. Liposuction is performed of submental fat in a pre-platysmal plane, without high risk of injury to the sub-muscular motor nerves.
Submental Platysmaplasty in Conjunction with Lower Rhytidectomy
Submental platysmaplasty is commonly performed concurrent to lower rhytidectomy. These authors prefer to perform the necklifting procedure prior to initiating the lower facelift. A submental incision and subcutaneous dissection can be performed initiated after infiltration of tumescent anesthesia. The neck should be maintained in an extended position with transillumination used to guide this dissection. The optimal dissection plan divides the subcutaneous fat evenly, with a layer of adipose tissue left on the posterior surface of the skin flap for vascularity, and the remainder left overlying the platysma muscle and available for sculpting. Sculpting can be performed via liposuction or direct excision. Careful measures should be taken to avoid overresection of submental fat which may yield a cobra neck deformity.
Next, manipulation of the platysma muscle can be performed. A central ellipse of platysma and fascia can be excised with paddle-tip monopolar cautery. This excision should extend from the hyoid bone to the mid-neck. A lighted retractor can aid in visualization. Once the subplatysmal fat is exposed, this may additionally be conservatively contoured via direct excision if required.
When submandibular gland contouring is necessary, the subplatysmal space can be entered and dissection performed laterally until the submandibular gland is encountered. The capsule may be sharply entered at the inferior border and the ptotic portion of the gland debulked appropriately. Bipolar cautery is often required to achieve hemostasis in this vascular gland. One should be careful to avoid injury to the marginal mandibular nerve, which courses cephalad to the gland. The gland capsule may be closed with sutures to decrease risk of sialocele. Intraoperative intra-gland chemodenervation may also be performed to reduce salivary output during the initial postoperative period. Deep drains may be placed for several days to wick away aberrant gland drainage.
Following subplatysmal fat sculpting, the digastric anterior muscle belly can be assessed by flexing the patient’s neck and viewing the submental region. Some surgeons will excise up to 90% of the anterior muscle belly to achieve a slightly concave appearance in the submental region. It is important to avoid overresection of submental fat and muscle soft tissues, which may lead to a cobra deformity.
Once an adequate submental contour has been achieved, the platysmaplasty may be completed via undermining of the two free cut edges, followed by central corset suturing along the midline (Figure 6). Interrupted or running suture techniques may be utilized. Lateral cutbacks are often made in the inferior cut-edge of the platysma to aid in the redraping of the muscle with eventual lateral SMAS suspension.
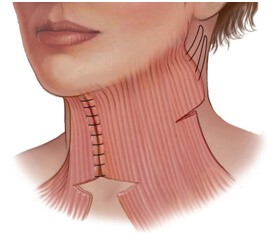
Figure 6. Corset Platysmaplasty
Figure credit: https://www.youniquecosmeticsurgery.com/contents/surgery/face/neck-lift
Direct Necklift
In the patient population desiring isolated neck rejuvenation without jowl correction, a direct neck lift may be considered. This procedure is most appropriate in the male population, where thick, hair-bearded skin may hide a vertical midline scar. The skin incision can be fashioned in a zigzag, lazy H, T-Z plasty, W-plasty, or ellipse with T-closure pattern at the midline. These authors prefer a W-plasty, which yields a non-linear incision line to optimize visually elusive healing (Figure 7). A subcutaneous incision is made and lateral undermining is performed and submental liposculpture is directly performed. A midline platysmal ellipse excision and corset platysmaplasty as well as subplatysmaplasty can be performed concurrently. Careful wound closure should be performed with numerous subcutaneous buried sutures, followed by superficial suture closure.
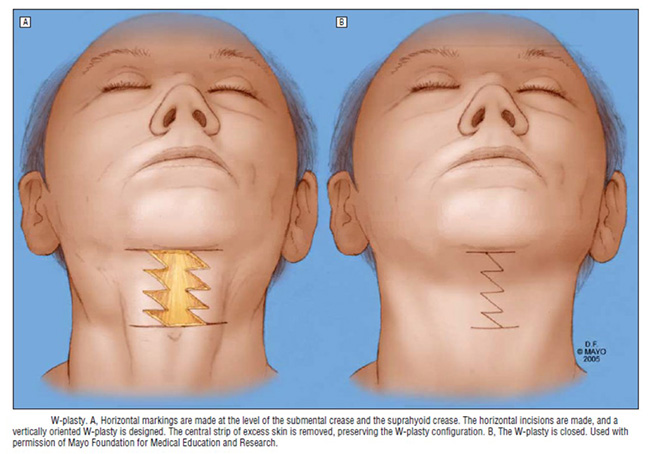
Figure 7. W-plasty incision for direct neck lifting
Figure credit: Bitner JB, Friedman O, Farrior RT, Cook TA. Direct Submentoplasty for Neck Rejuvenation. Arch Facial Plast Surg. 2007 May/June;9:194-200.
Mandibular Augmentation
Mandibular augmentation, either via sliding genioplasty or augmentation via implantation of alloplastic or autogenous tissue, may be performed concurrent to necklifting to further define the cervicomental angle in cases of mandibular hypoplasia or recession.
Post-Operative Management
Compressive dressing
Post-operatively a compressive dressing should be placed, comprised of Kerlix and a Coband, to place constant gentle pressure on the submental and upper neck regions. The submental incision should be protected beneath the dressing with a smooth drain sponge or Telfa. This dressing should remain in place until post-operative day 1, at which time the patient should be transitioned to a soft neck wrap. These authors instruct patients to wear this wrap full-time for the first post-operative week, and at bedtime only for the second post-operative week. It is important that the patient take limited compression breaks and prevent too tight of wrapping, to avoid flap compression ischemia.
Drain management
For submental necklifting, a JP drain should be inserted bilaterally at time of surgery and secured to the patients post-auricular area to remain in place overnight. If no evidence of accumulated hematoma or seroma, these drains can be removed on post-operative day 1 or 2. If excessive edema is present or concern for fluid collection exists, the drains should be checked for proper aspiration. If properly functioning, the drains should remain in place, the patient placed on oral antibiotics and monitored daily for improvement. In cases of submandibular gland excision, an independent deep subplatysmal drain may be placed intraoperatively and maintained for several days post surgery, with removal timing dictated by tapering salivary gland output.
Post-operative evaluations
For routine healing, the patient should be examined a minimum of day 1, day 7 and month 1 following platysmaplasty. Simultaneous treatment with skin resurfacing, or any evidence of complications, may mandate closer follow-up.
Complications
Cobra neck deformity
A “cobra neck deformity” may result from overaggressive resection of submental fat or anterior digastric muscle (Figure 8). Volume augmentation can be performed with autologous fat transfer as a reconstructive treatment option.

Figure 8. Cobra Neck Deformity Resulting from Overzealous Submental Fat Excision
Figure credit: Botched (https://www.youtube.com/watch?v=2Fz9lhz0Yxs)
Undercorrection
Residual neck fullness may be noted in the post-operative period from underresected submental fat or inadequate skin redraping. Minimal contour irregularities may be amenable to non-operative remediation, including with Ultherapy, deoxycholic acid, cryolipolysis or laser resurfacing. Moderate contour deformities may require surgical revision. Residual skin excess can be improved with delayed posterior surgical redraping, which can be performed a minimum of six weeks post-surgery to allow for adequate revascularization of skin flaps.
Vascular injury
The external jugular vein travels medial to the great auricular nerve and can sustain trauma if not carefully avoided. Injury to the external jugular vein requires suture ligation for hemostasis. Overcautery of subcutaneous vascular supply during surgery can produce vascular compromise to the edges of the skin flap, producing tissue ischemia and poor healing.
Great auricular nerve injury
Even without injury to the great auricular nerve, sensory hypoesthesia across the area of the subcutaneous flap due to transection of minor branches of the nerve is common after rhytidectomy surgery, and typically resolves within 12 months. The great auricular nerve is the most commonly injured nerve during cosmetic surgical lower face and neck surgery. As this nerve provides sensory innervation to the lower ear, parotid and mastoid areas, damage may result in hypoesthesia, paresthesia or painful neuroma in those regions. Careful avoidance of violating the deep cervical fascia during surgical dissection can minimize risk of injury. Transection noted intraoperatively should be repaired with end-to-end anastamosis, usually with good outcome.
Historical Perspective, References and Additional Resources
- Adamson JE, Horton CE, Crawford HH. The surgical correction of the “turkey gobbler” deformity. Plast Reconstr Surg. 1964;34:598-605.
- Bitner JB, Friedman O, Farrior RT, Cook TA. Direct Submentoplasty for Neck Rejuvenation. Arch Facial Plast Surg. 2007 May/June;9:194-200.
- Vanaman M, Fabi SG, Cox SE. Neck Rejuvenation using a Combination Approach: Our Experience and a Review of the Literature. Dermatologic Surgery. 2016 May;42(5S):S94-S100.
- Warren RJ, Aston SJ, Mendelson BC. Face Lift. Plast Reconstr Surg. 2011 Dec;128(6):747e-764e.
