Orbital Floor Fractures
Updated August 2024
Establishing the diagnosis
Anatomy
- The orbital plate of the maxilla forms the largest part of the floor.
- The orbital surface of the zygoma forms the anterolateral portion.
- The orbital process of the palatine bone forms a small area of the floor behind the maxilla.
- The orbital floor slopes upward medially at 45° and ascends posteriorly at about 30°.
- The floor of the orbit is traversed by the infraorbital sulcus or groove, which runs almost straight forward from the inferior orbital fissure and becomes the infraorbital canal carrying the infraorbital nerve and vessels.
- The floor of the orbit is separated from the medial wall by a thin suture line.
- The floor is separated from the lateral wall posteriorly by the inferior orbital fissure. Anteriorly the floor is continuous with the lateral wall.
- The medial floor is about 0.4–0.5-mm thick. It is most thin over the infraorbital canal.
- The lateral orbital floor is much thicker than the medial floor and is approximately 1.25-mm in thickness.
- Below the floor of the orbit, for nearly its whole extent, lies the maxillary sinus.
Etiology
- Low-velocity blunt trauma to the lids and globe can raise hydrostatic pressure in the orbit and fracture the thin medial portion of the floor causing it to “blow out” into the maxillary sinus.
- The weakest point on the orbital floor is usually along the infraorbital groove, therefore the greatest point of separation of the bone fragment in a blowout fracture is usually along the infraorbital groove.
- “Hinged” bone fragment can be separated at the infraorbital groove and attached to the medial wall (Figure 1).
- Alternatively, 2 points of separation can develop — along the infraorbital groove and at the junction with the medial wall — causing the medial orbital floor to be displaced downward into the maxillary sinus.
- Rarely, the separation is primarily at the junction with the medial wall causing the bone to be “hinged” in the opposite direction, with remaining attachment along the infraorbital groove.
- Rarely, a hinged fracture is lateral to the infraorbital groove — the thin bone fragment remaining attached to the thick lateral zygomatic bone (JAMA Ophthalmol 2013; 131:1492).
- High-velocity blunt trauma absorbed directly by the bone along the orbital rim is more likely to displace the zygoma, possibly causing the orbital floor to buckle and fracture in an anterior-posterior direction.
- Can be associated with other orbital and facial fractures as well as intracranial or soft tissue trauma
- Rarely, fractures can be spontaneous, such as with Graves disease (OPRS 2010; 26:301).
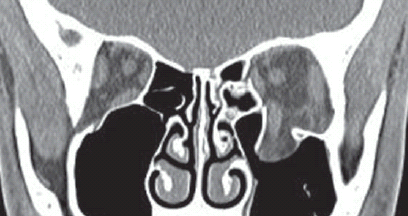
Figure 1. CT exam of a medial hinged floor fracture. Note the concomitant medial-wall fracture and orbital contents herniating into the maxillary sinus. Inferior rectus muscle is rotated 90 degrees.
Epidemiology
- Among 133 orbital floor fractures with CT scans treated at Moorfields Eye Hospital in London from 1991 to 2008, 72 (54%) had isolated involvement of the floor; the remainder had concomitant medial wall fractures.
- Among 113 orbital floor fractures treated at Fukushima University in Tokyo from 1999 to 2002, 87 (77%) were males, reflecting a predominance of men in most series of orbital fractures (AJO 2006; 142:1019).
- There were 19 females among 54 orbital fractures treated at Penn State University from 1989 to 1993, the majority due to domestic violence/sexual assault and motor vehicle accidents (6/19 or 31% each) (Ophthalmology 1996; 103:953).
- Intimate partner violence is an important factor to recognize; surgical intervention has secondary implications in helping to emphasize the severity of the experience and injury (OPRS 2014; 30:508).
- There can be variation in anatomic predisposition: Afro-Caribbean patients sustained medial wall fractures more commonly (only 2/19 or 10% had isolated floor fractures) than Caucasians and Asians in the Moorfields study (Ophthalmology 2011; 118:1677).
- Adult patients are more likely than pediatric patients to develop floor fractures.
- Orbital fractures in children are most commonly associated with sports injuries.
Pathophysiology
- In classic (indirect) blowout fracture, also known as orbital hydrostatic theory, low-velocity blunt force to the soft tissue raises the intraorbital pressure fracturing the thin medial orbital floor (Figure 2).
- Relative weakness in the orbital floor provides an energy outlet to protect the globe from mechanical displacement and rupture (OPRS 2000; 16:188).
- Based on cadaver studies the estimated energy required to fracture the bone of the orbital floor according to the hydrostatic theory is about 71-78 mJ (OPRS 2000; 16:188).
- Direct fractures are caused by strong forces applied directly to the malar eminence or inferior orbital rim causing buckling of adjacent floor in an anterior-posterior direction.
- Because the rim is the thickest portion of the orbit, stronger forces (such as those in a motor vehicle accident) are required to fracture this bone.
- “Trapdoor” fractures are more common in younger patients.
- Sometimes referred to as white-eyed fractures because other signs of periocular trauma such as bruising or subconjunctival hemorrhage can be absent.
- Pediatric bones have a higher proportion of osteocytes than osteoblasts with a smaller amount of calcified osseous tissue, so they are more pliant.
- Entrapment of orbital soft tissue is more common in greenstick fractures than in blowout type fractures.
- Perimuscular fascia is more commonly entrapped than the actual inferior rectus muscle.
- If the muscle or its fascia is entrapped, vertical diplopia with an inability to fully elevate the eye is common.
- The patient often refuses to look upward secondary to pain and nausea. The oculocardiac reflex with bradycardia on elevation might also be seen.
- Muscle entrapment is a relative emergency as the blood supply to the inferior rectus can be compromised and muscle necrosis can occur.
- After surgery, the patient might continue to have vertical diplopia for some time secondary to trauma to the inferior rectus muscle. Damage to the third nerve branch or hematoma of the muscle might prevent it from working normally.
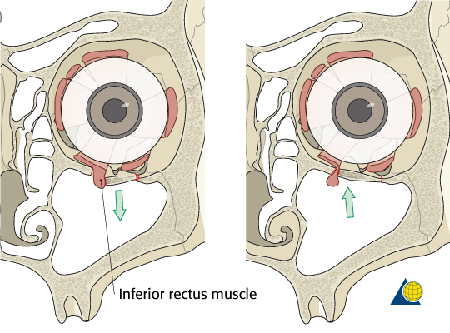
Figure 2. Illustration of the mechanism for entrapment with a floor fracture.
History
- Elicit a detailed and extensive history of the mechanism of injury.
- Most commonly the mechanism is a traumatic event, but can be seemingly incidental in children.
- Of particular importance is the patient’s visual acuity immediately after the event.
- Roughly 70% of all orbital trauma patients will have a globe injury.
- Elicit a list of comorbidities that can influence your surgical decisions.
Clinical features
- Life-threatening injuries and vision-threatening injuries always take precedent.
- If the globe has ruptured, diplopia and enophthalmos, potential sequelae of the floor fracture, become less relevant.
- Visual acuity and pupil evaluation
- Check pupil size and shape.
- Is there a possibility of traumatic optic neuropathy?
- Slit lamp or pen light evaluation
- Is there a hyphema?
- Other intraocular injuries such as traumatic iritis, lens subluxation, angle recession, commotio retinae etc?
- Intraocular pressure evaluation — unless the globe is obviously open
- Extraocular motility evaluation
- Check ductions and versions; pain on upgaze might suggest orbital tissue and/or inferior rectus muscle entrapment.
- Diplopia — check forced ductions.
- Globe position evaluation
- Hertel measurements.
- Is there hyper or hypo globus?
- Large fractures can induce luxation of the globe through the bony defect (OPRS 1991; 7:303) (Figure 3).
- Severe injury resulting in globe luxation into the maxillary sinus can cause irreversible complete visual loss (OPRS 2007; 23:156).
- Late visual recovery to 20/20 six weeks after repositioning a subluxed globe has been reported in a patient also treated with intravenous methylprednisolone (250 mg every 6 hours), but the patient was left with a severely constricted visual field (OPRS 2011; 28: e17).
- Canthal evaluation
- Check for telecanthus.
- Is the canthus stable to bimanual palpation?
- Cranial nerve V evaluation
- Hypesthesia, dysesthesia, or hyperalgesia in V1 and V2.
- Palpation
- Is there a step-off deformity of the orbital rim?
- Is trismus present?
- Is there crepitus?
- Is there decreased retropulsion or a tense orbit?
- Is there palatal movement?
- Is there mandibular stability?
- Check for periorbital edema, ecchymosis, subcutaneous emphysema
- In children and young adults with a “trap-door” fracture
- Minimal signs of external trauma.
- Double vision on upgaze and less commonly on downgaze
- Supraduction can illicit nausea, vomiting, and bradycardia because of the oculocardiac reflex
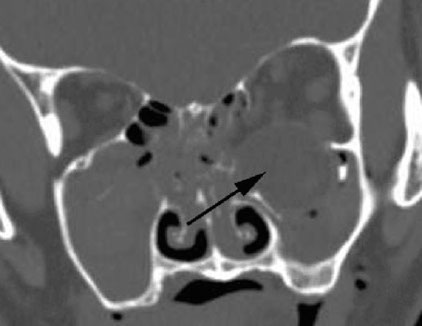
Figure 3A. Coronal CT exam demonstrating hypoglobus with subluxation of the globe into the maxillary sinus.
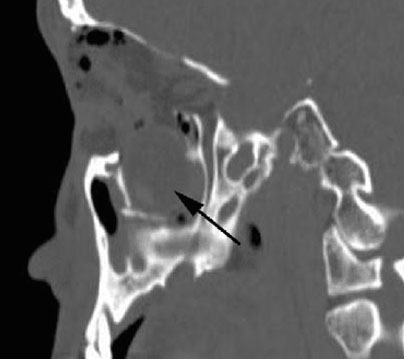
Figure 3B. Same CT in the sagittal plane.
Testing
- Facial computed tomography (CT) scan
- Thin cuts (2–3 mm) without contrast
- Axial, coronal and sagittal views
- Bone and soft tissue windows
- Extensive (panfacial) fractures can be evaluated with a 3D CT (Figure 4).
- Floor fractures are best evaluated in the coronal and sagittal views.
- Look for a trapdoor type fracture with entrapped orbital tissue especially in children and teens.
- Look for opacification or air/fluid level in maxillary sinus
- X-rays are of very limited use.
- Can be of use when evaluating for metallic foreign bodies.
- Bone windows
- Look for location, size and morphology of the fracture.
- Coronal views allow the surgeon the best medial/lateral evaluation to judge the extent of medial wall and lateral floor involvement.
- If severe head or neck trauma does not allow for direct coronals then reconstructed views can be obtained.
- Sagittal views allow the surgeon to evaluate the anterior/posterior aspect of the fracture and judge the size of the posterior ledge.
- Axial views allow the surgeon to judge the involvement of the medial and lateral walls of the orbit and optic canal.
- Look for other facial fractures
- Medial wall, lateral wall, orbital roof
- Maxillary, ethmoid, frontal sinuses
- Lateral maxillary buttress
- Medial maxillary buttress
- Zygomatic arch
- Nasal fractures
- Nasoethmoidal (NOE) fractures
- Mandible fractures
- Pterygoid plates
- Soft-tissue windows
- Rule out ruptured globe by evaluating the shape of the globe, location of the lens and intraocular hemorrhage.
- Look for orbital hemorrhage/hematoma.
- Look for orbital emphysema.
- Look for intraocular or intraorbital foreign bodies.
- Evaluate for proptosis or enophthalmos.
- Evaluate for hyper or hypoglobus.
- Look for signs for extraocular muscle trauma such as hematoma
- Look for signs of venous congestion such as a dilated superior orbital vein.
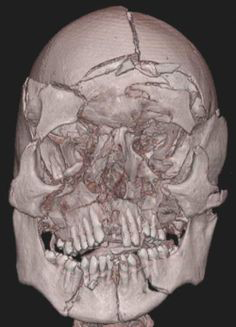
Figure 4. 3D CT exam showing a panfacial fracture.
Differential diagnosis
Direct damage to the inferior rectus muscle and/or its innervation
- Intrinsic injury to the inferior rectus muscle is marked by hypertropia with limitation of downgaze and a negative forced duction test.
- Inferior rectus muscle injury can be corrected by ipsilateral superior rectus muscle recession and partial transposition of the lateral and medial rectus muscles (J Craniofacial Surg 2013; 24:e590).
- Transection of the inferior rectus muscle also induces a large exotropia (Internat Ophthalmol 2014; 34;341).
- Hematoma in the inferior rectus can present as weakness several days after the injury (JAMA Ophthalmol 2013; 131:1492).
- Isolated inferior rectus muscle paresis can be from trauma, congenital or vascular anomaly (Strabismus 2014; 22:58).
- Third nerve branch palsy.
Direct damage to the superior rectus muscle and/or its innervation
- Muscle hematoma
- Third nerve branch palsy
Patient management: treatment and follow-up
Medical therapy
- Can observe for 7–10 days for resolution of motility disturbance resulting from edema, hemorrhage, rectus muscle contusion.
- If the fracture is large and associated with early enophthalmos then a period of observation is not indicated.
- Medications
- Nasal decongestants
- Oral steroids
- Oral antibiotics — infection occurred in 0.8% of orbital fractures in 1 study; 3 of the 4 patients with infection received antibiotics (Ben Simon, Ophthalmology 2005).
- Botulinum toxin injection is less effective in correcting vertical deviation from orbital fractures, compared to similar ocular deviation from other orbital pathology (Strabismus 2013; 21:165).
- Avoid nose blowing
- Ice packs for 2–3 days.
Surgery
Surgical criteria should be treated more as guidelines than strict rules. Indications for repair:
- “Trap-door” or “white-eyed” floor fractures can have severe restriction, which can cause pain and vagal symptoms of nausea, vomiting and bradycardia
- Urgent surgical intervention might be required to prevent inferior rectus ischemia.
- Surgical repair more than 48 hours after injury with white eyed blowout fracture has resulted in residual limitation in upgaze, despite adequate surgical repair (Arch Dis Child 2013; 98:445).
- Typically do not have significant enophthalmos, and the degree of fracture might appear limited on orbital imaging (OPRS 1998; 14:379).
- Unresolved diplopia in useful fields of gaze suspected to be restrictive in nature or secondary to globe malposition
- Check forced ductions
- Early enophthalmos > 2 mm
- Large fracture (> 50% of orbital floor on CT scan) indicates that enophthalmos is likely to occur.
- Concomitant medial orbital wall fracture can increase risk of progressive enophthalmos. Orbital floor fracture repair might be indicated in this setting for small or medium sized defects.
- Appropriate timing is based on the clinical exam and imaging.
- Oculocardiac reflex — bradycardia and nausea from traction on orbital contents with significant herniation of orbital contents; can be without clinical evidence of extraocular muscle entrapment (OPRS 2009; 25:496).
- Has been observed with clinical evidence of entrapment, bradycardia with vomiting was exacerbated by upgaze (BMJ Case Reports 2014, 2014).
- Oculocardiac reflex can also resolve spontaneously without surgery (Orbit 2014; 33:286).
- Infraorbital nerve hypesthesia — rarely an indication for surgical intervention
- Mostly resolves spontaneously
- Severe, progressive nerve pain and paresthesia can be an indication for surgery (OPRS 1994; 10:271).
Timing of surgery:
- Early intervention
- Trapdoor fractures with signs of severe restriction and nausea/pain
- Intervention should occur within first few days to prevent permanent motility deficits (Jordan DR, Ophthal Plast Reconstr Surg, 1998)
- Early intervention improves likelihood of complete recovery in motility deficits in pediatric population (Mehta et al. Effect of Time to Operative Intervention on Motility Outcomes Following Orbital Floor Fracture Repair in Children. Ophthalmic Plastic and Reconstructive Surgery)
- Delayed intervention
- Typically 7–14 days after trauma to allow for edema to subside making the surgery easier and safer by decreasing the chances for a compartment syndrome.
- In a comparison of 36 orbital floor fractures with diplopia repaired early (average 9 days after injury), versus 22 late repairs (average 19 days after trauma), there was no significant difference in postoperative diplopia (OPRS 2008; 24:437).
- Late intervention
- Might be weeks to months after injury; repair more than 6 weeks after injury can still have good outcomes, but prognosis is more varied. (OPRS 2015).
- Some surgeons will wait until visually significant enophthalmos develops or diplopia remains.
- Additional reports have indicated that outcomes of fractures in which repair was delayed might be similar to those of more acutely repaired fractures among oculoplastic surgeons (Dal Canto, Ophthal Plast Reconstr Surg 2008)
Preoperative evaluation:
- Enophthalmos
- In addition to Hertel measurements, volumetric analysis of CT images can have predictive value, estimating bone displacement (BJO 1993; 77:100).
- CT images can be more helpful early after the injury, with clinical exam altered by edema and hemorrhage.
- As an approximation, volumetric expansion of 1 cm3 correlates with 0.8 mm of induced enophthalmos (BJO 1994; 78:618).
- A 1.5-cm-wide fracture, involving half the typical orbital floor, with 2 cm in depth, typical of the maxillary sinus, and 1 cm displacement, potentially creates volumetric expansion of 1.5 x 2 x 1 = 3 cm,3 presenting concern about postoperative enophthalmos.
- Because a hinged fracture creates a bisecting triangle, it might induce only half the volumetric expansion.
- When floor fractures are combined with medial wall and zygoma fractures the likelihood of enophthalmos is greater.
- Diplopia
- Hess screen can confirm restriction of muscle movement and isolate involved muscle (AJO 2006; 142:1019).
- Hess area ratio (HAR) is defined as percentage of total measured ocular motility on the affected side compared to movement on the unaffected side.
- In a study of 30 patients with orbital fractures and diplopia undergoing repair within 7 days after injury, 13 (43%) with HAR > 85% had no postoperative diplopia while 5/8 (52%) with HAR <65% had postoperative diplopia at four months (OPRS 2009; 25:123).
- Stop anticoagulants if possible.
Surgical approach:
- Transconjunctival approach (Figure 5).
- Probably the most common approach used by oculofacial surgeons.
- Without or with lateral canthotomy (“swinging eyelid”) for better exposure.
- Conjunctival incision
- Subtarsal
- Midfornix
- Can be extended for access to medial and lateral orbital walls.
- Advantages
- No visible scar
- Wide access to the inferior orbit
- Less chance for postoperative lid retraction
- No damage to the orbicularis or its innervation
- Disadvantages
- Less direct approach
- Higher learning curve
- Transcutaneous (Figure 6).
- Less commonly used by oculofacial surgeons
- Skin incision
- Subciliary
- Subtarsal
- Orbital rim
- Advantages
- More direct approach
- Less of a learning curve
- Disadvantages
- Visible scar
- Higher chance of cicatricial lower lid retraction
- Transantral endoscopic
- Rarely used
- Requires endoscopic equipment
>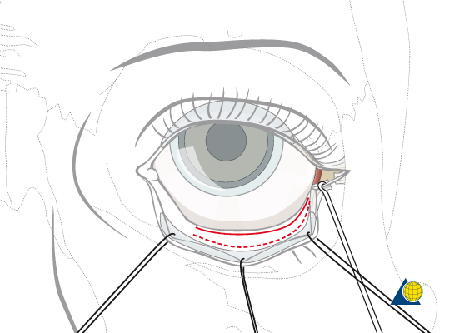
Figure 5. Illustration of the transconjunctival approach to the orbit.
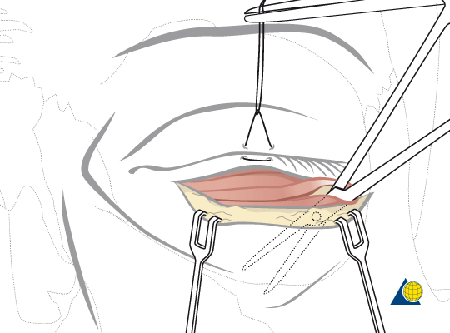
Figure 6. Illustration of the transcutaneous approach to the orbit.
Transconjunctival procedure:
- General anesthesia, lidocaine with epinephrine into the lower lid.
- Perform forced ductions. (Figure 7).
- Evert the lower lid.
- Open conjunctiva (e.g., with monopolar knife) with or without release of the lateral canthus.
- Sharply and bluntly dissect posterior to the orbicularis and anterior to the orbital septum.
- Blunt retractor in lower lid and conjunctiva/lower lid retractors on bridle suture over cornea.
- Open the periosteum of the rim and dissect in the plane inferior to the periosteum posteriorly in the orbit.
- Careful release of entrapped tissue from the fracture.
- Placement of implant to reproduce the anatomic position of the orbital floor.
- Posterior aspect of the implant must rest on the posterior ledge.
- Perform forced ductions and ensure release of any entrapped tissue.
- Close periosteum over the rim.
- Close conjunctiva and repair lateral canthus if it was released.
- No patch.
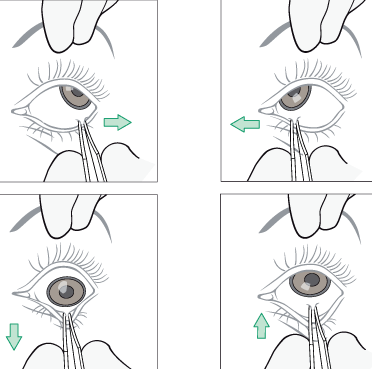
Figure 7. Illustration of forced duction testing.
Orbital floor implants:
- Autologous material
- Bone
- Calvarial
- Anterior maxillary wall
- Cartilage
- Nasal septal
- Conchal/auricular
- Fascia lata
- Periosteum
- Allogenic material
- Irradiated bone
- Lyophilized dura
- Lyophilized cartilage
- Fascia lata
- Bovine bone
- Alloplastic material
- Metallic
- Titanium mesh (Figure 8 and Figure 9)
- Vitallium mesh
- Nonmetallic
- Silastic (silicone) sheet
- Marlex mesh (crystalline polypropylene)
- Bioactive glass (glass/ceramic)
- Teflon
- Porous polyethylene — with titanium reinforcement (Figure 8) and without
- Resorbable
- Polylactic/polyglycolic (PLA/PGA) acid copolymer
- Polydioxanone (PDS)
- Seprafilm — carboxymethylcellulose and hyaluronate hybrid (OPRS 2009; 25:2011).
- Polyglactin 910 polydioxanone (OPRS 1993; 9:191).
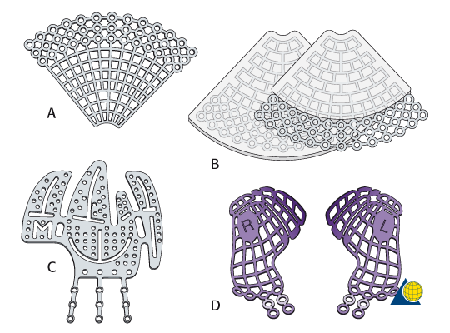
Figure 8. Illustration of various titanium implants used for orbital fracture repair. A. Titanium fan-shaped plate. B. Porous polyethylene covered titanium fan-shaped plates. C. Titanium floor and medial wall plate. D. Preformed right and left anatomic titanium floor plates.
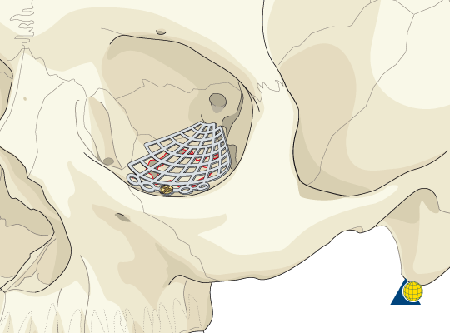
Figure 9. Illustration of titanium implant placed on the floor of the left orbit.
Postoperative care:
- Typically the surgery is outpatient and the patient is allowed to go home after the surgery.
- Medications
- Pain control medication
- Lubricating ointment
- Antibiotic ointment with or without steroid (e.g., Tobradex)
- Possibly antinausea medication
- Possibly oral steroids
- No nose blowing
- No contact sports
- No patch
- The patient might develop a hematoma with optic nerve compromise, and the patch can mask this.
- Ice packs for the first 2–3 days, then heat packs
- Instructions to call the surgeon ASAP at any hour if uncontrolled bleeding or vision loss is experienced
- Note: Some surgeons will place a drain in the orbit and admit the patient overnight.
- Follow-up in the surgeon’s office in a few days to 1–2 weeks
Preventing and managing treatment complications
Postoperative orbital hemorrhage
- Stop all anticoagulants if possible prior to surgery.
- Might require discussion with the primary care provider or other provider such as the cardiologist or cardiothoracic surgeon.
- Meticulous hemostasis during surgery.
- Consider thrombin and gel foam if excessive oozing is encountered.
- Control blood pressure during and after surgery.
- Apply cold compresses after surgery.
- Consider placing a drain if bleeding is an issue during the surgery.
- Consider removing the implant and surgically draining the hematoma if the vision is compromised.
Postoperative vision loss or blindness
- Monitor the pupil during surgery
- Take care to monitor the retractors held by the assistants.
- Size the implant appropriately and place it very carefully.
- Treatment of the vision loss depends on the etiology
- Optic nerve trauma
- Consider removing the implant.
- Consider high dose corticosteroids.
- Orbital hemorrhage
Infection
- Consider pre and intraoperative intravenous antibiotics
- Use sterile technique
- Routine postop antibiotics are controversial (Wladis, Orbit 2013)
- If postoperative infection is confirmed, treatment varies
- Confirm infection; patients often think the wound is infected when it is actually not infected
- Consider location of infection: orbital versus skin/subcutaneous tissue
- Consider source of infection: sinuses versus superficial source.
- Consider obtaining cultures tissue for microbiology.
- If no cultures, can treat empirically with IV or oral antibiotics.
- Consider draining and packing of an abscess
- Consider removal of implant.
- Reconsider the type of implant and potential need for replacement if implant is removed.
Implant related morbidity
- Extrusion
- Can be caused by infection, hemorrhage, oversized implant or poor fixation
- Treatment depends on cause and degree of migration
- Infection would be treated with antibiotics and implant removal
- Can require repositioning or replacement
- Cyst
- Fibrotic capsule or respiratory epithelium surrounds implant (OPRS 2008; 24:498).
- Cyst exacerbated by hemorrhage can become large (OPRS 2011; 27:e117).
- Can present as a mass several years after the injury (OPRS 2009; 25:238).
- Inflammation
- Some implant materials such as silicone can produce inflammation that can simulate myositis in addition to a hematic cyst (OPRS 1991; 7:267).
Hypesthesia
- Can take up to 12 months to resolve following injury or surgery
- Postop CT scan to evaluate implant and/or screw placement if hypesthesia not resolving as anticipated
Eyelid retraction or ectropion
- The transconjunctival approach has lower risk for lid retraction
- Avoid excessive traction and cautery of the lower eyelid.
- Careful wound closure to avoid shortening the orbital septum.
- Take great care to cover any titanium on the orbital rim with periosteum or other soft tissue to keep the orbicularis from sticking to and scarring the implant.
- Treatment depends on the severity of the scarring.
- Injection of steroid into the scar with vigorous massage might release the cicatrix.
- Surgery typically requires removal of the rim titanium implant
- Spacer material is typically required to prevent rescarring
- Hard palate mucosa works very well
- Upper lid free tarsal graft
- Auricular cartilage (can be bulky)
- Alloderm (human cadaveric dermis)
- Tarsys (decellularized porcine derived membrane)
- Tutoplast (human preserved sclera)
- Porous polyethylene (high complication rate)
- Others
- Keeping the eyelid on stretch over the cornea for several days can be very helpful.
Persistent restriction of motility
- Treatment depends on etiology.
- Ensure release of all entrapped tissue after the implant has been placed into position.
- Perform forced ductions prior to closing of the wound.
- Consider follow-up imaging studies to evaluate implant position and possibility of residual tissue incarceration.
- Restricted motility secondary to rectus muscle damage will typically resolve over weeks to months.
- Muscle hematoma
- CN III branch trauma
Enophthalmos undercorrection
- Ensure that the orbital implant is placed adequately on the posterior ledge and is nonmobile.
- Ensure that all fractures are adequately addressed (e.g., floor and medial wall)
- Evaluate for incorrect implant placement with follow-up CT scan.
- Consider implant replacement or augmentation of orbital volume.
- This can be difficult because of orbital scarring, rectus muscle retraction, and fat atrophy.
- Augmentation material must be placed behind the globe and not underneath or hyperglobus will result.
Enophthalmos overcorrection
- Ensure that the proper size and thickness of implant is used
- Ensure proper placement of the implant
- The overcorrection typically improves with time as edema resolves.
Persistent lymphedema
- Most commonly seen with cutaneous approach
- Ensure the incision placement does encroach on the lymphatic vessels of the lateral canthus.
- Warm compresses to increase blood flow and decrease healing time.
- Typically improves over time.
Disease-related complications
Soft-tissue emphysema
- Commonly seen after facial trauma can be introduced by nose blowing or sneezing.
- Orbital emphysema with proptosis typically resolves without intervention.
- In severe cases, release of the intraorbital air pocket with a large gauge needle might be indicated.
- Severe subcutaneous emphysema can extend beyond the orbit and sinus onto the neck and chest, causing airway obstruction and necessitating intubation (OPRS 2005; 21:465).
Orbital hemorrhage
- Commonly seen after orbital trauma, typically resolves without intervention.
- In severe cases, the increased orbital pressure can cause compromise of blood flow to the optic nerve.
- Emergent release of the lateral canthus via lateral canthotomy and cantholysis might be required.
- Out-fracturing of orbital walls and/or drainage of the hematoma with drain placement might be required.
Persistent diplopia
- There are multiple potential causes for persistent diplopia including injury to the muscle and/or innervation of the extraocular muscle.
- Can be caused by persistent muscle entrapment
- In a study of 19 patients younger than 20 years old and treated 2000–2008 for entrapment, delaying surgery more than a week after the injury increased the likelihood of postoperative upgaze diplopia, but this resolved within 2 months without additional surgery (BJO 2010; 94:736).
- Can require prism glasses or strabismus surgery
- When scarring limits strabismus repair to ipsilateral inferior rectus muscle, moderate vertical deviation can also be corrected by contralateral superior oblique posterior tenotomy (Strabismus 2013; 21:29).
Enophthalmos
- Relatively common, especially if multiple orbital walls are involved.
- Early enophthalmos can continue to worsen over time.
- Late enophthalmos might be seen as edema resolves.
- Typically easier to repair in the first 2–3 weeks after injury but can be repaired weeks to months later.
Aberrant maxillary sinus drainage
- Prolapsed orbital contents can potentially interfere with drainage of maxillary sinus.
- Can produce congestion and silent sinus syndrome with secondary enophthalmos; can be corrected with maxillary antrostomy (OPRS 2004; 20:241).
- Fistulous tract between orbit and maxillary sinus can predispose to orbital emphysema; can be repaired with a patch graft (OPRS 1995; 11:66).
Orbital cellulitis
- Uncommon after orbital fractures
- Can be secondary to sinus infection or from direct communication between the nose and orbit.
- Can be secondary to foreign matter (e.g., plant material) introduced at time of the trauma.
- Treat with topical and systemic antibiotics.
- Might require surgical drainage with cultures.
Sinusitis
- Uncommon after orbital fractures.
- Oxymetazoline (alpha adrenergic agonist) induces vasoconstriction and improves airflow and drainage.
- Treat with systemic antibiotics.
- Might require ENT referral
Patient instructions
- Typically the surgery is outpatient.
- Medications
- Pain control medication
- Lubricating ointment
- Antibiotic ointment with or without steroid (e.g., Tobradex)
- Possibly antinausea medication
- Possibly oral steroids
- Avoid nose blowing
- No contact sports until cleared by physician
- No patch — can develop a hematoma with optic nerve compromise and the patch can mask this.
- Ice packs can be helpful for the first 2–3 days
- Instructions to call the surgeon ASAP if uncontrolled bleeding or vision loss is experienced.
- Some surgeons will place a drain in the orbit and admit the patient overnight.
- Follow up in the surgeon’s office in a few days to 1–2 weeks.
- Avoid swimming or scuba diving or other activities associated with substantial changes in pressure.
References and additional resources
- AAO, Basic and Clinical Sciences Course. Section 2: Fundamentals and Principles of Ophthalmology; Section 6: Pediatric Ophthalmology and Strabismus; Section 7: Orbit, Eyelids, and Lacrimal System, 2013-2014.
- AAO, Surgical Anatomy of the Ocular Adnexa, 1996, p.52, 80.
- AAO Focal Points. Vol. XXXI, Number 1.
- Ahmad F, Kirkpatrick NA, Lyne J, et al. Buckling and hydraulic mechanisms in orbital blowout fractures: fact or fiction? J Craniofac Surg. 2006; 17:438.
- Ben Simon GJ, et al. Orbital cellulitis: a rare complication after orbital blowout fracture. Ophthalmology. 2005; 112: 2030.
- Boush BA, Lemke BN. Progressive infraorbital nerve hypesthesia as a primary indication for blow-out fracture repair. Ophthal Plast Reconstr Surg. 1994; 10:271-275.
- Burnstine MA. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol. 2003; 14:236.
- Carroll SC, Ng SGJ. Outcomes of orbital blowout fracture surgery in children and adolescents. Br J Ophthalmol. 2010; 94:736-739.
- Chang EL, Bernardino CR. Update on orbital trauma. Curr Opin Ophthalmol. 2004; 15:411.
- Charteris DG, Chan CH, Whitehouse RW, Noble JL. Orbital volume measurement in the management of pure blowout fractures of the orbital floor. Br J Ophthlmol 1993; 77:100-102.
- Cheong EC, Chen CT, Chen YR. Endoscopic management of orbital floor fractures. Facial Plast Surg. 2009; 25:8.
- Clark TJ, Renner LM, Sobel RK, et al. Intimate partner violence: an underappreciated etiology of orbital floor fractures. Ophthal Plast Reconstr Surg. 2014; 30:508-511.
- Cook T. Ocular and periocular injuries from orbital fractures. J Am Coll Surg. 2002; 195:831.
- Cruz AA, Eichenberger GC. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol. 2004; 15:416.
- Dal Canto AJ, Linberg JV. Comparison of orbital fracture repair performed within 14 days versus 15 to 29 days after trauma. Ophthal Plast Reconstr Surg. 2008; 24:437-443.
- De Silva DJ, Rose GE. Orbital blowout fractures and race. Ophthalmology. 2011; 118:1677-1680.
- Egbert JE, May K, Kersten RC, Kulwin DR. Pediatric orbital floor fracture : direct extraocular muscle involvement. Ophthalmology. 2000; 107:1875.
- Egbert Dal Canto AJ, Linberg JV. Comparison of orbital fracture repair performed within 14 days versus 15 to 29 days after trauma. Ophthal Plast Reconstr Surg. 2008; 24:437.
- Foulds JS, Laverick S, MacEwen CJ. ‘White-eyed’ blowout fracture: a case series of five children. Arch Dis Child 2013; 98:445-446.
- Furuta M, Yago K, Iida T. Correlation between ocular motility and evaluation of computed tomography in orbital blowout fracture. Am J Ophthalmol. 2006; 142-1019-1025.
- Gagnon M, Yeatts PR, Williams Z, Matthews B. Delayed enophthalmos following a minimally displaced orbital floor fracture. Ophthal Plast Reconstr Surg. 2004; 20:241-243.
- Grenga PL, Reale G, Cofone C, et al. Hess area ratio and diplopia: Evaluation of 30 patients undergoing surgical repair for orbital blow-out fracture. Ophthal Plast Reconstr Surg. 2009; 25:123-125.
- Hartzell KN, Botek AA, Goldberg SH. Orbital fractures in women due to sexual assualt and domestic violence. Ophthalmology. 1996; 103:953-957.
- Hatton MP, Watkins LM, Rubin PA. Orbital fractures in children. Ophthal Plast Reconstr Surg. 2001; 17:174.
- Jatla KK, Enzenauer RW. Orbital fractures: a review of current literature. Curr Surg. 2004; 61:25.
- Jones DF, Wilson MW. Repiratory epithelial ingrowth and hemorrhage as late complications of orbital floor fracture repair with silicone sheet implant. Ophthal Plast Reconstr Surg. 2008; 24:498-499.
- Jordan DR, Allen LH, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthal Plast Reconstr Surg. 1998; 14:379-390.
- Joseph JM, Rosenberg C, Zoumalan CI, et al. Oculocardiac reflex associated with a large orbital floor fracture. Ophthal Plast Reconstr Surg. 2009; 25:496-498.
- Kashkouli MB, Pakdel F. Spontaneous orbital floor fracture in thyroid eye disease. Ophthal Plast Reconstr Surg. 2010; 26:301-302.
- Kelly C P, Cohen A J, Yavuzer R, Jackson I T. Cranial bone grafting for orbital reconstruction: is it still the best? J Craniofac Surg. 2005; 16:181.
- Kreidl KO, Kim DY, Mansour SE. Prevalence of significant intraocular sequelae in blunt orbital trauma. Am J Emerg Med. 2003; 21:525.
- Lelli G, Milite J, Maher E. Orbital floor fractures: evaluation, indications, approach and pearls from an ophthalmologist’s perspective. Facial Plast Surg. 2007; 23:190.
- Levine M, Perla B. Maxillary sinus orbital fistula secondary to repair of an orbital floor fracture. Ophthal Plast Reconstr Surg. 1995; 11:66-69.
- Manolidis S, Weeks BH, Kirby M, et al. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. J Craniofac Surg. 2002; 13:726.
- Matteini C, Renzi G, Becelli R, et al. Surgical timing in orbital fracture treatment: experience with 108 consecutive cases. J Craniofac Surg. 2004; 15:145.
- Mauriello JA, Wasserman B, Kraut R. Use of vicryl (polyglactin-910) mesh implant for repair of orbital floor fracture causing diplopia: a study of 28 patients over 5 years. Ophthal Plast Reconstr Surg. 1993; 9:191-195.
- Mellema PA, Dewan MA, Lee MS, Smith SD, Harrison AR. Incidence of ocular injury in visually asymptomatic orbital fractures. Ophthal Plast Reconstr Surg. 2009; 25:306.
- Mullins J B, Holds J B, Branham G H, Thomas J R. Complications of the transconjunctival approach. A review of 400 cases. Arch Otolaryngol Head Neck Surg. 1997; 123:385–388.
- Otori N, Haruna S, Moriyama H. Endoscopic endonasal or transmaxillary repair of orbital floor fracture: a study of 88 patients treated in our department. Acta Otolaryngol. 2003; 123:718.
- Parbhu KC, Galler KE, Li C, Mawn LA. Underestimation of soft tissue entrapment by computed tomography in orbital floor fractures in the pediatric population. Ophthalmology. 2008; 115:1620.
- Scawn RL et al. Outcomes of Orbital Blow-Out Fracture Repair Performed Beyond 6 Weeks After Injury. Ophthal Plast Reconstr Surg. 2015; .
- Reeves DL, Lucarelli ML, Rose JG. Severe subcutaneous emphysema following orbital blowout fracture. Ophthal Plast Reconstr Surg. 2005; 21:465-467.
- Shah HA, Shipchandler TZ, Sufyan AS, et al. Use of fracture size and soft tissue herniation on computed tomography to predict diplopia in isolated orbital floor fractures. Am J Otolaryngol. 2013; 34:695.
- Sires BS, Stanley RB, Jr, Levine LM. Oculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repair. Arch Ophthalmol. 1998; 116:955.
- Smit TJ, Koornneef L, Zonneveld FW. A total orbital floor fracture with prolapse of the globe into the maxillary sinus manifesting as post-enucleation socket syndrome. Ophthal Plast Reconstr Surg. 1991; 7:303.
- Smith B, Lisman RD, Simonton J, Della Rocca R. Volkmann’s contracture of the extraocular muscles following blowout fracture. Plast Reconstr Surg. 1984; 74:200.
- Sutula FC, Palu RN. Delayed chocolate cyst after blow-out fracture. Ophthal Plast Reconstr Surg. 1991; 7:267-272.
- Taban M, Nakra T, Mancini R, et al. Orbital wall fracture repair using seprafilm. Ophthal Plast Reconstr Surg. 2009; 25:211-214.
- Villarreal P M, Monje F, Morillo A J, Junquera L M, González C, Barbón J J. Porous polyethylene implants in orbital floor reconstruction. Plast Reconstr Surg. 2002; 109:877.
- Warwar RE. Bullock JD, Ballal DR, Ballal RD. Mechanisms of orbital floor fractures: a clinical, experimental, and theoretical study. Ophthal Plast Reconstr Surg. 2000; 16:188-200.
- Whitehouse RW, Batterbury M, Jackson A, Noble JL. Prediction of enophthalmos by computed tomography after ‘blow out’ orbital fracture. Br J Ophthalmol. 1994; 78:618-620.
- Wladis EJ. Are post-operative oral antibiotics required after orbital floor fracture repair? Orbit. 2013; 32:30.
