Orbital Apex and Roof Fractures
Updated July 2024
Establishing the diagnosis
Etiology
- High-energy blunt trauma (Cossman, Plast Reconstr Surg 2014)
- Motor vehicle accident
- Fall
- Assault
- Sports-related injury
- Relatively low-energy blunt trauma can be seen in young children (Greenwald, Ophthalmology 1989)
- Frontal sinus typically does not develop until 7 years of age, leaving nothing to absorb energy as it extends along roof.
- Young children can develop nondisplaced linear roof fractures even with minor trauma.
- The cribriform plate can be involved.
- Penetrating trauma
- Penetrating injury by pencils is an important cause because of the possibility of retained foreign body (Cho, 2017).
Epidemiology
- 1%–9% of all facial fractures, but up to 30% of all orbit fractures in the pediatric population (Greenwald, Ophthalmology 1989, and Hink, Ophthal Plast Reconstr Surg. 2014)
- 16 of 36 children (Greenwald, 1989) had isolated roof fractures; 20 had additional fractures.
- Among 40 patients age 1-16 years with orbital fractures, mean age (4.8±3.3 years) of 14 patients with roof fractures was significantly less than mean age (12.0±4.2 years) of 26 children with other orbital fractures (Koltai, 1995).
History
- The event is recorded, including seemingly incidental trauma in children.
- Mechanism of injury
- Loss of consciousness might indicate intracranial injury
- Periorbital edema and ecchymosis
- Delayed upper eyelid hematoma is characteristic history
- Change in vision
- Diplopia
- Supraorbital nerve hypesthesia
- Pain
Clinical features
- Decreased visual function (e.g., traumatic optic neuropathy)
- Decreasing visual acuity
- Altered color vision
- Afferent pupillary defect (APD)
- Decreased ocular motility from entrapped extraocular muscles, orbital edema, or palsies of cranial nerves III, IV, and VI (Bater, Br J Oral Maxillofac Surg. 2008)
- Blepharoptosis
- Periorbital edema and ecchymosis
- Developing upper eyelid hematoma might indicate intracranial bleeding decompressing into orbit.
- Lacerations of brow or upper eyelid
- Proptosis (might be pulsatile) or globe dystopia
- Superior orbital rim stepoff or frontal bone deformity
- Cerebrospinal fluid (CSF) rhinorrhea
- Intraocular injuries (14%–29%) (Miller, Plast Reconstr Surg 1967)
- Altered mental status or other neurologic deficits
- Other associated fractures include orbital floor and medial wall, zygoma, nasal bone, frontal bone, maxilla, and mandible (Martello, Ann Plast Surg. 1997)
Testing
- Visual function
- Visual acuity
- Color vision
- Pseudoisochromatic plates (PIP)
- Red desaturation
- Pupil exam
- Direct and consensual response
- Presence of absolute or relative APD
- Visual fields
- Confrontation
- Formal computerized visual field
- Dilated fundus examination
- Ocular motility
- Forced ductions to rule out restriction
- Ptosis
- Mechanical—superior orbital edema/hematoma, CSF accumulation, bone fragments
- Paralytic—oculomotor (III) nerve palsy
- Traumatic—direct damage to levator-superior rectus muscle complex
- V1 and V2 function (relative numbness)
- Assure no ruptured globe
- Globe displacement (ocular dystopia)
- Exophthalmometry
- Resistance to retropulsion
- Hypoglobus (inferior globe displacement)
- Dilated fundus exam
- Evaluate optic nerve head for decreased perfusion, swelling, or hemorrhage
- CT scan
- Axial and direct coronal views with sagittal reformats (Figures 1 and2); can also reformat for 3D imaging (Figure 3)
- Thin 1–2–mm cuts through the orbit and apex
- Frontal sinus opacification
- Presence of other facial fractures, optic canal or skull base fractures
- Intracranial injury—pneumocephalus, brain laceration, subdural or epidural hematomas (Figure 2)
- Orbital hemorrhage
- Globe injury

Figure 1. Coronal CT image showing a displaced right orbital roof fracture.
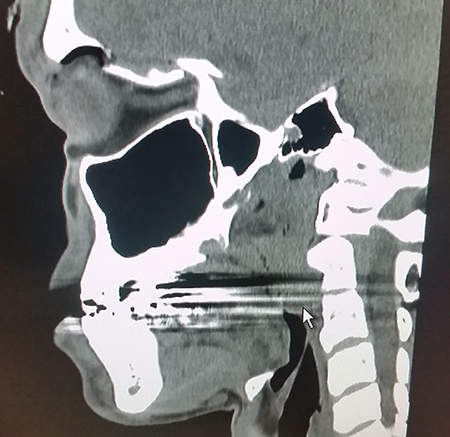
Figure 2. Soft tissue window of the same patient. Note the intraparenchymal hemorrhage just above the fracture.
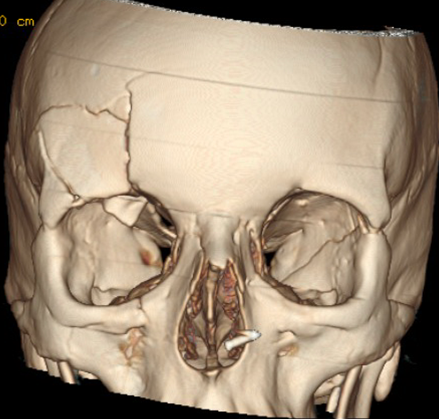
Figure 3. 3D reformat of the same patient showing an associated comminuted frontal bone fracture.
Risk factors
- Young age
- Male
- High-risk behavior
Differential diagnosis
- Orbital hemorrhage
- Frontal sinus fracture
- Cranial nerve III, IV, or VI palsy
- Orbital inflammatory syndrome
- Acute orbital infection
Patient management: treatment and follow-up
Natural history
Many roof fractures do not need repair, and good outcomes are achieved with conservative management alone.
Early surgical intervention has been advocated to prevent meningitis and brain abscess formation (Jamieson, J Neurosurg. 1973).
- However, other studies indicate that medical management or delayed surgical repair does not increase morbidity (Fulcher, Ophthal Plast Reconstr Surg. 2003).
- The decision of whether and when to proceed with surgical repair should be made in conjunction with neurosurgery, as many roof fractures involve herniated brain tissue and CSF leak.
Table 1 summarizes the indications for urgent and delayed repair.
- Urgent intervention is indicated when displaced fractures cause optic nerve compression and for associated sight-threatening complications including orbital hemorrhage and perforating eye injury (Fulcher, Ophthal Plast Reconstr Surg. 2003 and Kim, Arch Plast Surg. 2012).
- Urgent intervention is indicated with blow-in fractures from the orbital roof with removal of the bone fragment that results in globe compression (Park, OPRS, 2023).
- Delayed repair is indicated when a foreign body is present, for enophthalmos, for a persistent CSF fistula, or when bony impingement causes vertical diplopia, torsional diplopia, traumatic ptosis, or lagophthalmos (Fulcher, Ophthal Plast Reconstr Surg. 2003).
- Bone fragments that mechanically restrict the superior rectus or levator should be repositioned or removed.
Table 1. Indications for urgent and delayed repair of orbital roof and apex fractures.
Urgent repair
Displaced fracture with direct optic nerve compression
Expanding orbital hemorrhage
Perforating eye injury
Early evidence of meningitis or brain abscess
Bone fragment compression on the globe
Delayed repair
Foreign body present
Bony impingement causing vertical diplopia, torsional diplopia, ptosis, or lagophthalmos
Large dural defect resulting in persistent CSF leak
Frontal sinus fracture
Enophthalmos
CSF fistulas occur in 0.5%–3% of craniocerebral trauma (Markovic, J Craniofac Surg 2006).
- Large dural defects need repair, usually with synthetic dural grafts, pericranium, and/or fascia lata (Pease, J Neurol Surg Rep. 2013).
- For minor CSF leaks where the dural edges are apposed or where sinus mucosa bridges the dural defect, conservative management with bed rest is curative in 85%–95% of cases (Salame, Neurosurg Focus 2000).
Traumatic optic neuropathy occurs in up to 10% of patients with craniofacial fractures (Yu-Wai-Man, Coch Collab 2009).
- Results from direct injury, ischemia, or blunt trauma.
- Treatments such as optic canal decompression and high- dose corticosteroids are controversial, with no proven benefit in randomized trials (Levin, Ophthalmology. 1999).
- Final visual potential cannot be adequately predicted.
Medical therapy
- IV antibiotics if signs of sinus disease or dural laceration/CSF leak
- High-dose corticosteroids to treat traumatic optic neuropathy are controversial.
- Consider if vision compromised on presentation.
- Methylprednisolone 250 mg IV every 6 hours for 24–48 hours (Warner, Ophthalmology. 2010)
Surgery
Surgical intervention is undertaken urgently or in a delayed fashion depending on the above criteria.
- Radiologic anatomy of the paranasal sinuses, orbital apex, and optic canal should be studied carefully in each patient to assess for anomalies or traumatic abnormalities of the anatomy.
- Surgical procedures include reduction of the fracture with placement of an implant, repair of dural tear if present, obliteration or cranialization of frontal sinus (if indicated), and optic canal decompression (if indicated).
- When the inner table of the orbital roof is not involved and there is no dural tear, the orbital fracture can be accessed by superior orbitotomy.
Approaches include extracranial, intracranial, and endonasal endoscopic; the approach used is determined by the surgical needs of the patient.
Extracranial approach
- Incisions include upper lid crease, brow, Lynch, bicoronal, or through an existing laceration (Matsuzaki, 2015).
- Orbital roof blow-up fractures may be best accessed using an anterior cranial fossa approach.
- With bone fragments adherent to dura mater, there is a risk of dura mater injury when fragments are moved for reduction.
- In blow-in fractures, reduction can be performed by pushing bone fragments up into the anterior cranial fossa.
- When there are intracranial injuries that require treatment an approach from the anterior cranial fossa is necessary.
- Lid crease approach can allow for release of entrapped orbital fat, without reduction of bone.
- The fracture can then be approached superiorly through a supraorbital frontal craniotomy.
- Alternatively, the fracture can be approached inferiorly from the roof of the orbit in the subperiosteal plane.
- Good visualization of the anatomy and is a useful approach to address frontal sinus at the same time
Intracranial
- Extradural approach through a craniotomy
- Should be done in conjunction with neurosurgery
- This is the approach of choice for cases
- With large dural defects that need concomitant repair
- In which the anterior clinoid is fractured
- In which the lateral optic canal wall must be exposed
- When unroofing the plane of the sphenoid and its associated falciform dural fold is needed (Goldberg, Ophthal Plast Reconstr Surg. 1996)
Endonasal endoscopic
(Kuppersmith, Laryngoscope. 1997)
- Can be used alone or with a transconjunctival approach for optic canal decompression
- Not useful for fracture reduction
Other management considerations
Entrapped superior rectus muscle can be released (McClurg, 1976).
Optic canal decompression can be performed through an external approach, intracranial approach, or endonasal endoscopic approach.
- From an orbital approach, the medial roof of the canal can be removed.
- The carotid artery lies inferior to the nerve, and the ophthalmic artery joins the optic nerve near the intracranial optic canal and courses inferior and lateral to the nerve (Goldberg, Ophthal Plast Reconstr Surg. 1996).
- Adequate decompression of the canal is achieved when 50% of the circumference of the canal is removed, bone along the entire length of the canal is removed, and total longitudinal incision of the dural sheath, including the annulus of Zinn, is completed (Sofferman, J Microsurg. 1979).
- Complications include injury to the internal carotid artery, thermal injury to the optic nerve from drilling, and enophthalmos.
If there is compromise of the nasofrontal duct in a frontal sinus fracture, the sinus should be obliterated. If the posterior table of the frontal sinus is fractured and the anterior table intact, the frontal sinus can be cranialized.
For small, minimally displaced roof fractures with entrapment of the superior rectus or oblique muscle, repositioning of the intraocular contents without placement of a graft is often all that is necessary. Synthetic dural replacement can be used if there is significant violation of the periorbita.
With larger defects, the surgeon has several options for reduction. The ideal implant should mold to the contour of the defect, be stable over time, inert, and radiopaque.
- Bone grafts
- Calvarium, rib, or ilium are most common harvest sites.
- Advantages include biocompatible, radiopaque, no additional cost.
- Disadvantages include longer operative time, donor site morbidity, can be difficult to contour, and risk of resorption (Kim, Arch Plast Surg. 2012 and Manolidis, J Craniofac Surg 2002).
- Titanium mesh (Kim, Arch Plast Surg. 2012 and Mokal Craniomaxillofac Trauma Reconstr. 2012)
- Advantages include ease of contouring, radio-opacity, low risk of infection, stability, and no donor site morbidity.
- Disadvantages include high cost and sharp edges if not trimmed properly (Lazaridis, Aust Dent J 1998).
- Porous polyethylene
- Advantages include stability and biocompatible.
- Disadvantages include radiolucent and high cost (Rubin, Ophthalmology 1994).
- Composite materials (porous polyethylene imbedded with titanium)
- Advantages include radio-opaque, ease of contouring, more rigid than porous polyethylene alone, better tissue incorporation than titanium alone (Mokal, Craniomaxillofac Trauma Reconstr. 2012).
- Disadvantages include cost and small risk of infection.
- Nylon foil (Supramid)
- Advantages include cost and stability.
- Disadvantages include radiolucent, risk of capsule formation, and inability to mold the implant (Custer, Ophthal Plast Reconstr Surg 2003).
Young patients with associated blepharoptosis and strabismus should be followed closely to monitor for amblyopia.
Common treatment responses, follow-up strategies
- Many patients regain full visual potential and motility.
- Patients with traumatic optic neuropathy should be counseled that their final visual potential is unknown.
- Patients with residual strabismus and ptosis not secondary to bony impingement might benefit from repair. These should be observed for at least 6 months after the injury, as many will resolve with time.
Preventing and managing treatment complications
- Complications from use of high-dose corticosteroids, including liver failure, changes in blood sugar and blood pressure, and gastrointestinal damage
- Intracranial bleeding
- Persistent CSF leak
- Persistent ptosis
- Persistent diplopia
- Supraorbital hypesthesia
- Frontal sinusitis or mucocele formation
- Scar formation from external approaches
Disease-related complications
- Intracranial injuries (see Cossman, Martello, Fulcher)
- Concentration difficulties
- Seizures
- Persistent motor defects
- Dural tear
- Pneumocephalus
- CSF rhinorrhea
- Orbitocele (CSF leak into the orbit)
- Oculorrhea (CSF leak into the orbit and expressed via the ocular surface, mimicking tear formation) (Pease, J Neurol Surg Rep. 2013)
- Orbital hemorrhage
- Encephalocele (Messinger, Plast Reconstr Surg 1989)
- Frontal lobe contusions and high intracranial pressure predispose to encephalocele (Wei, 2016)
- Ocular pulsation
- Bony fragments prolapsed into the orbit
- Meningitis
- Blepharoptosis
- Enophthalmos or globe dystopia (Rha, J Craniofac Surg. 2013)
- Extraocular dysmotility and diplopia
- Superior orbital fissure or orbital apex syndrome
- Traumatic optic neuropathy
Historical perspective
- High-dose steroid therapy after optic nerve injury increased in the 1980s after the results of the National Acute Spinal Cord Injury Study II.
- Although some case studies have shown benefit from early high-dose corticosteroids, the International Optic Nerve Trauma Study (IONTS) completed in 1999 found that neither high-dose corticosteroids nor surgical intervention with optic canal decompression increased the probability of visual improvement (Levin, Ophthalmology. 1999).
References and additional resources
- AAO, Basic and Clinical Science Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2013-2014
- AAO, Focal Points: Management of Orbital Trauma: Fractures, Hemorrhage, and Traumatic Optic Neuropathy. Vol. 12, No. 7, 1994, p.6-11
- Bater MC, Ramchandani PL, Ramchandani M, Flood TR. An orbital apex fracture resulting in multiple cranial neuropathies. Br J Oral Maxillofac Surg. 2008 Mar;46(2):163-4
- Cho W, Ko AC, Eatamadi H, et al: Orbital and orbitocranial trauma from pencil fragments: Role of timely diagnosis and management. Am J Ophthalmol 2017; 180:46-54.
- Cossman JP, Morrison CS, Taylor HO, et al. Traumatic orbital roof fractures: Interdisciplinary evaluation and management. Plast Reconstr Surg. 2014 Mar;133(3):335e-43e
- Custer PL, Lind A, Trinkaus KM. Complications of supramid orbital implants. Ophthal Plast Reconstr Surg 2003;19:62–7
- Fulcher TP, Sullivan TJ. Orbital roof fractures: management of ophthalmic complications. Ophthal Plast Reconstr Surg. 2003 Sep;19(5):359-63
- Goldberg RA, Steinsapir KD. Extracranial optic canal decompression: indications and technique. Ophthal Plast Reconstr Surg. 1996 Sep;12(3):163-70
- Greenwald MJ, Boston D, Pensler JM, Radkowski MA. Orbital roof fractures in childhood. Ophthalmology 1989;96:491-496
- Hardy SP, Morales L Jr. Orbital roof and supraorbital ridge fractures. In: Holck DEE, Ng JD, eds. Evaluation and Treatment of Orbital Fractures: A Multidisciplinary Approach. Philadelphia: Elsevier Saunders; 2006:193-199
- Hink EM, Wei LA, Durairaj VD. Clinical features and treatment of pediatric orbit fractures. Ophthal Plast Reconstr Surg. 2014 Mar-Apr;30(2):124-31
- Jamieson KG, Yelland JDN. Surgical repair of the anterior cranial fossa because of rhinorrhoea, aerocele or meningitis. J Neurosurg. 1973;39:328–31
- Kim JW, Bae TH, Kim WS, Kim HK. Early reconstruction of orbital roof fractures: clinical features and treatment outcomes. Arch Plast Surg. 2012 Jan;39(1):31-5
- Koltai PJ, Amjad I, Meyer D, et al. Orbital fractures in children. Arch Otolaryngol Head Neck Surg 1995; 121:1375-79.
- Kubal WS. Imaging of orbital trauma. Radiographics. 2008 Oct;28(6):1729-39
- Kuppersmith RB, Alford EL, Patrinely JR, et al. Combined transconjunctival/intranasal endoscopic approach to the optic canal in traumatic optic neuropathy. Laryngoscope. 1997 Mar;107(3):311-5
- Lazaridis N, Makos C, Lordanidis S, Zouloumis L. The use of titanium mesh sheet in the fronto-zygomatico-orbital region. Case reports. Aust Dent J 1998;43;223–228
- Levin LA, Beck RW, Joseph MP, Seiff S, Kraker R. The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma Study. Ophthalmology. 1999 Jul;106(7):1268-77
- Manolidis S, Weeks BH, Kirby M, Scarlett M, Hollier L. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. J Craniofac Surg 2002;13;726–737
- Markovi€à MV, Brkljaci€à B, Ratkovi€à NA, et al. Posttraumatic cerebrospinal fluid cyst of the orbit. J Craniofac Surg 2006;17(1):189–191
- Martello JY, Vasconez HC. Supraorbital roof fractures: a formidable entity with which to contend. Ann Plast Surg. 1997 Mar;38(3):223-7
- Matsuzaki K, Enomoto S, Aoki T. Treatment of orbital roof blow-up fracture using a superior blepharoplasty incision. Orbit 2015; 34:166-71.
- McClurg FL, Swanson PJ. An orbital roof fracture causing diplopia. Arch Otolaryngol 1976; 102:497-8.
- Messinger A, Radkowski MA, Greenwald MJ, et al. Orbital roof fractures in the pediatric population. Plast Reconstr Surg 1989;84:213-6
- Miller GR, Tenzel RR. Ocular complications of mid-facial fractures. Plast Reconstr Surg 1967;39:37–42.
- Mokal NJ, Desai MF. Titanium mesh reconstruction of orbital roof fracture with traumatic encephalocele: a case report and review of literature. Craniomaxillofac Trauma Reconstr. 2012 Mar;5(1):11-8.
- Park RB, North VS, Rebhun CL, Belinsky I, Godfrey KJ, Tran AQ. Globe Compression by Bone Fragments in Orbital Blow-in Fractures: A Case Series and Systematic Review. Ophthalmic Plast Reconstr Surg. 2023 Mar-Apr 01;39(2):162-169.
- Pease M, Marquez Y, Tuchman A, et al. Diagnosis and surgical management of traumatic cerebrospinal fluid oculorrhea: case report and systematic review of the literature. J Neurol Surg Rep. 2013 Jun;74(1):57-66
- Rha EY, Joo HS, Byeon JH. Orbital dystopia due to orbital roof defect. J Craniofac Surg. 2013 Sep;24(5):e500-4
- Rubin PA, Bilyk JR, Shore JW. Orbital reconstruction using porous polyethylene sheets. Ophthalmology 1994;101;1697–1708
- Salame K, Segev Y, Fliss DM, Ouaknine GE. Diagnosis and management of posttraumatic oculorrhea. Neurosurg Focus 2000;9(1):e3
- Sofferman RA. An extracranial microsurgical approach to the optic nerve. J Microsurg. 1979;1:195-202
- Warner N, Eggenberger E. Traumatic optic neuropathy: a review of the current literature. Current Opinion in Ophthalmology. 2010. 21:459–462
- Wei LA, Kennedy TA, Paul S, et al. Traumatic orbital encepaloceles: Presentation and imaging. Orbit 2016; 35:72-7.
- Yu-Wai-Man P, Griffiths PG. Surgery for traumatic optic neuropathy (Review). Coch Collab 2009; 1:15–28
