Orbital varix
Updated May 2024
Vivian T. Yin, MD
Establishing the diagnosis
Etiology
- Vascular hamartoma
- Low-pressure, low-flow
- Thin walled and distensible with increase in venous pressure
Epidemiology
- No age or gender predilection
Clinical features
- Variable, intermittent proptosis associated with increase venous pressure (ie. bending, Valsalva). During episodes of proptosis can have associated discomfort or pain, nausea or blurry vision
- Optic neuropathy can occur in ~15% of patients (Duke-Elder, Textbook of Ophthalmology 1952; Song, Chinese Medical Journal 1979)
- Can have association with orbital wall defect or encephaloceles in 4.5% of cases (Islam, Ophthalmology 2004)
Imaging Modalities
- The mainstay of imaging used for diagnosis is dynamic CT or MRI scan with contrast. The hallmark is distensible mass with increase venous pressure, which can be elicited through Valsalva maneuver, pressure on ipsilateral neck veins or dependent head position with hyperextension of neck. [Figure 1]. (Shields, Wu, Am J Ophthalmol 1984; Chinese Medical Journal 1985)
- Historically, the presence of phlebolith on X-ray or CT can be useful for determining the etiology of an orbital varix from other masses, however, venogram was traditionally regarded as the gold standard for imaging a varix.
- Ultrasound using combination of A- and B-scan has been described to be diagnostic in 8 of 15 patients with vascular lesions of the orbit; however, all patients still required additional imaging with CT and/or MRI for management. (Ko, OPRS 2011)
- Alternative imaging modality with PET has been proposed as way to distinguish vascular from solid tumors of the orbit with 100% sensitivity and 86% specificity. (Polito, Arch Ophthalmol 2005)
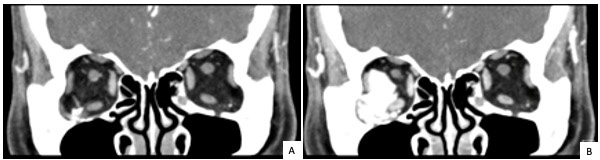
Figure 1
Differential diagnosis
- Lympho-venous malformation (lymphangioma)
- Cavernous hemangioma
- Carotid-cavernous fistula
Patient management: treatment and follow-up
Surgical Excision
- Approaches described include standard orbitotomy, craniotomy and option for endoscopic excision for medial apical lesions for prevention of compressive optic neuropathy as a surgical complication.
- For complex lesions, consideration for either pre- or intra-operative embolization to facilitate removal and decrease risk of hemorrhage.
- A lesion may be considered complex if apical, multi-cavitated, recurrent or wrapped around vital structures.
- Straight forward excision still standard choice for simple and/or anterior lesions
Embolization Approach and Materials
- The use of embolization alone has been described, however, for lesions of significant size or with compressive optic neuropathy, excision is required following embolization for resolution of proptosis and compression.
- For all approaches to embolization, there is a variety of materials described. Each material has different advantages and should be selected to maximize those advantages:
- Cyanoacrylate has been described with 1:1 mixture of lipiodized oil to have a 1 second set time for embolization with direct puncture approach to facilitate surgical removal (Tsai ASH, OPRS 2008)
- Use of microcoils with metallic materials (see below) has also been described as primary procedure without removal.
- Oxny, a non-adhesive embolic agent, has the advantage of its black color and rubber texture to help with dissection and is less inflammatory than cyanoacrylate if left in the orbit. In neurosurgical use, onyx has lower complication and higher initiation occlusion and durability. (Choo, Interv Neuroradiol 2016; Rabinov, Neurointerv Surg 2013)
- Percutaneous approach: Under general anesthesia with varix positioned in a dependent position. Under fluoroscopy and DynaCT, a low contrast CTA, the varix is accessed with percutaneous puncture. [Figure 2] (Couch, Am J Ophthalmol 2009)
- Difficult and high risk for damage to normal structures when the lesion is intraconal or apical
- Recurrence after percutaneous CT and fluoroscopy guided cyanoacrylate embolization was noted in 2 or 7 patients while 2 or 2 patients underlying direct resection by craniotomy had recurrence. (Mokhtarzadeh, Am J Ophthalmol 2004)
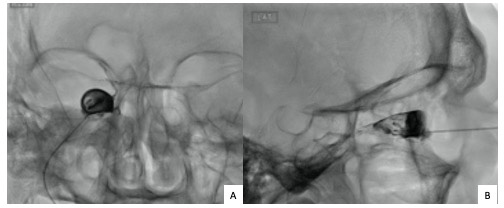
Figure 2
- Direct puncture: Surgical exposure through routine orbitotomy to expose one accessible face of the orbital varix. Direct puncture with a 27G or 25G hypodermic needle connected to an intravenous extension and a 3-way stopcock.
- Injection of contrast for a venography under fluoroscopy to define the feeding vessels. A small amount of fluid is typically withdrawn from the lesion before filling with the embolic material with fluoroscopy to check for amount of fill.
- Free tungsten microcoils requires introduction through multiple puncture at different orientation and dozens of coils to achieve complete filling. (Weill, AJNR Am J Neuroradiol 1998)
- Endovascular approach has been described for varix originating from the superior ophthalmic vein. Transfemoral venous heparin prior to catheterization of internal jugular vein with guide catheter to the superior ophthalmic vein and venous varix sac allowed neurocoils to be introduced for embolization. (Kumar, Indian J Ophthalmol 2015)
- Pre-operative angiogram may identify anastomosis between orbital vasculature and facial veins may allow for other vascular access point. (Mavilio, Interv Neurorad 2000)
Sclerotherapy
- Use of sclerotherapy such as bleomycin is more commonly described for lympho-venous malformation or lymphangiomas through a percutaneous route with 1-6 injections needed and an average decrease in size of lesion by 60% and improvement in proptosis by 65%. (Raichura, J AAPOS 2017; Hanif, Oribt 2018)
- The maximal intra-lesional dosage was 1U/kg per session and maximal cumulative dose of 150U. (Hanif, Oribt 2018)
Gamma Knife Radiation
- Range of radiation of 30-40Gy with stereotactic gamma knife radiation show resolution of primary orbital varices in 10 of 14 (71%) patients. At a median of 36 month follow-up, one patient, age 7, had side effect of retinal detachment. (Xu, Br J Ophthalmol 2011)
Preventing and managing treatment complications
- Bleomycin treatment has the acute effects of an inflammatory orbital response with mild pain, worsening of proptosis and transient hyperpigmentation of skin. (Raichura, J AAPOS 2017)
- Systemic side effect includes fever (55%), diarrhea (6%), vomiting (3%) and dyspnea (3%). (MacIntosh, Sem Ophthalmol 2014)
- Transvenous sclerotherapy with bleomycin for orbital varix has been described by Badlamudi et al. with 2 treatments with resolution on imaging at 6 months follow-up. (Vadlamudi, BMJ Case Reports 2016)
- Loss of vision can be related to inadvertent occlusion of or direct surgical damage to the ophthalmic or central retinal artery from retrograde fill of embolic material. Incidence is quoted at less than 15% historically but likely much lower today with proper technique. (Song, Chinese Medical Journal 1979; Leibocitch, Ophthalmol 2006)
- Vision loss from compressive optic neuropathy has also been reported with coiling of orbital varix. (Hwang, Orbit 2012)
- Diplopia secondary to paralysis of extraocular muscle is usually transient
Disease-related complications
- Acute thrombosis was believed to be associated with venous stasis, injury to vascular wall from inflammation, infection or trauma, or hypercoagulable. As noted by Bullock et al, characteristics of a “bull-neck” appears to be (Wade, BMJ Case Reports 2013; Bullock, Ophthalmol 1990) associated with risk of thrombosis, likely from venous stasis.
- Symptoms of acute thrombosis is less congestive as those in CCF but with acute proptosis, acute optic nerve compression, and/or increase IOP.
- Acute orbital hemorrhage occurs in less than 15% of cases and in 1 of 8 cases lead to visual sequela. (Kim, Jpn J Ophthalmol 2009; Lancey, Ophthalmology 1999)
- Compressive optic neuropathy can occur but is rare with 1/30 cases reported in series of distensible vascular malformation. (Lancey, Ophthalmology 1999)
References
- Islam N, Mireskandari K, Curton BJ, Rose GE. Orbital varices, cranial defects and encephaloceles. Ophthalmology 2004;111:1244-1247.
- Song G, Tian W, Qiang D. Surgical treatment of orbital varices. Chinese Medical Journal 1979;92:723-728.
- Duke-Elder S: Textbook of Ophthalmology, Vol 5, Kimpton, London 1952.
- Xu D, Liu D, Zhang Z, Zhang Y, Song G. Gamma knife radiosurgery for primary orbital varices: a preliminary report. Br J Ophthalmol 2011;95:1264-7.
- Ko F, DiBernardo CW, Oak J, Miller NR, Subramanian PR. Confirmation of and differentiation among primary vascular lesions using ultrasonography. Ophthal Plast Recosntr Surg 2011;27:431-5.
- Lancey B, Rootman J, Marotta TR. Distensible venous malformations of the orbit: Clinical and hemodynamic features and a new technique of management. Ophthalmol 1999;106:1197-1209.
- Kim Y-J, Kim Y-D. Orbital venous anomaly presenting with orbital hemorrhage. Jpn J Ophthalmol 2009;53:408-413.
- Wu E-H, Bai R-J, Zhang Y-T, Song G-X. CT with pressure exerted on neck veins in the diagnosis of primary orbital varices. 1985;98:287-8.
- Shields JA, Dolinskas C, Augsburger JJ, Shah HG, Shapiro ML. Demonstration of orbital varix with computed tomography and Valsalva maneuver. Am J Ophthalmology 1984;97:108-110.
- Mokhtarzadeh A, Garrity JA, Cloft HJ. Recurrent orbital varices after surgical excision with and without prior embolization with n-butyl cyanoacrylate. Am J Ophthalmol 2014;157:447-450.
- Couch SM, Garrity JA, Cameron D, Cloft HJ. Cyanoacrylate as an aid in surgical excision: Results of 4 case with histopathologic examination. Am J Ophthalmol 2009;148:614-618.
- Bullock JD, Goldberg SH, Connelly PJ. Orbital varix thrombosis. Ophthalmology 1990;97:251-6.
- Wade RG, Maddock RB, Ananth S. Orbital varix thrombosis: a rare cause of unilateral proptosis. BMJ Case Reports 2013 Jan 25.
- Weill A, Cognard C, Castaings L, Robert G, Moret J. Embolization of an orbital varix after surgical exposure. AJNR Am J Neuroradiol 1998;19:921-3.
- Kumar RR, Singh A, Singh A, Abhishek. Embolization of a deep orbital varix through endovascular route. Indian J Ophthalmol 2015;63(3):270-2.
- Raichura ND, Alam MS, Noronha VO, Mukherjee B. A prospective study of the role of intralesional bleomycin in orbital lymphangioma. J AAPOS 2017;21:146-151.
- Vadlamudi V, Gemmete JJ, Chaudhary N, Pandey AS, Kahana A. Transvenous sclerotherapy of a large symptomatic orbital venous varix using a microcatheter balloon and bleomycin. BMJ Case Reports 2016;8:e30.
- Hanif AM, Saunders JA, Hawkins CM, Wojno TH, Kim HJ. Use of percutaneous bleomycin sclerotherapy for orbital lymphatic malformation. Orbit 2018 Jun 14:1-7. [Epub ahead of print]
- Mavilio N, Pau A, Pisani R, Casasco A, Rosa M. Embolisationo f orbital varix via the superficial temporal vein. Interventional Neurorad 2000;6:137-140.
- Polito E, Burroni L, Pichierri P, Loffredo A, Vattimo AG. Preoperative diagnosis of cavernous hemangioma and other vascular orbital tumors. Arch Ophthalmol 2005;123:1678-1683.
- Tsai ASH, Fong KS, Lim W, Al Jajeh I, Chuah CT, Rootman J. Bilateral orbital varices: An approach to management. OPRS 2008;24:486-488.
- Rabinov JD, Yoo AJ, Ogilvy CS, Carter BS, Hirsch JA. Onyx versus n-BCA for embolization of cranial dural arteriovenous fistulas. J Neurointervent Surg 2013;5:306-310.
- Choo DM, Shankar JJ. Onyx versus nBCA and coils in the treatment of intracranial dural arteriovenous fistulas. Interv Neuroradiol 2016;22:212-6.
- Leibotvitch I, Modjtahedi S, Duckwiler GR, Golderg RA. Unsuccessful cannulation of the superior ophthalmic vein in the treatment of cavernous sinus dural fistulas. Ophthalmol 2006;113(7):1220-6.
- Hwang CS, Lee S, Yen MT. Optic neuropathy following endovascular coiling of an orbital varix. Orbit 2012;31(6):418-419.
