Periorbital Hollows
Updated January 2025
Introduction and surface anatomy
The traditional paradigm of plastic surgery is subtractive: tissue is removed to reduce puffiness.
- There is still a role for subtractive surgery in cases of puffy upper or lower eyelid.
Starting in the 1990s, there was increased recognition of the role of volume loss in the aging face (Figure 1).
Orbital aging can be conceptualized as the development of periorbital hollows (Figure 2)
Hollows occur in the areas of skin fixation to bone (Goldberg, Plast Reconstr Surg 2005 and Goldberg, McCann, Plast Reconstr Surg 2005) (Figures 3 and 4).
- The orbital rim hollow (including the medial portion, the “tear trough” hollow) occurs in the area of the orbital rim ligament.
- Another hollow forms along the zygomatic ligament, at the origin of the zygomatic muscles. Between the orbital rim and zygomatic attachments forms the malar triangle, a potential space that can contain edema and form a fluid containing mound.
The periorbital hollow extends to the superior orbital rim. Particularly in the East Asian patient, this leads to unveiling of the frontal bone, and elongation of the tarsal platform (deepening of the superior sulcus) (Figure 5).

Figure 1. Aging changes are characterized by deflation, with loss of volume along the superior and inferior orbital rim.
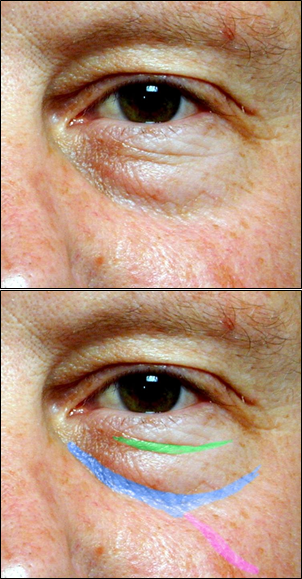
Figure 2. This patient has some fullness of the inferior orbital fat, and might be improved with fat removal, but he will get a more natural and effective rejuvenation if we recognize and treat the periorbital hollows. Blue: orbital rim hollow. Purple: Zygomatic hollow. Green: Septal confluence hollow.
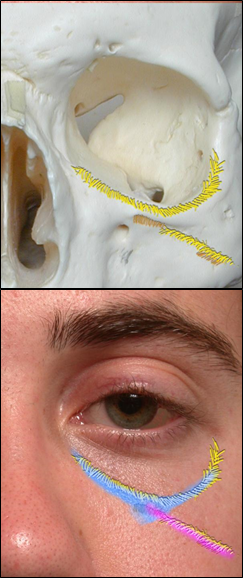
Figure 3. Volume loss occurs in areas of deep ligamentous attachments from bone to skin, particularly the orbital rim ligament (blue) and zygomatic ligament (purple).

Figure 4. The malar triangle is a potential space that can fill with boggy edema, bound by the orbital rim ligament (blue) and the zygomatic ligament (purple).

Figure 5. Filling the superior orbital hollow. 39-year-old woman with hollow superior orbital rim, before and after 1-ml Restylane filling.
History
It is important to elicit a history of previous surgical and nonsurgical treatments including fillers or neurotoxin injections.
A history of thyroid disorder should be sought.
A history of allergies, tendency for episodic edema, dermatitis, or rosacea, vasculitis, or autoimmune disease should be sought.
Risk factors
Relatively small maxilla predisposes to deeper orbital rim hollow.
Thin skin (congenital, or with aging) unveils the orbital rim hollow.
Differential diagnosis
The hollow forms between the full orbital fat and the cheek fat. In some cases, the orbital fat is so puffy that reducing the fullness (blepharoplasty) is the most appropriate treatment.
The cheek fat probably does not descend as much as it deflates (Lambros, Plast Reconstr Surg 2007 and Lambros Clin Plast Surg 2008), however in some cases, there is an element of midface descent, so that midface lifting is appropriate to elevate the malar fat into the orbital rim hollow.
Patient management
Blepharoplasty with fat removal
Fat removal alone may allow some improvement in periorbital hollows. In particular, a full lateral fat pad can cause the “Charlie Brown” lateral orbital hollow, and debulking the fat can lessen the appearance (Figure 6). However, fat removal alone does not address the hollow itself.

Figure 6. The lateral “Charlie Brown” hollow forms between the lateral orbital fat pad and the adjacent malar fat. Upper: Debulking the puffy lateral fat pad with blepharoplasty will improve the contour, here combined with midface lift. Lower: another treatment option is to fill the hollow using a conservative, feathered pattern.
Blepharoplasty with fat transposition
The medial and central fat pads of the lower eyelid can be repositioned over the orbital rim. This effectively addresses the contour by reducing the fullness of the fat and simultaneously filling the adjacent tear trough and orbital rim hollow.
A transcutaneous approach has been described by Hamra (Plast Reconstr Surg 2004) and others, but is less often used by oculofacial specialists.
A transconjunctival approach allows the fat pads to be isolated and converted into pedicles. When creating the fat pedicles, the surgeon should find a balance between adequate release to disengage the pedicles from the orbital motility system and excessive release to preserve maximal blood supply to the pedicle.
The fat can be transposed into a subperiosteal plane (Goldberg, Plast Reconstr Surg 2000). The subperiosteal plane is easily dissected, relatively blood free, and provides maximal tissue coverage over the pedicle. Technical points include releasing the levator labii superioris, and preserving the infraorbital neurovascular bundle.
Alternatively the fat can be transposed into a submuscular (SOOF) plane. This plane can be more bloody and sometimes more difficult to define. The submuscular plane may have the advantage of releasing the orbital rim ligament, allowing the orbicularis to elevate and perhaps effacing the eyelid-cheek junction (Mohadjer OPRS 2006 and Yoo, JAMA Fac Plast Surg 2013).
Fixation of the pedicle can be accomplished with a buried suture (more difficult to place) or a suture externalized to the cheek skin (easier to place, but potentially annoying to the patient).
Filling periorbital hollows
Synthetic fillers are the workhorse for periorbital filling (Kane, Aesth Plast Surg 2005; Goldberg OPRS 2006; Goldberg, Aesth Surg J 2006; Lambros, Plast Reconstr Surg 2007; Berros, Plast Reconstr Surg 2013).
- Hyaluronic acid gels are well tolerated, relatively safe, and predictable.
- Calcium Hydroxyapatite fillers are trickier because they cannot be dissolved, the white material can show below thin skin, and lumps or contour problems are not easily treated.
- PLLA fillers are less predictable in the periorbital area and not commonly used.
- Permanent fillers have substantial risk and most experts recommend against their use.
The periorbital area is tricky for filling because the skin is thin and the 3-dimensional contours are complicated.
- If patients can avoid blood thinners such as aspirin for several weeks before the procedure, bruising may be lessened.
- Consent should include discussion of rare catastrophic risks including loss of vision or stroke.
- Although the actual risk is low, most practitioners will not administer fillers to pregnant patients.
- Strong topical anesthetics are useful to improve the comfort of the procedure: particularly for cosmetic treatments, patients should not experience pain. Handholding, distraction techniques, music, aromatherapy, and warm engagement by all staff are examples of measures that can improve the patient experience.
- Sterile preparation of the skin is appropriate because the filler represents an implanted device and there is a risk of biofilm formation. Options include alcohol, chlorhexidine, and betadine.
- Small volumes of filler (sometimes less than 0.5ml per side) and a careful, detailed, feathered pattern of filling are important (Figure 7).
- The filler should be placed deep to the orbicularis oculi muscle, adjacent to the bony rim.
- The practitioner and assistant should be alert to hematoma formation, which is addressed with immediate firm pressure over the bleeding vessel, held for at least 90 seconds, to reduce bruise formation.
- Some practitioners use a blunt cannula in order to reduce bruising and perhaps decrease the risk of intra-arterial injection.
- After the procedure, the patient can resume normal activities. It may be prudent to avoid heavy massage or pressing on the area for one week.
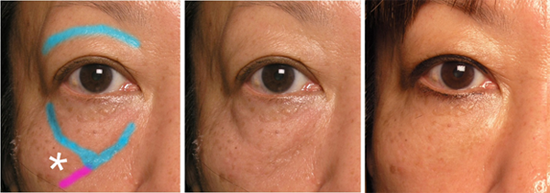
Figure 7. Patient before and after filling the periorbital hollows, 1ml Restylane split between the sides. Blue: orbital rim hollow. Purple: Zygomatic hollow.
Follow-up is generally in 3–6 months, although new patients may benefit from an early post-treatment visit to help with bonding and positive reinforcement.
- The hyaluronic acid gel fillers can last a long time in the periorbital area, sometimes even years. As the effect fades, patients are candidates for maintenance injections.
Periorbital fat injections
Periorbital fat injections are another option for filling. The thin skin of the periorbital region is prone to lumpiness and contour irregularities, which can be very difficult to treat. Therefore periorbital fat transfer should be performed with optimal surgical technique, and in patients who have some tolerance for complications.
Complications
The nightmare risk of injectable fillers is stroke or blindness, related to intra-arterial embolization into the internal carotid circulation.
- Based on reported cases, areas of particular danger are in the midline: glabella and nasal injections have higher risk. However, blindness has been reported from temple injections as well, and in theory there is risk for any injection location (Cohen, Aesth Surg J 2015; Hwang, OPRS 2015).
- The mechanism of blindness is presumed to relate to intra-arterial injection, which allows the filler to travel (upstream or downstream depending on the patient’s vascular anatomy) from the external carotid circulation into the internal carotid circulation).
- Prevention may not be possible in every case. Reasonable precautions include avoiding known vessels, reflux of the syringe (when possible, based on the type of filler), slow injection, moving the needle during injection, and stopping immediately if severe pain is reported by the patient.
- There have not been reported cases of successful treatment of retinal or cerebral embolization. Experimental treatments include anticoagulants, hyperbaric oxygen, and direct injection of hyaluronidase either intra-arterial (interventional radiology) or intraocular.
Early swelling can occur. This early swelling may relate to needle trauma or filler reaction, and subsides over the first week. Salt restriction, cool compress, and occasionally a short course of corticosteroids, can be used.
Blue-grey dyschromia (incorrectly ascribed to the Tyndall effect (Rootman, OPRS 2014) can occur in the medial orbital rim hollow (tear trough) (Figure 8). It is more common in patients with thin, translucent skin, and may be exacerbated by pre-existing allergic-type dark circles. Treatments to thicken the skin, such as exfoliants, laser, or peel, may be helpful.
Enhancement of malar triangular fluid mounds may occur early, or late, after hyaluronic acid gel filling. Patients who have a problem with periorbital edema are generally not good candidates for hyaluronic acid gels. In these patients, a “drier” filler such as calcium hydroxyapatite can be considered.
Late boggy fullness of the orbital rim (“ridge formation”) can occur months or even years after the injection. (Figure 9). This usually responds to dissolving the filler with hyaluronidase, sometimes over several treatments of 30–150 units per session.
Lumps and contour problems can appear with any filler in any area, but the periorbital region is particularly difficult. Sometimes these will improve over time. A focal fullness can sometimes be reduced with firm pressure directly over the area, for example using a cotton tip applicator. Filling around a lump or mound can sometimes camouflage it. In severe cases, it is best to dissolve all of the filler with hyaluronidase, and start over.

Figure 8. Blue grey dyschromia, 2 years after periorbital hyaluronic acid gel injections
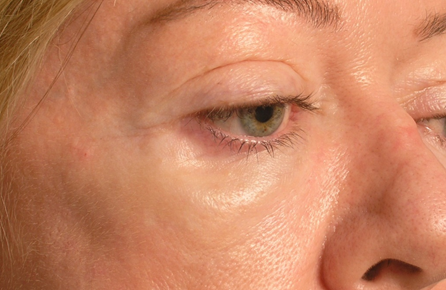
Figure 9 Late boggy edema, 1 year after periorbital hyaluronic acid gel injections.
References and additional resources
- Berros P, Lax L, Bétis F. Hyalurostructure treatment: superior clinical outcome through a new protocol-a 4-year comparative study of two methods for tear trough treatment. Plast Reconstr Surg. 2013 Dec;132(6):924e-31e.
- Cohen JL, Biesman BS, Dayan SH, DeLorenzi C, Lambros VS, Nestor MS, Sadick N, Sykes J. Treatment of Hyaluronic Acid Filler-Induced Impending Necrosis With Hyaluronidase: Consensus Recommendations. Aesthet Surg J. 2015 May 10.
- Goldberg RA. Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg. 2000 Feb;105(2):743-8; discussion 749-51.
- Goldberg RA. The three periorbital hollows: a paradigm for periorbital rejuvenation. Plast Reconstr Surg. 2005 Nov;116(6):1796-804. Erratum in: Plast Reconstr Surg. 2006 Jan;117(1):349. PubMed PMID: 16267452.
- Goldberg RA, Fiaschetti D. Filling the periorbital hollows with hyaluronic acid gel: initial experience with 244 injections. Ophthal Plast Reconstr Surg. 2006 Sep-Oct;22(5):335-41; discussion 341-3.
- Goldberg RA. Nonsurgical filling of the periorbital hollows. Aesthet Surg J. 2006 Jan-Feb;26(1):69-71.
- Goldberg RA, McCann JD, Fiaschetti D, Ben Simon GJ. What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg. 2005 Apr 15;115(5):1395-402; discussion 1403-4.
- Hamra ST. The role of the septal reset in creating a youthful eyelid-cheek complex in facial rejuvenation. Plast Reconstr Surg. 2004 Jun;113(7):2124-41; discussion 2142-4.
- Hwang CJ, Morgan PV, Pimentel A, Sayre JW, Goldberg RA, Duckwiler G. Rethinking the Role of Nitroglycerin Ointment in Ischemic Vascular Filler Complications: An Animal Model With ICG Imaging. Ophthal Plast Reconstr Surg. 2015 Mar 18. Epub ahead of print
- Kane MA. Treatment of tear trough deformity and lower lid bowing with injectable hyaluronic acid. Aesthetic Plast Surg. 2005 Sep-Oct;29(5):363-7.
- Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg. 2007 Oct;120(5):1367-76; discussion 1377.
- Lambros V. Models of facial aging and implications for treatment. Clin Plast Surg. 2008 Jul;35(3):319-27; discussion 317.
- Lambros VS. Hyaluronic acid injections for correction of the tear trough deformity. Plast Reconstr Surg. 2007 Nov;120(6 Suppl):74S-80S.
- Mohadjer Y, Holds JB. Cosmetic lower eyelid blepharoplasty with fat repositioning via intra-SOOF dissection: surgical technique and initial outcomes. Ophthal Plast Reconstr Surg. 2006 Nov-Dec;22(6):409-13.
- Rootman DB, Lin JL, Goldberg R. Does the Tyndall effect describe the blue hue periodically observed in subdermal hyaluronic acid gel placement? Ophthal Plast Reconstr Surg. 2014 Nov-Dec;30(6):524-7.
- Yoo DB, Peng GL, Massry GG. Transconjunctival lower blepharoplasty with fat repositioning: a retrospective comparison of transposing fat to the subperiosteal vs supraperiosteal planes. JAMA Facial Plast Surg. 2013 May;15(3):176-81.
