Pleomorphic adenoma
Updated July 2024
Establishing the diagnosis
Etiology
- Oncogenetic origin is unknown.
- Histology is characterized by involvement of epithelial and myoepithelial structures.
- Myoepithelial cells are contractile elements in the gland.
- Metallothionein is a cysteine-rich protein found in benign and malignant myoepithelial neoplasms; it might play a role in altering the pattern of apoptosis in these tumors (Viana 2013).
Epidemiology
- Most commonly presents in the fourth and fifth decade
- Pleomorphic adenoma is a head and neck tumor, and is the most common benign neoplasm of both the major and minor salivary glands.
History
- Slowly developing (> 1 year) proptosis or globe displacement
- Nonpainful enlargement of the lacrimal gland
Clinical features
- Globe displaced inferiorly and medially
- Tumors that arise in the palpebral lobe of the lacrimal gland present earlier than orbital tumors (Rose 1992).
- Pleomorphic adenoma has been reported in the eyebrow, upper eyelid, lateral and medial lower eyelid, lacrimal sac, and even intraocularly (Obi 2013).
- Recurrent benign pleomorphic adenoma can be multifocal and multinodular and can present multiple times after incomplete primary resection before developing malignant transformation (McNab 2011).
- Average time to malignant transformation is estimated to be 15–20 years (Font 1978).
- Recurrent pleomorphic adenoma, even without malignant transformation, can cause local morbidity such as compressive neuropathy (Benoit 2010).
Testing
- CT scan (Figure 1) and MRI demonstrate a well-circumscribed mass with pressure remodeling of the lacrimal fossa that can indent globe.
- In about a third of malignant lacrimal gland tumors, calcification is evident in a stippling patter; in benign tumors, calcification is less common and more localized and dense. Therefore, diffuse calcification raises the index of suspicion for malignancy and lowers the threshold for incisional biopsy (Wright 1992).
- Establishing a diagnosis of pleomorphic adenoma is unusual in that incisional biopsy is avoided to prevent possible tumor spillage and seeding, which can lead to recurrence after excision.
- Therefore the diagnosis is established on clinical grounds.
- After complete excision of an encapsulated mass, with the capsule intact, the diagnosis of pleomorphic adenoma can be confirmed by histopathology.
- Definitive management is complete surgical excision, which can be performed by anterior or lateral orbitotomy, depending on the size and location of the tumor.
- The cues that allow for clinical diagnosis include:
- Color: It is white versus pink, which would suggest a lymphoid tumor.
- Location: It can be seen as contiguous with and adjacent to the normal lacrimal gland
- Consistency: It is solid without a lobular gland-like appearance.
- Encapsulation (or pseudocapsule): It is surrounded by a glistening surface, which should not be violated.
- Definitive excision with the capsule intact is the goal of surgery even if the mass is fairly large.
- In the pre-CT era, John Wright proposed an approach to differentiating between benign and malignant lacrimal gland tumors based on duration of symptoms — benign tumors slowly enlarge over a period of at least one year — and presence of pain — painless growth implies benign tumor (Wright 1979).
- In a review of 78 patients treated at Moorfields Eye Hospital from 1968 to 1990 for pleomorphic adenoma, 89% (63 tumors) were correctly diagnosed prior to surgery, based on these clinical and radiographic characteristics (Rose 1992).
- Eight patients among those 78 had symptoms for less than 1 year and 4 had pain, leading to a misdiagnosis.
- Eight patients among those 78 had palpebral lobe tumors, and presented with clinical evidence of tumor for less than 1 year.
- Among six palpebral lobe lacrimal gland tumors treated at the University of British Columbia from 1982 to 1995, only 3 were pleomorphic adenomas. The malignant tumors included an adenoid cystic carcinoma and 2 malignant transformations of pleomorphic adenoma. The index of suspicion should be different for a palpebral lobe tumor (Vangveeravong 1996).
- Proponents of incisional biopsy assume that the risk of tumor seeding is outweighed by the advantage of establishing the diagnosis (Tse 1988).
- Pleomorphic adenoma gene 1 rearrangement is well known in pleomorphic adenoma with alterations can be seen in cases of carcinoma ex pleomorphic adenoma
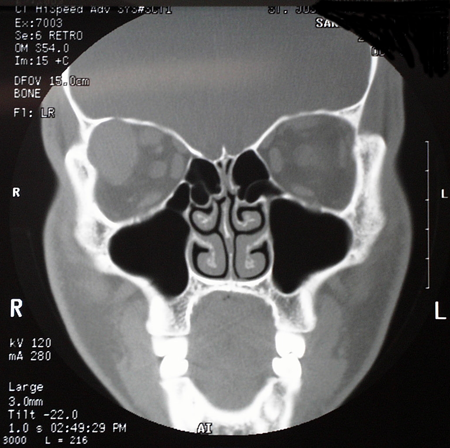
Figure 1. Pleomorphic adenoma CT. Courtesy Robert G. Fante, MD, FACS.
Testing for staging, fundamental impairment
There is no staging needed for this benign tumor.
Risk factors
- Fourth to fifth decade
- No other known risk factors
Differential diagnosis
- Inflammatory lesions of lacrimal gland
- Idiopathic orbital inflammation
- Sjögren syndrome
- Sarcoid
- Mumps
- Tuberculosis
- Lymphoid lesions
- Benign reactive lymphoid hyperplasia
- Atypical lymphoid hyperplasia
- Lymphoma
- Epithelial tumors
- Malignant mixed tumor of the lacrimal gland
- Adenoid cystic carcinoma
Patient management: treatment and follow-up
Natural history
This is a slow-growing tumor until malignant transformation occurs.
Medical therapy
- In the salivary gland, HER2/neu overactivity has been observed with malignant transformation carcinoma ex pleomorphic adenoma, therefore HER2 based therapy might be effective when medical treatment is needed (Sharon 2010). It has not yet been studied in orbital tumors.
- Trastuzumab (Herceptin) is a monoclonal antibody that competitively binds to the plasma membrane HER2 receptor.
Radiation
Cases of multinodular recurrent benign pleomorphic adenoma can be treated with radiotherapy, in addition to surgery or if surgical excision is impractical.
Surgery
Although excisional biopsy is the accepted standard of care there are advocates of limited preliminary biopsy prior to excision to confirm the diagnosis (Lai 2009).
- The theory behind incisional biopsy is that management can be changed by recognizing an alternative diagnosis.
- Incisional biopsy might be most appropriate when the lesion is not amenable to simple removal, without affecting tissues other than the lacrimal gland.
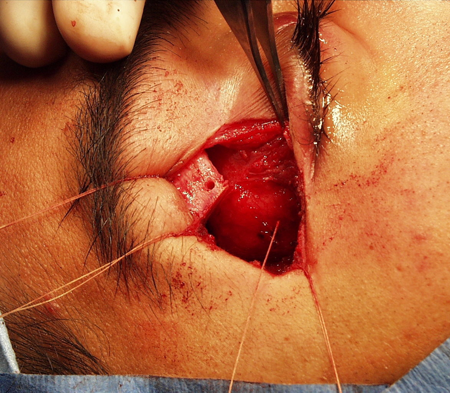
Figure 2. Bone flap for pleomorphic adenoma. Courtesy Robert G. Fante, MD, FACS.
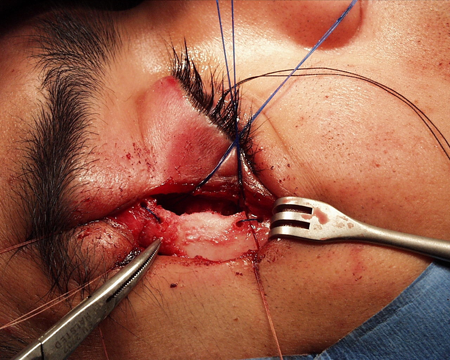
Figure 3. Bone flap replaced. Courtesy Robert G. Fante, MD, FACS.
Other management considerations
- Secondary excision if tumor has been left behind focuses similarly on dissection along the encapsulated surface
- Wide tumor free margins might be needed to assure complete excision and avoid malignant transformation.
Common treatment responses, follow-up strategies
Once complete excision has been accomplished with the capsule intact, there should be no risk of continued tumor growth.
Preventing and managing treatment complications
- Aside from recurrence, concern centers on morbidity from the excision, including dry eye from trauma to the lacrimal gland or its ductules.
- When the tumor arises in the palpebral lobe, disruption of the lacrimal gland ductules during resection might be unavoidable (Rose 1992).
Disease-related complications
Although it has not been described in pleomorphic adenoma of the lacrimal gland, there is an unusual, extremely rare feature of pleomorphic adenoma in the head and neck region with solitary metastases (e.g., kidney, liver, lung) seen even with benign histology of the primary tumor (Diagnost Cytopathol 2009). These are called benign metastasizing pleomorphic adenoma and are usually associated with locally recurrent tumors.
Historical perspective
- The term “mixed tumor” was introduced by Minssen in 1874 (Davies 1954).
- Case reports of mixed tumor in the lacrimal gland date back as far as 1598.
- Warthin in 1901 suggested that the histopathology of these tumors in the lacrimal gland was similar to the salivary gland tumors (Warthin 1901).
References and additional resources
- Asahina M, Saito T, Hayashi T, Fukumura Y, Mitani K, Yao T. Clinicopathological effect of PLAG1 fusion genes in pleomorphic adenoma and carcinoma ex pleomorphic adenoma with special emphasis on histological features. Histopathology. 2019 Feb;74(3):514-525. doi: 10.1111/his.13759. Epub 2018 Dec 2. PMID: 30307055.
- Benoit MM, Handzel O, McKenna MJ, Deschler DG. A 42-year-old man with facial nerve weakness and multiple recurrent pleomorphic adenoma. Otology & Neurotology. 2010;31(7):1157-1159.
- Davies WS. Pleomorphic adenoma and adenocarcinoma of the lacrimal gland, with report of thirteen cases. Trans Am Ophthalmol Soc. 1954-1955;52:467-496.
- Font RL, Gamel JW. Epithelial tumors of the lacrimal gland: an analysis of 265 cases. In: Jakobiec FA, ed. Ocular and Adnexal Tumors. Birmingham, AL: Aesculapius; 1978:787–805.
- Lai T, Prabhakran VC, Malhotra R, Selva D. Pleomorphic adenoma of the lacrimal gland: Is there a role for biopsy? Eye (Lond). 2009; 23(1):2-6.
- McNab A, Satchi K. Recurrent lacrimal gland pleomorphic adenoma: Clinical and computed tomography features. Ophthalmology. 2011;118(10):2088-2092.
- Obi E, Drummond S, Kemp E, Roberts F. Pleomorphic adenoma of the lower eyelids: a case series. Ophthal Plast Reconstr Surg. 2013;29(1):e14-e17.
- Rose GE, Wright JE. Pleomorphic adenoma of the lacrimal gland. Br J Ophthalmol. 1992;76(7):395-400.
- Sharon E, Kelly RJ, Szabo E. Sustained response of carcinoma ex pleomorphic adenoma treated with trastuzumab and capecitabine. Head Neck Oncol. 2010;2:12.
- Tse DT, Folberg R. Technique for incisional biopsy of a lacrimal gland mass when the diagnosis of benign mixed tumor cannot be excluded clinically. Ophthalmic Surg. 1988;19(5):321-324.
- Vangveeravong S, Katy SE, Rootman J, White V. Tumors arising in the palpebral lobe of the lacrimal gland. Ophthalmology. 1996;103(10):1606-1612.
- Viana ADM, Ribeiro DC, Florencio TNG, et al. Immunihistochemical expression of metallothionein in pleomorphic adenoma of minor salivary glands: A role in the control of apoptosis? Acta Histochemica. 2013;115(6):564-568.
- Warthin AS. A case of endothelioma of the lacrimal gland. Arch Ophthalmol 1901;30:601.
- Wright JE, Stewart WB, Krohel GB. Clinical presentation and management of lacrimal gland tumours. Br J Ophthalmol. 1979;63(9):600
- Wright JE, Rose GE, Garner A. Primary malignant neoplasms of the lacrimal gland. Br J Ophthalmol. 1992;76(7):401-407.
- Zhang Y, Gomez-Fernandez CR, Jorda M, Ganjei-Azar P. Fine needle aspiration (FNA) and pleural fluid cytology diagnosis of benign metastazing pleomorphic adenoma of the parotid gland in the lung: a case report and review of the literature. Diagn Cytopathol. 2009;37(11):828-831.
