Rhytidectomy (Facelift)
Updated August 2024
Natalie Homer; Tanuj Nakra
Goals, indications, contraindications
The Aging Face
Facial aging is a dynamic process that results from simultaneous deterioration of skin texture and tone, volume depletion, and gravitational descent. An anatomic understanding of the factors contributing to facial maturation enables the cosmetic surgeon to direct intervention toward restoring to a more youthful state.
Age-related skin changes may be influenced by ethnicity, genetics, hormonal shifts and environmental exposures. Atrophy of the dermal extracellular matrix and damage by oxidative stress lead to loss of elasticity and architectural irregularity (Mendelson), appearing clinically as rhytids, skin laxity and dyspigmentation. Smoking may accelerate cutaneous aging changes by 10-20 years (Mendelson). The Glogau classification system may be used to quantify photoaging (Figure 1). Skin rejuvenation may be performed with use of chemical peels or ablative laser resurfacing.
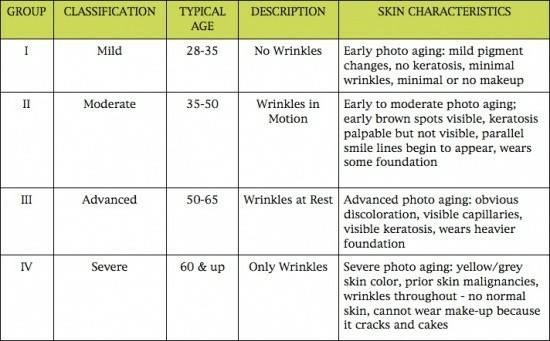
Figure 1. Glogau classification of photoaging
Figure credit: Bostonbeautyblog.com
Facial volume loss occurs from a combination of fat depletion, muscle atrophy and skeletal resorption. Generally, there is preferential deflation of the deep facial fat pads, including the suborbicularis oculi fat pad and deep malar fat pads of the midface, and the buccal fat pad of the lower face (Wan et al). This loss of support for superficial soft tissues results in overlying soft tissue descent. Bony resorption in the midface is particularly evident in the anterior maxilla and infraorbital rim, contributing to the tear trough deformity and negative vector of the globe. Deep volume restoration can be achieved with use of fillers, autologous grafts or allogenic implants.
Finally, gravitational descent plays a key role in facial aging. The zygomatic and orbital retaining ligaments divide the mid-face into the lower eyelid, malar and nasolabial segments (Figure 2– Mendelson). Gravitational descent of skin and midface fat pads across these ligaments leads to the infraorbital hollowing, deepening of the tear trough, and accentuation of the nasolabial fold (Figure 3). In the lower face, the masseteric and mandibular retaining ligaments provide a tether over which soft tissue descends, including the buccal fat pad, leading to a visible labiomandibular fold and jowl. Fat accumulation in the lower face leads to an inferiorly widened, pear-shape appearance. Gravitational changes are best addressed with facelifting (rhytidectomy) surgery.
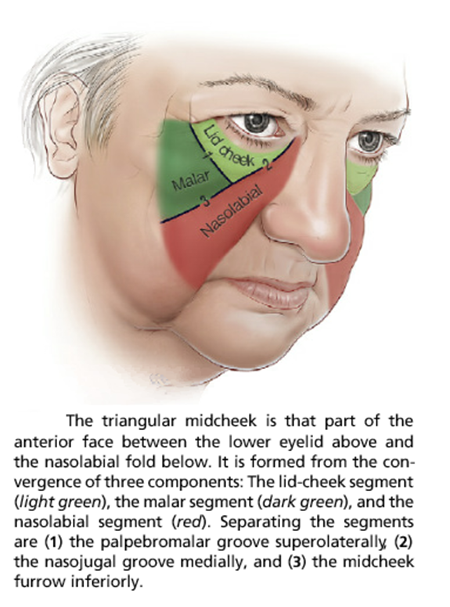
Figure 2. Midcheek anatomic components, including the lid-cheek segment (light green), malar segment (dark green) and nasolabial segment (red), separated by the (1) palpebromalar groove, (2) nasojugal groove, and (3) midcheek furrow.
Figure credit: Mendelson B, Wong C. Chapter 6.1: Facelift: Facial anatomy and aging. Aesthetic Surgery of the Face.
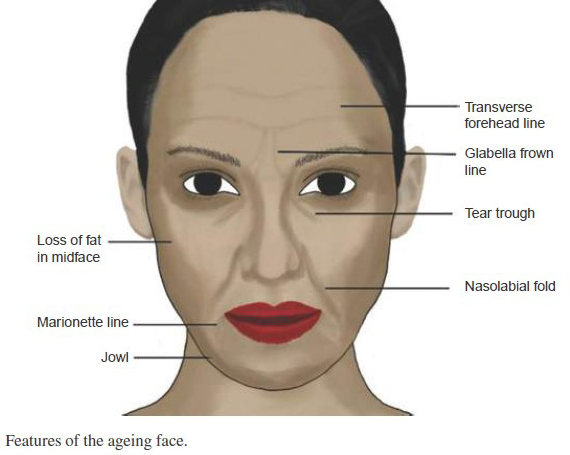
Figure 3. The Aging Face
Figure credit: Kanapathy M, Kirkpatrick N. Chapter 16: Facial Aesthetic Surgery. Textbook of Plastic and Reconstructive Surgery.
Contraindications
As rhytidectomy is an elective, invasive surgical procedure, potential candidates should be verified to be in good health. Smoking cessation for a minimum of 3 months prior to surgery is an absolute requirement, as flap necrosis has been seen to have 10-12-fold increase in tobacco users. Serum testing for cotinine, a metabolic byproduct of nicotine, can be performed to confirm patient compliance. Medical conditions which may adversely affect optimal healing, such as vasculitis, autoimmune disease, and history of face or neck radiation, are also contraindications. Importantly, patients with unreasonable or unrealistic expectations should also be deterred from pursuing cosmetic surgery.
Relevant Anatomy
Soft Tissue Layers and the SMAS
A comprehensive 3-dementional familiarity with mid and lower facial anatomy is essential for the facial cosmetic surgeon. The facial soft tissue consists of five basic concentric layers: skin, subcutaneous tissue, superficial musculoaponeurotic system (SMAS), loose areolar tissue (including retaining ligaments and potential space), and deep fascia. The SMAS layer plays a particularly key role in facelifting surgery. The SMAS is a fibromuscular sheath which envelops the facial mimetic muscles responsible for facial expression. This layer is continuous with the platysma in the neck, temporoparietal fascia of the temple and galea aponeurosis of the forehead. The SMAS may be divided into its mobile portion in the temple and medial mid and lower face regions, and its immobile portion overlying the parotid gland. The SMAS also varies in thickness, with thinnest segments overlying the malar and masseter regions. Manipulation of this fibromuscular layer allows for robust and enduring correction of gravitational descent during rhytidectomy.
Ligaments
The tethering effect of facial retaining ligaments leads to the cosmetically bothersome folds observed in in the aged face. The true osteocutaneous ligaments, extending from the periosteum to skin, include the zygomatic, masseteric and mandibular ligaments. The zygomatic ligament widens over the body of the zygoma, an area known as McGregor’s patch, and projects through the malar fat pad to interdigitate cutaneously. Progressive laxity of these ligaments, coinciding with overlying soft tissue descent, leads to the accentuated appearance of the nasolabial fold, melolabial fold and jowl. Release of these ligaments is essential to SMAS elevation. Fascial retaining ligaments include the lateral orbital and temporal ligaments, and are infrequently manipulated in isolated lower face rhytidectomy.
Muscles
The facial mimetic muscles produce dynamic facial expression. Nearly all of these muscles receive motor innervation on their deep surfaces, thus allowing for safe surgical dissection along their anterior fibers. These muscles include the orbicularis oculi, zygomaticus major and minor, orbicularis oris, levator labii superioris, risorius, and depressor anguli oris. The deep mimetic muscles, the buccinator, levator anguli oris and mentalis, are conversely innervated on their superficial surfaces, and should not be manipulated along this plane to avoid nerve disruption.
Motor Nerves
The facial nerve (CN VII) provides somatic innervation to the facial mimetic muscles. This motor nerve exits the stylomastoid foramen and divides into an upper and lower trunk within the parotid gland. Five nerve branches subsequently arise: the temporal (or frontal), zygomatic, buccal, marginal mandibular and cervical branches (Figure 4). The temporal branch exits the parotid gland superiorly, coursing over the periosteum of the middle one-third of the zygomatic arch, passing within the superficial fascia over the temporalis fossa to ultimately innervate the frontalis, corrugator supercilii, and superior portion of the orbicularis oculi. The course of the temporal nerve branch can be estimated by the imaginary Pitanguy line extending from a point 0.5 cm inferior to the tragus to a point 1.5 superior to the lateral tail of the brow (Figure 5). The zygomatic branch exits superolaterally and travels along the inferior border of the zygomaticus muscles, innervating the zygomaticus major and minor, procerus, inferior orbicularis oculi, procerus, nasalis (alar portion), levator labii superioris aleque nasi and levator anguli oris on their posterior surfaces. The buccal branches course medially within the masseteric fascia to innervate the lip and mouth elevators, including the orbicularis oris, the buccinator, as well as the transverse portion of the nasalis. While buccal branches are the most common to be injured during facelifting surgery, significant nerve arborization of both the zygomatic and buccal branches generally safeguards against long-lasting paralysis. The marginal mandibular nerve trajectory can be the most variable. In a majority of cases, this nerve branch courses anteriorly above the border of the mandible in a layer deep to the masseteric fascia. However, cadaveric studies have confirmed occasional trajectory below the inferior mandibular border. The nerve penetrates the deep cervical fascia and travels in a sub-platysmal plane, crossing anterior to the facial artery and vein near the mandibular border at a position average 3 cm anterior to the mandibular angle. The nerve branch subsequently courses through the buccal space to innervate the lip depressors. The cervical branch exits the parotid inferiorly, coursing deep to the platysma to provide motor innervation to this muscle, essential for oral commissure depression and neck contraction.
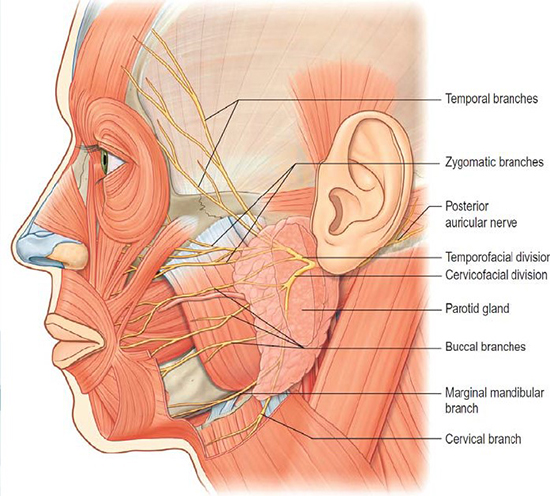
Figure 4. Facial nerve branches
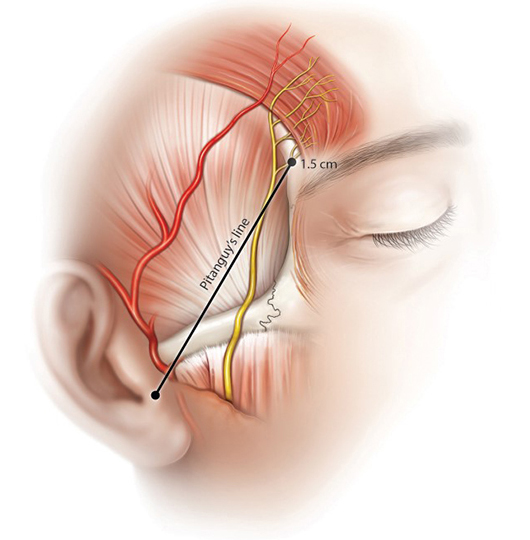
Figure 5. Pitanguy Line
Figure credit: https://plasticsurgerykey.com/4-frontal-branch-of-the-facial-nerve/
Sensory Nerves
The great auricular nerve is the most common nerve to be injured during facelifting surgery. This nerve provides sensory innervation to the ear lobule, concha and posterior auricle. The nerve travels beneath the superficial cervical fascia, and is particularly prone to injury as it exits the posterior border of the sternocleidomastoid muscle where platysma is absent. The nerve crosses the sternocleidomastoid anteriorly at McKinney’s point, approximately 6.5 cm inferior to the external auditory canal (Figure 6). The nerve courses between the lesser occipital nerve (posteriorly) and the external jugular vein (anteriorly), and thus serves as a landmark for identifying and avoiding injury to these structures.
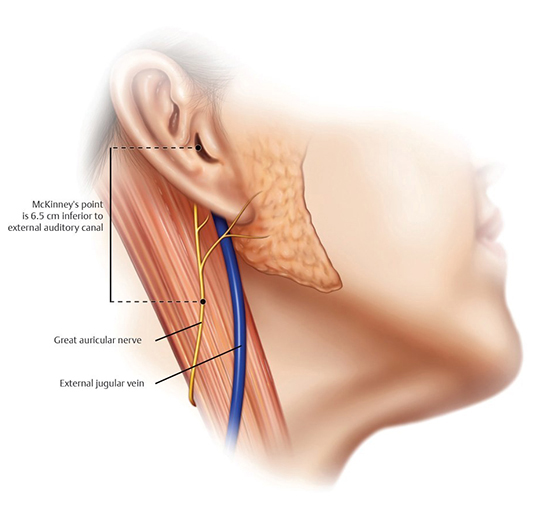
Figure 6. Great Auricular Nerve
Figure credit: Stuzin JM. Plastic Surgery Key. 2020 July. (https://plasticsurgerykey.com/7-great-auricular-nerve/)
Pre-procedure Evaluation
General assessment
A general clinical assessment should be performed of the patient’s skin quality, baseline volume status and notable soft tissue descent. It is often helpful to examine old photographs of the patient to determine anatomical baseline, which is ultimately what facelifting surgery aims to restore. The patient’s past medical history should be assessed to determine overall health status and anesthesia appropriateness. Medical history should be specifically reviewed for autoimmune or rheumatologic disease, vasculitis, uncontrolled hypertension (given increased risk of post-operative hematoma) and radiation exposure. Medications should be reviewed, with particular attention to blood thinning medications (including over-the-counter supplements), skin care regimen (including tretinoin, isotretinoin use), and immunosuppressive medication. Social history, including tobacco and alcohol use, should be assessed. The patient’s psychological stability and expectation appropriateness should also be evaluated.
Patients should be asked about prior facial surgical or procedural history, including prior incisional surgery, ultherapy, deoxycholic acid treatment, liposuction, thread lifting, chemodenervation, filler or autologous fat injection.
Facial asymmetries
The surgeon should make specific notice of underlying facial asymmetries, which should be documented, photographed and discussed with the patient. Surgical planning can often account for these asymmetries, with volume conservation or addition performed at varying degrees on each side. Asymmetries that cannot reasonably be remedied with surgery should be disclosed to the patients.
Prior surgery or incisions
Patients with a history of prior facelift surgery should have a thorough examination of previous incisions, including the location and quality of the resulting scar. Revision facelift can be performed along the same incision with prior scar excision or adjusted appropriately. Earlobe anatomy, including attached earlobe or iatrogenic pixie ear deformity may be augmented during time of surgery according to the patient’s wishes. It may be prudent to obtain operative reports from prior rhytidectomy surgery to understand the method and extent of prior dissection.
Incisional planning
Incisional planning should be performed at the preoperative appointment and described to the patient to align postoperative expectations. The vertical position of the patient’s sideburn should dictate the plan for a vertical intra-hairline incision vs. a transverse horizontal incision along the base of the sideburn. In the case of a high sideburn, a transverse incision should be preferentially considered so to not abnormally elevate the hairline during skin redraping. A low-to-normal sideburn allows for a vertical incision within the hairline to avoid visible incisional scar at the temple.
In the preauricular area, a post-tragal incision most often provides the optimally aesthetic incision line. A pre-tragal incision should used in male patients to avoid lateralization of bearded skin onto the tragus. In these cases, the pre-tragal incision can be designed with a non-linear contour to enhance the apparent visibility of the postoperative scar.
The patient’s post-auricular hairline should also be evaluated. A “short scar” approach may be considered in the setting of minimal neck skin laxity, which does not require substantial post-auricular incision. Full correction of excessive neck laxity may require extensive redraping and extended posterior incision for optimal improvement. The option of carrying the postauricular incision inferior to the hairline should be fully discussed and patient consent obtained. Patients with short hair, or with preference for updo hairstyles, may wish to avoid an extensive lateral neck incision at the expense of compromised skin redraping.
Surgical Techniques
Anesthesia and Positioning
Facelifting is generally performed under monitored intravenous sedation or general anesthesia with laryngeal mask airway (LMA) or endotracheal intubation. Judicious use of tumescent and full-strength local anesthetic solution acts as a vascular tourniquet, aiding in hemostasis and intraoperative visualization.
Intraoperative antibiotic and steroid administration is recommended. Patients should be positioned supine with padded support to the upper extremities to avoid ulnar or brachial radiculopathy. Deep vein thrombosis prophylaxis with sequential compressive devices or compression stockings is essential. Strict intraoperative blood pressure control and post-extubation emesis prophylaxis are critical to avoiding post-operative hematoma.
Subcutaneous facelift
The original facelifting techniques described by Bames in the early 1900s were limited to a subcutaneous flap elevation. The skin-only flap is performed in a plane deep to the subcutaneous fat with preservation of the subdermal plexus to allow for adequate flap vascularity. This flap is best performed with use of a blade (#15 or #10) or sharp dissection scissors, using counter traction and transillumination.
Exclusive use of this skin-only flap technique led to the stereotypical “wind swept” appearance and flattened facial contour that predominated the post-operative outcomes of the mid-1900s. This technique is less commonly utilized in isolation today, replaced by concurrent SMAS manipulation to provide more effective and enduring soft tissue lift and minimize skin flap tension, which may lead to widely spread and mal-appearing scars. The subcutaneous facelift can still be beneficial rarely in cases of revision rhytidectomy with residual skin excess, or in setting of connective tissue disease where skin laxity is the predominating pathology.
SMAS Plication (MACS lift)
SMAS manipulation has become the primary mechanism for repositioning of ptotic facial soft tissues. Elevation of this inelastic tissue layer allows for more direct correction of deep soft tissue descent. Suture plication of the SMAS following subcutaneous dissection may be performed as a minimally invasive, low risk and technically straightforward technique. The minimal access cranial suspension (MACS) lift, first described by Tonnard et al., involves 2-3 purse-string sutures woven along the lower and mid-face SMAS (Figure 7), anchored to the deep temporalis fascia above the zygomatic arch. In their original technique, the authors utilized a 1-0 PDS suture to take progressive 1-cm long bites through the SMAS along the desired trajectory to provide this elevation. This procedure may be performed through limited preauricular and temple incisions. A subcutaneous flap can subsequently be redraped vertically and trimmed. This technique is most appropriate for patients with mild gravitational descent and without desire for surgical neck recontouring. Downsides of this technique include lateralization of facial volume, and visible irregularity of SMAS contour.
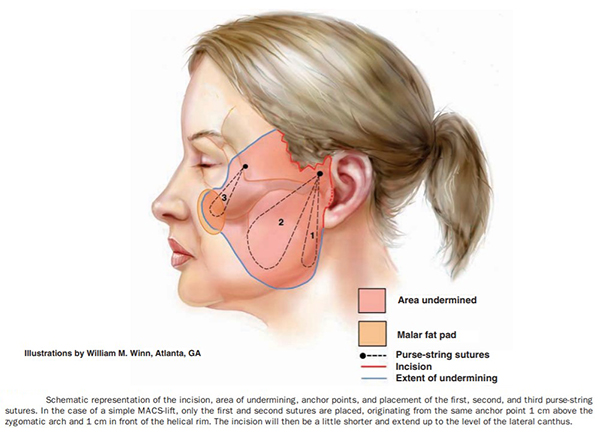
Figure 7. MACS Lift
Figure credit: Tonnard P, Verpaele A. The MACS-lift short scar rhytidectomy. Aesthet Surg J. 2007 Mar-Apr;27(2):188-98. doi: 10.1016/j.asj.2007.01.008. PMID: 19341646.
SMAS Imbrication or Excision
Lateral SMAS excision, or “SMASectomy”, was popularized by Dr. Daniel Baker in 1992. This technique similarly begins with an extended subcutaneous dissection, followed by excision of a 2-3 cm strip of SMAS along a line extending from the lateral malar eminence toward the tail of the parotid gland (Figure 8, Baker). This technique can be performed with or without preceding neck and jowl liposuction. The cut edges of SMAS are then reapproximated, immobile lateral edge to mobile anterior edge. The benefit of this technique includes lateralization of the mobile thin medial SMAS without requiring sub-SMAS dissection in that area, minimizing risk of morbidity and SMAS injury. This technique was later refined in 2001 to become known as the minimal incision rhytidectomy.
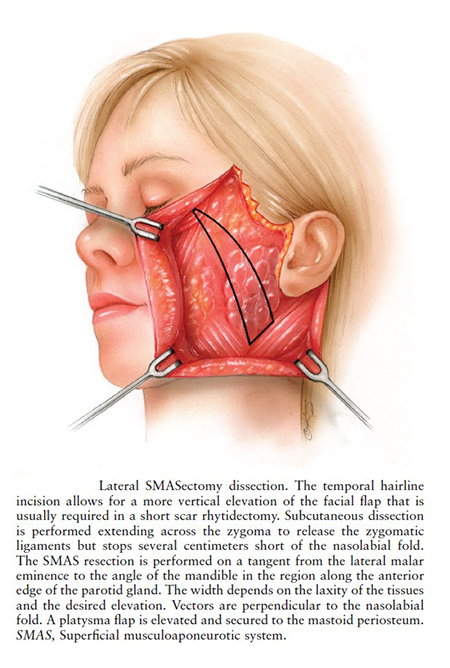
Figure 8. Lateral SMASectomy Facelift Technique
Figure credit: Baker DC, Levine SM. Chapter 18: Lateral SMASectomy Facelift. Master Techniques in Facial Rejuvenation.
Deep Plane Facelift
As early as the 1970s, a deep sub-SMAS dissection technique, with lateral SMAS dissection overlying the parotid gland was popularized (Figure 9). Dr. Skoog proposed lifting of a single flap containing skin, subcutaneous fat and SMAS (Skoog). In subsequent years, further refined techniques involved separate subcutaneous and SMAS flaps, with extension of the sub-SMAS dissection anterior to the parotid gland to more effectively efface the jowl and contour the lower face via ligament release and robust tissue mobilization. This technique requires complete release of the zygomatic, masseteric and mandibular osteocutaneous ligaments for maximal long-lasting SMAS elevation and effacement of the nasolabial folds and jowls. This sub-SMAS flap can be initiated either laterally over the immobile SMAS or anteriorly over mobile SMAS. These authors prefer to begin this dissection with paddle-tip cautery in the preauricular area over the parotid gland where the facial nerve is protected by deep fascial and glandular tissue. The dissection is continued anteriorly along the anterior surface of the masseteric fascia, under which the facial nerve branches lie. Operative staff should observe closely for muscle twitching, as this indicates cautery stimulation of a nearby facial nerve branch. The SMAS flap may be continued above the zygomatic arch in a “high SMAS” technique to provide improved mobilization of midface soft tissues compared to the “low SMAS” technique which truncates this flap below the zygomatic arch.
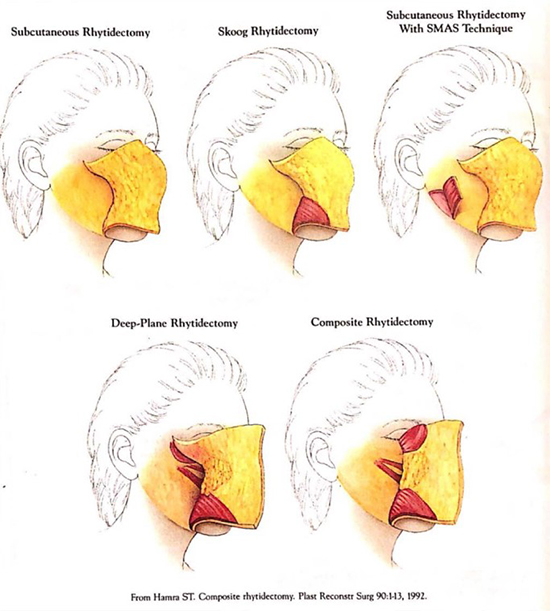
Figure 9. Facelifting Techniques
Figure credit: Hamra ST. Composite rhytidectomy. Plast Reconstr Surg. 1992;90:1-13.
Once fully released from ligamentous attachments, the SMAS can be redraped in a primarily vertical vector and fixated to the deep temporalis fascia. If simultaneous neck lifting is performed, the sub-SMAS flap is connected with the previously developed sub-platysmal flap. A portion of the neck flap may be draped in a posterior direction and secured to deep cervical fascia in the post-auricular region to optimize definition of the mandibular border.
The subcutaneous flap is then separately redraped in a superolateral vector, able to be closed with minimal tension using deep buried and superficial sutures.
Composite Facelift
Hamra et al. described the composite facelift technique, in which a deep plane dissection was continued posterior to the orbicularis oculi for simultaneous resuspension of the infraorbital soft tissues (Figure 9). A composite flap comprised of SMAS, malar fat and orbicularis oculi muscle is then elevated for comprehensive facial rejuvenation. These authors are less favorable toward this technique given risk of orbicularis oculi denervation with lateral orbicularis incision and sub-muscular dissection.
Subperiosteal Facelift
A subperiosteal facelift, or “mask-lift” was proposed by Tessier in 1989, to be performed either via a bicoronal or vestibular incisions, allowing for elevation primarily of the upper two-thirds of the face, including the frontal, maxillary, malar, zygomatic and orbital regions. The lower 1/3rd of the face was simultaneously addressed from a deep plane sub-SMAS approach. This approach gained popularity with the invent of endoscopes, allowing for short incisions in the temple and buccal sulcus. This technique works well for midface elevation, maintaining a plane deep to the facial nerve, but has limited use in the lower face and neck regions. Simultaneous subperiosteal upper face release enhances release of the midfacial ligaments, facilitating more complete mobilization of the lower face during concurrent deep plane rhytidectomy.
Post-Operative Management
Compressive dressing
A compressive dressing should be placed immediately post-operatively. This may be comprised of Kerlix, secured with an encircling Coband wrap, or with a pre-fashioned compression head wrap. The periauricular incisions should be protected with drain sponge or Telfa prior to head dressing placement. This dressing should remain in place until post-operative day 1, at which time the patient should begin to wear a soft circumferential neck wrap for prevention of seroma formation in the gravity dependent regions. These authors instruct patients to this wrap full-time for the first post-operative week, and at bedtime-only for the second post-operative week. It is important that the patient take short breaks in compressive wrap wear and avoid overtightening to prevent flap ischemia.
Drain management
A Jackson Pratt (JP) drain should be inserted bilaterally at time of surgery and secured to the patient’s post-auricular area to remain in place overnight. If no evidence of accumulated hematoma or seroma, these drains can be removed on post-operative day 1. If excessive edema or fluctuance is noted, the drains should be left in place and checked for proper aspiration. Malfunctioning drains may need to be replaced with a subsequent JP or suction drain. These patients should be placed on oral antibiotics and monitored daily for improvement.
Post-operative evaluations
In the setting of routine healing, the patient should be examined a minimum of day 1, day 7 and month 1 following rhytidectomy. Simultaneous treatment with skin resurfacing, or any evidence of complications, may mandate closer follow-up.
Complications
Hematoma
Hematoma is the most common early post-operative complication of rhytidectomy, occurring in 3-8% of cases, and typically presenting within the first 24 hours following surgery. Risk factors for hematoma formation include male gender, labile intraoperative blood pressure, as well as post-operative emesis, coughing, agitation or poorly-controlled pain. Holding of medications with anti-platelet and anti-coagulant properties, including herbal supplements, during the perioperative period is essential. Patients should adhere to their routine blood pressure medication regimens, including on the morning of surgery. Patients should be counseled on signs and symptoms of hematoma, as immediate evacuation is necessary to prevent flap ischemia. Patients with indwelling drain should be checked for drain function and output. Signs of actively expanding hematoma despite compression in the setting of a functioning drain may require surgical exploration.
Seroma
Seroma accumulation most commonly occurs 5-7 days after surgery. Patients typically present with painless fluid collection beneath the flap, often in gravity-dependent areas. Seroma prevention includes judicious use of compressive dressing in the initial post-operative period. Fibrin glue has been tested for improved flap adherence with mixed success.
Seroma formation should similarly prompt immediate evacuation with needle aspiration. These authors recommend low threshold for placement of a suction catheter (e.g. SeromaCath) if more than a minimal amount of fluid is detected on aspiration. Any symptoms concerning for infection, including pain, erythema or warmth at the site of fluid collection, or systemic infectious symptoms, should prompt microbiological analysis of aspirated fluid and empiric treatment with oral antibiotics.
Facial nerve injury
Facial nerve injury remains the most feared complication of rhytidectomy, with reported incidence of 0.3-2.6%. It is important to note that transient facial nerve weakness is expected in the immediate post-operative period during which the local anesthetic remains active. Longer-lasting motor deficit may result from nerve trauma by cautery, excessive retraction or suture placement, anticipated to improve. The buccal nerve branches are most commonly injured during facelifting surgery, though rarely result in permanent paresis given their extensive arborization. The most common motor deficits following facelifting surgery result from injury to the marginal mandibular branches.
Nerve transection observed intraoperatively should be repaired with suture anastomosis of the perineural sheath. Mild motor deficits noticed post-operatively can be treated with chemodenervation to the contralateral side. Fortunately, most motor nerve deficits noticed during the early post-operative period will recover with watchful waiting over 3-4 months time.
Great auricular nerve injury
Even without injury to the great auricular nerve, sensory hypoesthesia across the area of the subcutaneous flap due to transection of minor branches of the nerve is common after rhytidectomy surgery, and typically resolves within 12 months. The great auricular nerve is the most commonly injured nerve during rhytidectomy. As this nerve provides sensory innervation to the lower ear, parotid and mastoid areas, damage may result in hypoesthesia, paresthesia or painful neuroma in those regions. The nerve is particularly vulnerable to injury during postauricular sub-SMAS dissection and during subplatysmal liposuction or fat excision. Careful avoidance of deep cervical fascial violation can minimize risk of injury. Transection noted intraoperatively should be repaired with end-to-end anastamosis, usually with good outcome.
Vessel injury
The external jugular vein travels just medial to the great auricular nerve and can sustain damage if not carefully avoided. Injury to the external jugular vein requires suture ligation for hemostasis. Overcautery of subcutaneous vascular supply during surgery can produce vascular compromise to the edges of the skin flap, producing tissue ischemia and poor healing.
Parotid gland or duct injury
Parotid gland parenchymal injury may occur during sub-SMAS dissection, and may lead to post-operative sialocele or fistula formation if not properly addressed. When parenchymal injury is identified intraoperatively, cauterization should be performed to seal gland ductules. Post-operative identification of pre-parotid fluid collection should prompt drainage and testing of fluid for amylase to confirm sialocele. Treatment with pressure dressing, anticholinergic agent (e.g. glycopyrrolate), intraglandular chemodenervation, transdermal scopolamine and bland diet should be initiated. Persistent salivary collection or fistula not improved with closed-suction drain may require surgical repair.
Parotid duct injury may occur during sub-SMAS dissection, with the duct traveling along the anterior border of the masseter along a trajectory estimated by a line drawn from the external auditory canal to the upper lip. Direct duct injury identified intraoperatively should be treated with retrograde cannulation with catheter placement.
Skin flap necrosis
Skin flap necrosis occurs most commonly following extensive subcutaneous dissection. Other risk factors for flap ischemia include untreated sub-flap hematoma or seroma, excessively thin flap with injury to the subdermal plexus or aggressive laser resurfacing over the flap. Closure of incisions with excessive tension also increases risk of incision-line necrosis. Tobacco use has been found to increase risk of post-surgical necrosis 10-12 fold. Evidence of necrosis may be treated conservatively with topical nitropaste and local wound care. Hyperbaric oxygen should be considered where available. While controversial, serial debridement may be considered in cases of extensive eschar for infection mitigation. The patient should be counseled on future treatment with options with topical and injected steroid and antimetabolite use, skin resurfacing, flap repair and grafting to optimize final healing.
Scar
Hypertrophic scar formation most commonly forms from excessive wound closure tension or incision necrosis. Patients should be evaluated pre-operatively for tendency to form keloid or hypertrophic scarring, which may be a contraindication for facelifting surgery. Hypertrophic and keloid scars should be treated judiciously with steroid and anti-metabolite injection and/or microneedling during the post-operative period.
Pixie ear
Pixie ear deformity occurs from overzealous resection of inferior auricular skin and/or inadequate deep fixation of the skin flaps, inducing downward traction on the earlobe over time. The periauricular incision design should include a preserved bridge of skin below the earlobe attachment point to prevent this deformity.
Alopecia
Hair loss may occur in up to 8% of rhytidectomies from follicle damage related to electrocautery use, direct follicle transection or skin ischemia from excessive skin flap tension. Beveling of incisions within the hairline aids in follicle preservation. Telogen effluvium, or stress-related hair loss, can also occur in the post-rhytidectomy period, with hair regrowth delayed for 4-6 months post-operatively. Telogen effluvium can be treated with intradermal corticosteroid injection and topical bimatoprost. Hair loss lasting beyond 12 months post-surgery may benefit from micrografting.
Infection
While infection is rare following rhytidectomy, prolonged untreated hematoma, seroma or skin necrosis may increase risk for infection. Routine intraoperative prophylactic administration of antibiotics with activity against Staphylococcus aureus and epidermids species is recommended. Delayed infection may indicate atypical mycobacterial infection, which often requires biopsy confirmation and macrolide antibiotics.
Frey Syndrome
Frey syndrome, or gustatory sweating, may occur from injury to the auriculotemporal nerve branch of the mandibular (V3) nerve overlying the parotid gland, allowing for aberrant regeneration of postganglionic parasympathetic nerves normally inducing salivation, to innervate cutaneous sweat glands. These patients demonstrate hyperhidrosis of the lateral face with anticipation of food intake. Anticholinergic agents and chemodenervation may be used as treatments.
Contour deformities
Contour deformities tend to occur at areas of SMAS plication or suturing. The deep plane layer should be examined for contour irregularities at time of surgery, prior to skin redraping, and any visible irregularities addressed. Contour depressions related to suture placement can be anticipated to improve with time. Sustained volume irregularities may be treated with autologous fat or filler.
Depression
Post-surgical clinical depression is an underrecognized adverse event complication following cosmetic surgery. Patients should be warned about the common feeling of “buyer’s remorse” and evaluated post-operatively for changes in mood. Some patients may benefit from psychological counseling and/or pharmacotherapy prior to or following surgery.
Historical Perspective, References and Additional Resources
- Baker DC. Lateral SMASectomy. Plast Reconstr Surg. 1997;100(2):509–13.
Mendelson B, Wong C. Chapter 6.1: Facelift: Facial anatomy and aging. Aesthetic Surgery of the Face. 2012.
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plast Reconstr Surg. 1966 Oct; 38(4):352-6. - Skoog. Plastic Surgery: New Methods and Refinements. Philadelphia: Saunders;1974.
- Tessier P. Le lifting facial sous-périosté [Subperiosteal face-lift]. Ann Chir Plast Esthet. 1989;34(3):193-7. French.
- Tonnard P, Verpaele A. The MACS-lift short scar rhytidectomy. Aesthet Surg J. 2007 Mar-Apr;27(2):188-98. doi: 10.1016/j.asj.2007.01.008. PMID: 19341646.
- Wan D, Amirlak B, Giessler P, et al. The differeing adipocyte morphologies of deep versus superficial midfacial fat compartments: A cadaveric study. Plast Reconstr Surg. 2014;133:615e-622e.
- Wan D, Small KH, Barton FE. Face Lift. Plast Reconstr Surg. 2015 Nov;136(5):676e-689e.
- Warren RJ, Aston SJ, Mendelson BC. Face Lift. Plast Reconstr Surg. 2011 Dec;128(6):747e-764e.
