Trichiasis
Updated May 2024
Eyelashes
Embryologically lash follicles and cilia arise from ingrowth of surface ectoderm.
Eyelashes emerge from the lid margin anterior to the gray line.
- The hair bulbs of the lashes are anterior to the tarsus (Figure 1).
- Eyelashes form 2 or 3 irregular rows along the anterior dermal edge of the eyelid margin.
- They protect the ocular surface by filtering small particles and functioning as sensors to stimulate reflex eyelid closure.
- Eyelashes are usually longer and more numerous on the upper lid than the lower (about 100 in upper lid and 50 in lower lid).
- Glands of Zeis (modified sebaceous glands) are associated with lashes.
- A few eyelashes can be found on the caruncle.
- Lashes are replaced every 3–5 months.
- They regrow in about 2 weeks if cut and within 2 months if epilated.
Eyelash enhancement:
- Prostaglandin F2a (PGF2a) analogs enhance the number, length, and thickness of lashes.
- They are available in the same formulation as glaucoma drops (bimatoprost 0.03%).
- Can cause periorbital fat atrophy, eyelid margin hyperemia and eyelid hyperpigmentation
- These changes often reverse if the drug is stopped for several months, but can be permanent.
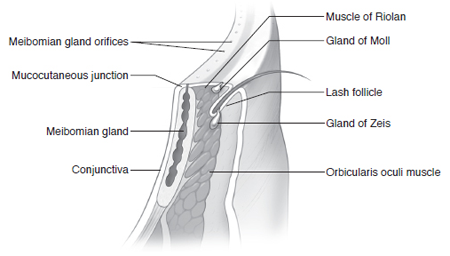
Figure 1. Eyelid margin anatomy.
Establishing the diagnosis
Etiology
Trichiasis refers to an abnormal misdirection of lashes, often turning inward against the eye, in the absence of entropion (Figure 2).
- Cicatricial lash problems generally arise from acute or chronic inflammation
- Most common acute causes
- Viral infection (herpes zoster, herpes simplex, vaccinia)
- Chemical burns, especially alkali
- Trauma
- Radiation
- Surgery
- Cryotherapy
- Most common chronic causes
- Blepharitis (Staphylococcus, seborrhea, rosacea, etc.)
- Trachoma
- Chronic viral infection
- Conjunctival shrinkage (pemphigoid, Stevens-Johnson syndrome)
- Topical medications
- Idiopathic inflammation
- Establishing the correct diagnosis is important and may affect prognosis and therapy
- If untreated, pemphigoid can lead to blindness.
- Unless patients are treated with immunesuppressants, pemphigoid can worsen with surgical insult.
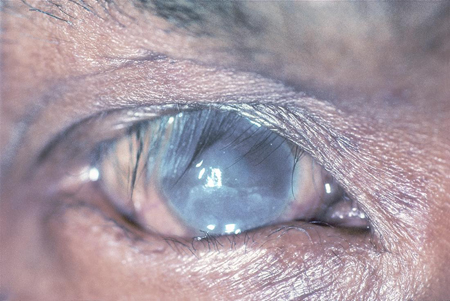
Figure 2. Trichiasis. Image courtesy Thomas M. Lietman, MD.
History
- Duration of symptoms
- Presence of oral or skin lesions or herpetic outbreaks
- Previous lash removal treatments
- Previous eyelid trauma or surgery
- Foreign travel or residence
- History of radiation treatment to periocular area
- Current or prior use of glaucoma or other eyedrops
- Use of cosmetic eyelash enhancing preparations
Clinical features
- Inward directed lashes: Note location and extent of misdirected lashes.
- Note mild in-turning of eyelid margin.
- Tarsal fibrosis or cicatrized conjunctiva
- Evidence of prior trauma or surgery
- Document related corneal changes.
- Eyelid lesions distorting lash orientation
Testing
- Cultures can be useful for infectious processes.
- Conjunctival biopsy with basement membrane studies for mucous membrane pemphigoid
Differential diagnosis
- Marginal or cicatricial entropion with subtle posterior lamellar scarring inverting the margin slightly
- Entropion: Various forms are discussed elsewhere.
- Aberrant lashes: normal position, abnormal direction
- Distichiasis: lashes growing posterior to the normal lash line, typically arising from Meibomian gland orifices (Figure 3)
- Uncommon, congenital condition
- Sporadic or autosomal dominant with variable penetrance
- Embryonic pilosebaceous units develop into hair follicles
- Metaplastic lashes: lashes growing from abnormal position
- Acquired distichiasis in the setting of chronic inflammation
- Metaplastic transformation of Meibomian glands due to chemical, physical or immunologic stimuli
- Epiblepharon (Figure 4)
- Lanugo hairs: Previous surgery (e.g., Hughes tarsoconjunctival flap) or trauma can alter eyelid margin so adjacent skin hair is in contact with the cornea.
- The term actually refers to fine, soft, nonpigmented hair on fetal or newborn skin.
- Clinically used to describe fine hair in contact with the cornea

Figure 3. Distichiasis. Image courtesy Jill Foster, MD.
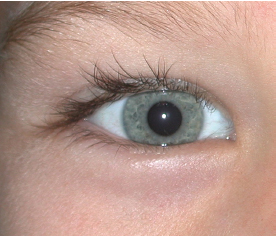
Figure 4. Epiblepharon. Image courtesy Jill Foster, MD.
Management
Indications
- Abnormal eyelash growth (trichiasis) or location (distichiasis) with subsequent ocular surface irritation or breakdown
Preprocedure evaluation
- Complete ophthalmic examination
- Main exam area focuses on location and type of abnormal eyelash growth.
- If the involved region is localized, consider surgical excision.
- If diffuse isolated misdirected lashes, consider electroepilation.
Medical therapy
- Ocular lubrication
- Bandage contact lens
Surgery
- Appropriate entropion procedures if present
- Manual epilation of affected lashes
- Some patients prefer repeat epilation as a reasonable option.
- Minimally invasive, but requires frequent office visits
- Some find this initiates a cycle of accelerated lash growth.
- Permanent epilation by electrolysis/ hyfrecation/radiofrequency ablation
- Cryotherapy
- Laser ablation
- Surgical dissection and excision (horizontal lid splitting and lash bulb excision)
- Block (full thickness block) resection and eyelid margin repair for recalcitrant cases
- Choice depends on etiology, extent of abnormality, location of misdirected lashes, and patient preference.
Techniques
Radiofrequency, hyfrecation, electroepilation
- Performed with operating microscope or at the slit lamp
- Injection of local anesthetic and topical ophthalmic anesthetic drop
- Extremely fine wire-tip electrode or partially insulated needle-tip inserted in hair shaft
- The Ellman Surgitron unit can be used (Hurwitz, Can J Ophthalmol, 1993).
- Converts electrical current into controlled energy in the radiowave portion of the electromagnetic spectrum at 3.8 MHz with less collateral tissue damage than bovie electrosurgery units that operate at 0.5 MHz.
- Needle insertion parallel to direction of the abnormal eyelash
- Depth should be approximately 2–3 mm.
- Current is applied until a bubbling is noted at the follicle orifice.
- With the Ellman, start with initial settings of 4 or cut or coag and adjust upward to maximum of 8.
- The abnormal lash should come out attached to the needle or be removed easily with forceps.
- Each aberrant eyelash is treated separately
- If needed, treatment can be repeated in several weeks
- Post treatment combination drops or ointment are optional
- Advantages
- Selectively destroys lash follicles without significant surrounding tissue damage
- Office procedure can be repeated as needed.
- Disadvantages
- Equipment needs (radiofrequency or similar unit)
- Extensive treatment can cause lid margin scarring
- Recurrences are common and retreatment is often needed.
Argon laser ablation
- The accuracy of the laser in theory should allow destruction of the follicle with minimal surrounding tissue damage compared with cryotherapy or electroepilation.
- Mechanism of action is focal tissue coagulation of the targeted follicle.
- Injection of local anesthetic and topical anesthetic drop
- Patient is positioned in an argon laser headrest.
- A laser-safe corneal protective shield is used.
- The eyelid is everted and the argon laser is positioned so that the aiming beam will parallel the direction of the abnormal eyelash.
- Spot size is set at 100–200 microns.
- Pulse duration is 0.5 seconds or longer.
- The lowest effective power settings are applied, about 1 watt.
- Repeat pulses are applied until the laser has ablated to a depth of 2–3 mm.
- Post-treatment combination drops or ointment are optional.
- Advantage
- Selective lashes can be targeted.
- Disadvantages
- Dimpling of lid margin
- Recurrence
- Hypopigmentation of skin
- Risk of laser damage to eye
Cryoepilation
- Cryotherapy kills by causing intracellular ice crystal formation.
- Lash follicles appear more sensitive than others cells in the lid.
- Corneal protective shield is used to avoid damage to the globe.
- Injection of local anesthetic and topical anesthetic drop
- Cryotherapy probe is applied to the affected area with a “double freeze-thaw” technique.
- This therapy is more appropriate for an area of focal trichiasis.
- The probe is left on for 20–40 seconds, the lid margin is allowed to thaw, then the probe is reapplied for another 20–40 seconds.
- A thermocouple can be used to monitor temperature, but might be unwieldy in this anatomic area.
- The desired temperature is about -20 C.
- Applications are made in an overlapping manner.
- Lashes should be easily removed with forceps after the procedure.
- Post-treatment combination drops or ointment are optional.
- Advantages
- Relatively large areas can be treated quickly.
- Small lashes that are difficult to isolate often respond well.
- Procedure can be repeated as necessary.
- Disadvantages
- Cryotherapy can incite a moderately severe inflammatory response.
- Can cause hypopigmentation (dermal melanocytes die at temperatures around -15 C) and lid margin scarring.
- It is difficult to spare normal lashes.
Surgical management
- Full-thickness wedge resection is indicated for focal areas of trichiasis/distichiasis.
- Advantage: completely eliminates focal area of aberrant follicles
- Disadvantages:
- More invasive than nonsurgical procedures
- Can result in visible eyelid scarring
- Lid-splitting is indicated for more diffuse areas of trichiasis/distichiasis.
- Local anesthetic is injected
- Blade incision to divide the grey line for 2 mm.
- Anterior lamella with skin, muscle, and lashes
- Posterior lamella with tarsus and conjunctiva
- Scissors to continue dissection to distal edge of tarsus
- Hemostasis with minimal cautery
- Involved lashes can be treated with any of the above destructive procedures (cryotherapy, etc.) or in refractory cases the involved lashes can be directly excised
- Double armed sutures are then passed from the anterior tarsal surface through the skin and tied over bolsters positioning the anterior lamella 2mm below (in lower lid cases) the posterior lamella
- The 2-mm “gap” will re-epithelialize during the healing process
- Standard post-operative care (ice packs, antibiotic ointment, etc.) should be employed
- Advantages:
- Addresses broad area of aberrant eyelashes
- Good choice for complex situations such as trachoma
- Disadvantages:
- More invasive than nonsurgical options
- Results in change in appearance of eyelid margins
- Tarsal fracture — lid everting procedure
- Most commonly used is the Weis procedure (transverse blepharotomy with margin rotation).
- Local anesthetic is injected.
- Horizontal full-thickness incision is made about 3 mm from the lid margin, extending from just lateral to the punctum to the lateral canthus.
- 4–5 double-armed 6-0 absorbable sutures are placed to rotate the lid margin outward.
- The sutures are started in the stable tarsal edge and are passed anterior to the anterior surface of the cut tarsus.
- They exit the skin just proximal to the lashes.
- Initial overcorrection is desirable.
- Advantages:
- Addresses entire extent of eyelid margin
- Good for patients with more extensive problems
- Disadvantages:
- More invasive than nonsurgical options
- Can cause change in eyelid appearance
- Eyelash extirpation with mucous membrane grafting
- A good option in severe or recurrent cases or when there this is accompanying keratinization of the lid margin (Stevens-Johnson syndrome, pemphigoid)
- Local anesthetic is injected.
- The lid margin is removed as a strip with enough depth to include the lash follicles.
- A full-thickness mucosal graft is harvested from inside the lip and thinned.
- The graft is sutured into position along the eyelid margin, extending anteriorly enough to allow for graft shrinkage and retraction.
- Advantages:
- Recurrence of trichiasis is rare.
- Other lid margin pathology such as keratinization is also addressed.
- Disadvantages:
- More invasive procedure with donor site morbidity
- Can result in loss of lid substance and eyelid retraction
- Results in change in eyelid appearance
Preventing and managing treatment complications
Radiofrequency, argon, cryotherapy
- Main complication is recurrence — as high as 50%.
- Most patients will require retreatment after 4 weeks.
- Infection
- Bleeding
- Eyelid irregularities
- Entropion
- Corneal abrasion
- Corneal burn
- Globe perforation
- Eyelid necrosis
Surgical excision
- Bleeding
- Infection
- Corneal abrasion
- Eyelid irregularities
- Entropion
- Globe perforation
- Scarring
Follow-up care
Radiofrequency, argon, cryotherapy
- Patients not previously treated can be seen in 1 week.
- Patients familiar with the procedure can be seen in 4-5 weeks for possible retreatment.
- Standard postoperative care (ice packs, antibiotic ointment, etc.) should be employed.
Surgical excision
- Standard postoperative care (ice packs, antibiotic ointment, etc.) should be employed.
- Patients are seen 1 week postoperatively.
- Lid margin sutures, when present, should be removed no sooner than day 10.
- A final postoperative visit can be scheduled between month 2 and 3.
References and additional resources
- AAO, Basic and Clinical Sciences Course. Section 7: Orbit, Eyelids, and Lacrimal System, 2013-2014.
- AAO, Surgery of the Eyelid, Orbit & Lacrimal system, Vol. 1, 1993, p.128, 139-140.
- AAO, Surgery of the Eyelid, Orbit & Lacrimal system, Vol. 2, 1994, p.50-52.
- AAO, Focal Points: Management of Trichiasis, Module #4, 2001.
- AAO, Focal Points: Management of Cicatricial Entropion, Trichiasis and Distichiasis Module #12, 1993.
- Hurwitz JJ et al. Experimental treatment of eyelashes with high-frequency radio wave electrosurgery. Can J Ophthalmol 1993;28:62-4.
- Hurwitz JJ et al. High-frequency radio wave electrosection of full-thickness eyelid tissues. Can J Ophthalmol 1993; 28:28-31.
- Thome JE, Anhalt GJ, Jabs DA. Mucous membrane pemphigoid and pseudopemphigoid. Ophthalmology. 2004;111:45-52.
- Wojno, TH. Lid splitting with lash resection for cicatricial entropion and trichiasis. Ophthal Plast Reconstr Surg. 1992;8(4):287-9.
